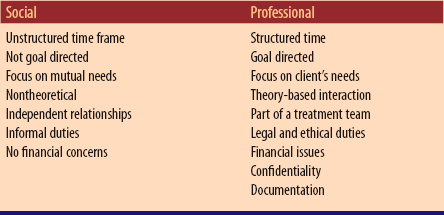
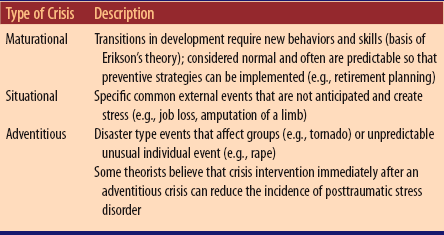
Chapter 16 A A fundamental component of psychiatric nursing is to understand the legal framework used to regulate the care and treatment of clients with mental illness; each state has its own mental health code that delineates the law in this area; therefore, the mental health laws vary from state to state; case law may also set precedents that guide care B Adherence to the Patient Care Partnership (formerly The Patient’s Bill of Rights) is essential C All civil rights are maintained D Clients have the right to be treated in the least restrictive environment; any curtailment of autonomy must be substantiated by documentation supporting the need to limit the client’s freedom; clients retain the right to a lawyer and the right to request a court hearing; clients may execute a psychiatric advance directive stating treatment preferences E Types of hospital admissions 1. Voluntary admission: clients of lawful age may apply in writing to be admitted for treatment to a mental health facility; written notice of intent to leave may be required with a waiting period during which the health care provider may choose to change admission status to involuntary 2. Involuntary admission (commitment): clients who have not agreed to treatment are placed in a mental health facility; criteria for involuntary admission in some states are very circumscribed (danger to self or others); in other states requirements are more liberal (mentally ill and in need of treatment, gravely disabled, and/or unable to provide for own basic needs); most states have various routes for involuntary admission that may include a. Emergency hospitalization: used to intervene when there is an immediate threat by a client to self or others; this short-term (48 to 72 hours) commitment is allowed for the assessment of the client and to determine if more long-term commitment is needed or the client can be discharged to outpatient treatment b. Court ordered observational admission: used to assess the mental status of a person in relation to legal activities (e.g., competency to stand trial) c. Formal commitment: used to treat clients with chronic mental illnesses over a prolonged period; periodic reviews may be made at 3, 6, or 12 months d. Two health care provider commitment: two health care providers document that the client has met the state’s criteria for involuntary care; most states provide for an intermediate length of time (1 to 6 weeks) admission e. Physician’s Emergency Certificate: allows the facility to keep people against their will F Seclusion and restraint: a client who is a threat to self or others may be placed in a seclusion room or in four-point restraints to prevent injury or harm 1. A health care provider must give an order for seclusion or restraint for each incident and renew it every few hours as determined by state mental health law; prn seclusion and restraint orders are not acceptable 2. The nurse must document the initial and continued need for seclusion or restraints; the client must be observed constantly if in restraints and checked every 15 minutes if in seclusion; hourly physical assessment must be performed if the client’s condition permits 3. Hydration, nutrition, and elimination needs must be met while the client is in seclusion or restraints 4. When it is determined that the client is no longer a threat to self or others, the client must be released from seclusion or restraints 5. Chemical restraint: the nurse may administer a prescribed prn medication without the client’s consent if the client is dangerous to self or others G Court-ordered medication: a client’s right to refuse treatment may be overruled, and the client may be court mandated to take medication to decrease the threat of injury to self or others H Psychiatric advance directive: a client with a recurrent/chronic psychiatric disorder may establish an advance directive to guide treatment during a future episode of mental illness when judgment is impaired A Implement care that meets the Scope and Standard of Psychiatric-Mental Health Clinical Nursing Practice as described by the American Nurses Association (ANA) and nursing practice laws of the state where practicing (e.g., health promotion, case management, treatment of human responses) B Remain current with skills and knowledge base C Keep accurate and concise client records D Maintain client/family confidentiality; an exception must be made to notify others (e.g., police, intended victim) if a credible threat against another person is made by the client E Know the laws governing practice within the state, the rights and duties of the nurse, and the rights of the client 1. Provide prevention, treatment, and rehabilitation services for individuals with emotional problems; also support for families 2. Maintain individuals and families in the community 3. Provide hospital care within the community in those instances when the individual cannot be maintained on an outpatient basis 4. Emphasize managed care mandates that shift care from costly inpatient treatment to community and home health visits B Types of settings in which services are provided a. Storefront clinics, daycare centers, mobile units, intensive outpatient programs, partial hospitalization programs, or day treatment centers b. Walk-in clinics in hospitals and psychiatric emergency departments d. Crisis intervention centers, mobile crisis units, hot-line phone centers and the Internet e. Private community practice, schools, and shelters f. Dual-diagnoses programs (mental health and chemical dependency) a. Specialized psychiatric hospitals, both long-term and short-term care b. General hospital psychiatric units c. Short-term placement; provide respite for caregivers, provide safe environment during episodes of aggressive acting-out 1. Observation, diagnosis, and determination of client needs 3. Direct care services to clients, including a. Supports the individual during the period of crisis b. Helps the individual learn new ways of coping with problems 5. Referral to other community agencies for necessary services 8. Education for professionals and consumers of mental health care B Assessment of the individual’s needs C Establishment of the therapeutic milieu D Consultation and collaboration with other professionals including the interdisciplinary team: health care providers (e.g., physicians, psychologists, advanced practice nurses, physicians assistants), social workers, school teachers, clergy, nursing home and managed adult residential facility staff E Active participation with the health team, including the individual and family F Involvement in individual, family, and group therapy G Supervision of licensed and unlicensed staff members H Coordination of health services for the individual and family; referral and preparation of client for scheduled appointments I Education of groups within the community J Function as client advocate including seeking health insurance parity for reimbursement of costs for psychiatric treatment K Advanced practice nurses may prescribe medication in some states A Phases of a therapeutic nurse-client relationship (see The Nurse-Client Relationship under Communication in Chapter 2) B Themes of communication (see The Communication Process under Communication in Chapter 2) C Therapeutic communication requires a basic understanding and use of interviewing techniques (see The Nurse-Client Relationship under Communication in Chapter 2) D Issues that interfere with a therapeutic relationship during the working phase of a therapeutic relationship 1. Transference: the client superimposes feelings from other relationships onto the nurse-client relationship (e.g., client gets angry easily at nurse who resembles a former significant other with whom the client had a contentious relationship) 2. Countertransference: the nurse superimposes feelings from other relationships onto the nurse-client relationship (e.g., older nurse treats a younger client like a son or daughter) 3. Resistance: client fails to engage in or sabotages treatment (e.g., forgets appointments, keeps changing subject) 4. Blurring of a professional versus a social relationship (see Table 16-1: Differences Between a Social and a Professional Relationship) A Help people to prevent mental health problems and assist clients to cope with mental health problems B Accept and respect people as individuals and strive to separate the person from behavior that may be dysfunctional C Reorient client to person, place, time, and situation D Limit or reject inappropriate behavior without rejecting the individual E Help individuals set appropriate limits for themselves or set limits for them when they are unable to do so F Recognize that all behavior has meaning and is meeting the needs of the person performing it, regardless of how distorted or meaningless it appears to others G Accept the dependency needs of individuals while supporting and encouraging moves toward independence; build on ego strengths H Create a nonjudgmental environment that encourages individuals to express their feelings I Recognize that individuals need to use their dysfunctional defenses until other healthier defenses can be substituted J Recognize how feelings, behavior, and thoughts are interactive and influence relationships K Recognize that individuals frequently respond to the behavioral expectations of others: family, peers, and authority figures (e.g., health team members) L Recognize that all individuals have a potential for movement toward higher levels of emotional health M Include family members in the health care team when they can be supportive and with client approval; recognize that in many cultures family bonds and support are important N Base interventions on research evidence (evidence-based practice) A A crisis is an acute, time-limited emotional response to a stressful event or series of stressful events that can be real, potential, or imagined; a crisis can overwhelm a person’s coping abilities (Table 16-2: Types of Crises) B Crises progress through four distinct phases (Table 16-3: Caplan’s Phases of Crisis Development) Table 16-3 Caplan’s Phases of Crisis Development C Continuing stress increases vulnerability and causes anxiety and physical discomfort and threatens the person’s self-esteem, integrity, and safety D The response to a stressor varies from person to person and will be determined by perception of the situation, prior coping skills, the client’s support system, and psychologic and physical health (e.g., some may experience a midlife crisis or empty-nest syndrome and others may not) E Crises are usually self-limiting and last between 4 and 6 weeks F Ineffective coping during a crisis can lead to personality disorganization and long-term maladaptive behaviors G Crisis intervention is a focused short-term therapy for clients in situations in which their usual coping has been overwhelmed H The goal is to return the client to precrisis level of functioning, but as the individual tries to regain psychologic equilibrium, there is the opportunity for personal growth by learning new coping skills and developing additional resources A Implement interventions that are directive and goal oriented because of the short time frame; focus on present problem and immediate crisis issues only B Progress through stages: intervening immediately, stabilizing the client, facilitating a realistic understanding of the event, facilitating use of resources, encouraging self-reliance, developing and utilizing healthy support systems C Assess the client’s developmental level, perception of the event, past and current coping skills, resources and support systems, and potential for violence/suicide D Encourage the client to express feelings and develop healthier coping skills E Refer the client for more long-term care treatment, to support groups, and to social services as needed A Includes child abuse, partner abuse, and elder abuse B Abuse can be physical, emotional, sexual, and/or financial C Neglect of a dependent child or elder is more common than abuse; neglect is the failure to provide basic care needs such as nutrition, shelter, and health care D The incidence of psychiatric illness and addiction disorders is higher in families where there is domestic violence E Families where abuse occurs are often isolated, with few support systems, have a history of abusive behaviors, and experience stressors such as unemployment or illness F The child who is most likely to be abused has a physical or mental handicap, was born prematurely or at a difficult time in the family’s history; such children become scapegoats and are blamed for the family’s problems; an elder adult who is abused may have physical or cognitive disabilities that make them more vulnerable and require caregivers to take on more responsibility G Societal influences of violence, sexual imagery, cultural norms about family roles, and the use of physical punishment to discipline may increase the tendency toward domestic violence A Identify signs of violence/neglect 1. Unexplained or frequent injuries or accidents, conflicting stories about injuries, delayed treatment for injuries, injuries in various stages of healing 2. Failure to thrive; delayed growth and development 3. Inadequate hygiene, inappropriate dress, and eating and sleeping disorders 5. Sexually transmitted infections; inappropriate (premature) sexual knowledge B Report suspicions of child and elder abuse to the appropriate governmental agency, which is a requirement for nursing licensure in most states; the nurse does not need to be absolutely certain and provide proof, there only needs to be a reasonable suspicion 1. Interventions for elder and child abuse include education about usual growth and development, methods of discipline of children, referral to support groups and social services, anger management, assertiveness training, and relaxation therapy 2. Removal of at-risk children; dependent adults may be removed from the home for their safety 3. Victims of partner abuse usually require several attempts before successfully leaving an abusive situation; victims should be helped to develop strategies for exiting an abusive situation, which include identifying financial resources, safe houses, and support groups; nurses should guard against expressing frustration to victims who choose to remain in their current situations A Rape counseling is a form of therapy directed to victims of sexual assault; sexual assault occurs when there is lack of consent regarding the event; minors and people with cognitive impairments are regarded as being unable to give consent; sexual activity between a minor or a cognitively impaired adult and a competent adult is a form of sexual assault; rape is an assault, the use of power to overwhelm someone B Sexual assaults may include actions such as fondling or indecent exposure C Although most victims of rape are women, men also can be victims of rape D Myths such as the woman must have done something to provoke the rape often keep women from reporting rapes E The acute reaction to rape is often shock, disbelief, and dissociation from the event F Somatic problems, sleep disorders, phobias, social withdrawal, and depression may occur as later responses, especially if therapy is not sought and received A Treat physical injuries, protect against sexually transmitted infections, offer pregnancy prevention and emotional support B Create a safe environment in which the victim may express feelings and regain some sense of choice and control C Provide support to family and friends of the victim and direct them how to support the victim appropriately D Refer to rape counselors and/or rape counseling centers for immediate help and for longer-term support E Focus on providing physical care and emotional support; assist with gathering evidence for criminal prosecution if needed
The Practice of Mental Health/Psychiatric Nursing
Legal Concepts Related to Mental Health/Psychiatric Nursing
Overview
The Nurse’s Responsibilities in Relation to the Law
Community Health Services
Overview
The Nurse’s Role in Community Nursing
Therapeutic Nurse-Client Relationship
Overview
General Nursing Care of Clients with Mental Health/Psychiatric Problems
Crisis Intervention
Overview
Phase
Description
Phase 1
Exposure to stressor (can be real or imagined) causes increasing anxiety as usual coping skills do not bring resolution to the problem.
Phase 2
Utilization of more dysfunctional coping behaviors occurs as high level of anxiety impedes problem solving.
Phase 3
Anxiety reaches panic level when effective coping is lost.
Phase 4
Anxiety overwhelms the individual, who feels immobilized or acts out with violence and self-destructive behaviors; personality disorganization occurs.
Nursing Care of Clients in Crisis
Nursing Care in Relation to Violence
Domestic Violence
Overview
Nursing Care of Situations of Domestic Violence/Neglect
Rape Counseling
Overview
Nursing Care of Clients Who Have Experienced Sexual Assault
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


The Practice of Mental Health/Psychiatric Nursing
Get Clinical Tree app for offline access