Advances in anesthetic agents and monitoring have resulted in more precise and safer delivery of anesthetic agents. Caring for the critically ill patient who is emerging from anesthesia requires diligent monitoring of the patient’s physical and psychologic status to prevent potential complications that may occur as a result of the anesthetic agents or techniques. To provide safe and competent patient care, the critical care nurse needs knowledge of anesthetic agents and techniques and the physiologic and psychologic responses of patients who receive anesthesia.1,2 The complex structure of the anesthetic agents, combined with potential medication interactions and the patient’s physical condition, can make it difficult to predict the patient’s response when emerging from anesthesia. Knowledge of the general principles of anesthesia prepares the nurse for the most commonly expected outcomes.2,3 The American Society of Anesthesiologists’ physical status classification is widely accepted as a method of preoperative patient evaluation.4 It guides communication of clinical conditions and predicts risks for anesthesia (Box 42-1). Preoperative evaluation allows the anesthesia care provider to individualize and modify care for patients at high risk for surgery.4 The type of anesthesia used for surgery may be local, regional, or general. Local and regional anesthetics eliminate the sensation of pain to a specific part of the body without loss of protective reflexes or consciousness. Many patients also receive intravenous sedation with benzodiazepines to relieve anxiety, provide amnesia, and promote relaxation. Local anesthesia with sedation may be defined as moderate or procedural sedation. Another term used is monitored anesthesia care. Depending on the sedation given and the patient’s response, the level of consciousness can range from light to deep. Further information on sedation is provided in Chapter 10. Regional anesthesia includes peripheral and central neuraxial (spinal, epidural, caudal) blocks. The blocks include single injection and continuous infusion techniques, typically used for postoperative or postprocedural analgesia. Spinal anesthesia involves injecting local anesthetic into cerebrospinal fluid contained within the subarachnoid space, below L1 in the adult and L3 in the child.5 Epidural anesthesia involves injecting the epidural space, which lies within the vertebral canal but outside the dural sac, with local anesthetics. Epidurals may be performed at all levels of the neuraxis. Spinal and epidural anesthesia cause sensory and motor anesthesia. The advantages of epidural over spinal anesthesia are a decreased incidence of spinal headache, less incidence of systemic hypotension, ability to provide a segmental sensory block, and increased ability to provide postoperative pain management.6 General anesthesia is a controlled, reversible state of unconsciousness: the patient is not arousable, there is partial or complete loss of protective reflexes, and the airway and ventilation needs to be continuously monitored and maintained. An endotracheal tube is commonly used for airway maintenance for general anesthesia, although a laryngeal mask airway (LMA) may also be used.7 Several factors influence the choice of anesthetic agent and the mode of delivery, including age and coexisting diseases, site of surgery, position of patient during surgery, status of surgery (i.e. elective, emergent), duration of the procedure, the skills of the anesthesia care provider and surgeon, and patient preference.8 The goals of general anesthesia are analgesia, amnesia/hypnosis, suppression of autonomic and sensory reflexes, and skeletal muscle relaxation.9 Stages of anesthesia, defined by Guedel around World War I, were initially used to identify the patient’s physiologic state and monitor anesthetic depth. These stages are less relevant today due to technologic advances in monitoring and anesthetic agents with faster onset and elimination, limiting the usefulness of the classic signs and symptoms associated with the stages to assessment and care of the patient after surgery.10 During general anesthesia, the goal is to keep the patient insensate, immobile, and safe. Recall or awareness during surgery can occur when the depth of anesthesia is inadequate (Box 42-2). Excessive anesthesia may stress the patient and increase emergence and recovery time. The level of anesthesia is monitored by continual assessment of the patient’s clinical presentation. Basic anesthetic monitoring standards adopted by the American Society of Anesthesiologists (ASA) mandate the use of pulse oximetry, capnography, an oxygen analyzer, disconnect alarms, body temperature measurements, and a visual display of an electrocardiogram (ECG) during the intraoperative period in all patients undergoing anesthesia.11 The standard may be exceeded as warranted by the patient’s condition and additional monitors used. External monitoring devices used to assess levels of anesthesia include lower esophageal contractility, heart rate variability, surface electromyogram, spontaneous electroencephalographic activity monitors, and evoked potentials. Typically two or more anesthetic agents are used in combination to achieve the desired level of anesthesia. To anticipate the patient’s response, it is important for the nurse to have knowledge of the anesthetic agents that are used and their usual physiologic effects.2 The characteristics of ideal anesthetic agents and adjuncts are listed in Box 42-3. Inhalation agents are used for induction and maintenance of anesthesia or, in combination with other anesthetic agents, to maintain surgical anesthesia. They can be classified as volatile or gaseous. Volatile agents are further classified as halogenated hydrocarbons or ethers, are liquid at room temperature, and have a boiling point of 20° C. Gaseous agents are gases at room temperature. Inhaled anesthetics are delivered through the respiratory tract and are absorbed into the circulation through the alveoli. The effects of inhalation agents depend on alveolar ventilation, the ventilation-perfusion ratio, co-administered gases, gas flow, and the physicochemical properties of the gas. Their exact mechanism of action is unknown, but all cause central nervous system (CNS) depression and a state of unconsciousness that is deep enough to allow surgery. Table 42-1 lists the inhalation anesthetics presently used and their chief characteristics, effects, and nursing implications.10 TABLE 42-1 CNS, Central nervous system; SVR, systemic vascular resistance. Because inhalation anesthetics can produce adverse effects such as vasodilation, hypotension, dysrhythmias, and myocardial depression, other medications and methods of delivery have been sought to provide general anesthesia. Intravenous anesthetics are commonly used in the perioperative period. Intravenous anesthetics are grouped by their primary pharmacologic action as nonopioid or opioid intravenous agents.12–14 The nonopioid agents are further divided into the barbiturates, nonbarbiturates, and sedatives. These medications can be administered by intermittent intravenous push dosing to induce anesthesia or by continuous intravenous drip to maintain anesthesia. Gamma-aminobutyric acid (GABA) is an inhibitory neurotransmitter. The nonopioid medications appear to interact with GABA in the brain. Activation of the GABA receptors inhibits the postsynaptic neurons and results in a loss of consciousness. Barbiturates bind to GABA postsynaptic receptors, inhibiting neuronal activity and causing a loss of consciousness. Sedatives such as benzodiazepines potentiate the action of GABA, leading to inhibition of neuronal activity. Nonbarbiturate induction agents, such as etomidate, antagonize the muscarinic receptors in the CNS and work as opioid agonists, resulting in a hypnotic state and loss of consciousness. Table 42-2 presents the nonopioid intravenous anesthetics and their effects and nursing considerations.12 TABLE 42-2 NONOPIOID INTRAVENOUS ANESTHETICS Flumazenil (Romazicon) reverses the sedative, amnesic, respiratory depressant, and muscle-relaxant effects of benzodiazepines.14 This medication is specific for the benzodiazepine receptors and does not reverse the effects of barbiturates or opiates. It should be used with caution in patients who have a history of seizures or chronic benzodiazepine use, as it can precipitate seizures. Because flumazenil has a shorter duration of action than most of the benzodiazepines, the risk of resedation can occur after the initial dose starts to wear off, especially when high doses of benzodiazepines are administered. The patient must be monitored for resedation and other residual effects. If the patient develops signs of resedation, flumazenil is repeated at 20-minute intervals. Flumazenil has proved to be a valuable asset in the care of the patient who has received an excessive dose of a benzodiazepine such as midazolam or lorazepam. Consequently, flumazenil is very useful intraoperatively, postoperatively, and in the critical care unit. Intravenous opioid anesthetics play an important role in clinical anesthesia care. These medications enhance the effectiveness of inhalation agents by providing the analgesic portion of the anesthetic process. Intravenous opioids blunt the sympathetic response to painful stimuli during anesthesia. The use of opioids allows for reduction in the concentration of the inhalation agent to be administered, increasing safety. Opioids bind to specific receptors and produce a morphine-like or opioid agonist effect. Opioids are used to manage acute and chronic pain and are administered for general anesthesia, sedation, and pain relief during regional anesthesia; they are important in all phases of the perioperative experience. Table 42-3 presents a summary of clinical uses and nursing implications for the most frequently used opioids.13 TABLE 42-3 *Agents include alfentanil (Alfenta), fentanyl (Sublimaze), ketorolac (Toradol), morphine, sufentanil (Sufenta), remifentanil (Ultiva), and hydromorphone (Dilaudid). Opioid antagonists are used to reverse the effects of opioids, particularly respiratory depression, restoring spontaneous ventilation in patients who are breathing inadequately. The medication of choice in perianesthesia care is naloxone (Narcan). Naloxone competes with and displaces the opioid on the receptor site; it therefore reverses respiratory depressant and analgesic effects of opioids. Naloxone is diluted and then titrated to the patient’s response, minimizing the risk of rapid reversal and subsequent adverse effects. The onset of action is 1 to 2 minutes and the duration of action is 1 to 4 hours. If adequate reversal has not been achieved after 3 to 5 minutes, naloxone administration is repeated until reversal is complete.15 Neuromuscular blocking agents (NMBAs), or muscle relaxants, interrupt the transmission of impulses from the nerve to the muscle, causing a decrease in muscle activity. Decreasing muscle activity allows the surgeon to operate in a quiet field and decreases the need for deep anesthesia. These medications have contributed greatly to clinical anesthesia care. Use of NMBAs is not limited to the operating room; they are used to facilitate endotracheal intubation, to terminate laryngospasm, to eliminate chest wall rigidity that may occur after the rapid injection of potent opioids, and to facilitate mechanical ventilation by producing total paralysis of the respiratory muscles.15 Table 42-4 presents a pharmacologic overview of the commonly used skeletal muscle relaxants.16 A number of factors can potentiate or antagonize the effects of nondepolarizing NMBAs; these factors are listed in Box 42-4.17 TABLE 42-4 NEUROMUSCULAR BLOCKING AGENTS* *Long-acting agents include pancuronium (Pavulon); intermediate-acting agents include atracurium (Tracrium), vecuronium (Norcuron), and cisatracurium (Nimbex); short-acting agents include rocuronium (Zemuron) and succinylcholine (Anectine), which is a depolarizing agent. The pharmacologic actions of nondepolarizing NMBAs can be reversed by anticholinesterase medications such as neostigmine (Prostigmin). These medications increase the amount of acetylcholine available at the receptor sites by preventing its destruction by acetylcholinesterase. This promotes more effective competition of acetylcholine with the nondepolarizing skeletal muscle relaxant that is occupying the receptor sites. Because of the increased availability and mobilization of the acetylcholine, the concentration gradient favors acetylcholine and the removal of the nondepolarizing agent from the receptors, resulting in the return of normal skeletal muscle depolarization and contraction.18 These medications also produce undesired side effects by increasing the level of acetylcholine at receptor sites in the heart, the lungs, the eyes, and gastrointestinal tract, which can lead to bradycardia, bronchospasm, miosis, and increased peristalsis and secretion. To prevent or minimize these effects, anticholinergic agents such as atropine or glycopyrrolate (Robinul) are given with the anticholinesterase agent. Table 42-5 outlines the common NMBA reversal agents used in anesthesia and their nursing implications.18 TABLE 42-5 The goal of management in the immediate postoperative period is the recognition and immediate treatment of any problems, to eliminate or lessen complications that may occur. This requires the collaborative effort of the nurse, the anesthesiologist, and the surgeon. Physical assessment of the postanesthesia patient begins immediately on admission to the unit. This initial assessment focuses on airway, ventilation, and circulation (heart rate, rhythm, and blood pressure). Following the brief initial assessment, the nurse admitting the patient receives a verbal report from the anesthesia care provider and surgeon. The report includes information about the patient’s general condition, significant past history or co-morbidities, the operation performed, the type of anesthesia administered, estimated blood loss, total intake and output during surgery, and any problems or complications encountered in the operating room.19 Pulse oximetry, a noninvasive technique, measures oxygen saturation of functional hemoglobin. Pulse oximetry can be used to identify hypoxemia, and its use should be standard on all postoperative patients. If the patient is intubated and mechanically ventilated, capnography can be used to assess for adequate ventilation. Arterial blood gas measurements are appropriate to definitively confirm abnormal pulse oximetry or capnography values. Normal pulse oximetry values are 97% to 99%; however, preanesthetic baseline values must be noted. Some patients normally have lower saturation values on room air for a variety of reasons, and attempting to maintain higher oxygen saturation levels may result in prolonged oxygen therapy.20 For spontaneously breathing patients, supplemental oxygen may be needed, typically using nasal cannula (prongs) or simple facemask. Surgery and anesthesia often interrupt the normal functioning of the nose, so humidification or nebulization with oxygen delivery may be needed. Humidifiers convert water from the liquid to the gaseous state, whereas nebulizers produce tiny water particles. This is especially helpful at higher flow rates.21 Patients may require mechanical ventilation following anesthesia. Various modes, such as positive end-expiratory pressure (PEEP), continuous positive airway pressure (CPAP), and synchronized intermittent mandatory ventilation (SIMV), are used to improve the respiratory status of the patient.21 A significant aspect of perianesthesia nursing management is the stir-up regimen.22 The regimen is aimed at the prevention of complications, primarily atelectasis and venous stasis. The stir-up regimen consists of five major activities—deep-breathing exercises, coughing, positioning, mobilization, and pain management. The sustained maximal inspiration (SMI) maneuver is a method to enhance the lung volumes of postoperative patients.22 The SMI maneuver consists of having the patient inhale as close to lung capacity as possible and, at the peak of inspiration, hold that volume for 3 to 5 seconds before exhaling it. This maneuver is more effective than simple deep breathing in preventing reduced lung volumes in the immediate postanesthesia periods. If the patient’s vital capacity is inadequate or if anesthesia respiratory depression is prolonged, deep breathing and the SMI maneuver may be augmented with a manual resuscitation bag connected to an oxygen source or with an intermittent positive-pressure breathing apparatus.
The Perianesthesia Patient
Selection of Anesthesia
General Anesthesia
Anesthetic Agents
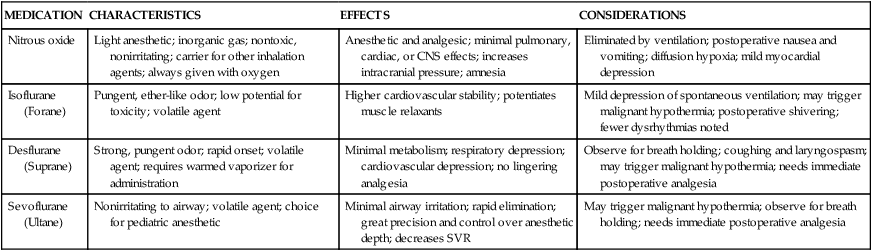
Inhalation Agents
MEDICATION
CHARACTERISTICS
EFFECTS
CONSIDERATIONS
Nitrous oxide
Light anesthetic; inorganic gas; nontoxic, nonirritating; carrier for other inhalation agents; always given with oxygen
Anesthetic and analgesic; minimal pulmonary, cardiac, or CNS effects; increases intracranial pressure; amnesia
Eliminated by ventilation; postoperative nausea and vomiting; diffusion hypoxia; mild myocardial depression
Isoflurane (Forane)
Pungent, ether-like odor; low potential for toxicity; volatile agent
Higher cardiovascular stability; potentiates muscle relaxants
Mild depression of spontaneous ventilation; may trigger malignant hypothermia; postoperative shivering; fewer dysrhythmias noted
Desflurane (Suprane)
Strong, pungent odor; rapid onset; volatile agent; requires warmed vaporizer for administration
Minimal metabolism; respiratory depression; cardiovascular depression; no lingering analgesia
Observe for breath holding; coughing and laryngospasm; may trigger malignant hypothermia; needs immediate postoperative analgesia
Sevoflurane (Ultane)
Nonirritating to airway; volatile agent; choice for pediatric anesthetic
Minimal airway irritation; rapid elimination; great precision and control over anesthetic depth; decreases SVR
May trigger malignant hypothermia; observe for breath holding; needs immediate postoperative analgesia
Intravenous Anesthetics
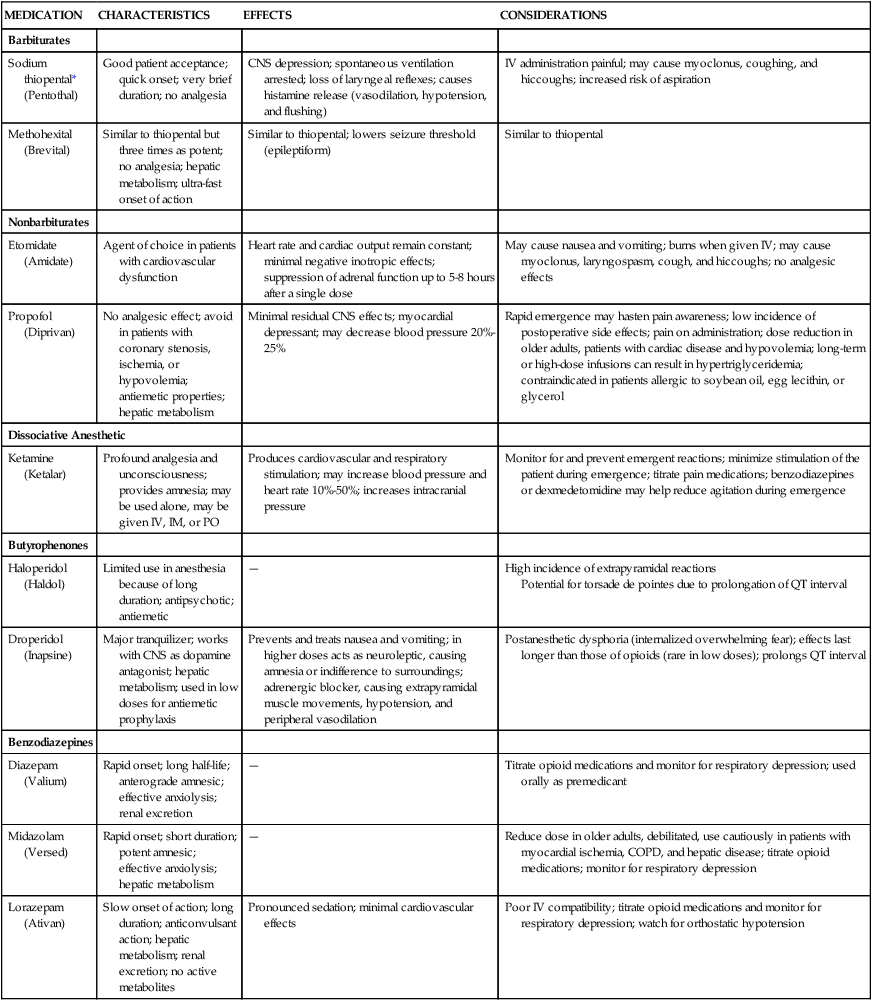
Nonopioid Intravenous Anesthetics
MEDICATION
CHARACTERISTICS
EFFECTS
CONSIDERATIONS
Barbiturates
Sodium thiopental* (Pentothal)
Good patient acceptance; quick onset; very brief duration; no analgesia
CNS depression; spontaneous ventilation arrested; loss of laryngeal reflexes; causes histamine release (vasodilation, hypotension, and flushing)
IV administration painful; may cause myoclonus, coughing, and hiccoughs; increased risk of aspiration
Methohexital (Brevital)
Similar to thiopental but three times as potent; no analgesia; hepatic metabolism; ultra-fast onset of action
Similar to thiopental; lowers seizure threshold (epileptiform)
Similar to thiopental
Nonbarbiturates
Etomidate (Amidate)
Agent of choice in patients with cardiovascular dysfunction
Heart rate and cardiac output remain constant; minimal negative inotropic effects; suppression of adrenal function up to 5-8 hours after a single dose
May cause nausea and vomiting; burns when given IV; may cause myoclonus, laryngospasm, cough, and hiccoughs; no analgesic effects
Propofol (Diprivan)
No analgesic effect; avoid in patients with coronary stenosis, ischemia, or hypovolemia; antiemetic properties; hepatic metabolism
Minimal residual CNS effects; myocardial depressant; may decrease blood pressure 20%-25%
Rapid emergence may hasten pain awareness; low incidence of postoperative side effects; pain on administration; dose reduction in older adults, patients with cardiac disease and hypovolemia; long-term or high-dose infusions can result in hypertriglyceridemia; contraindicated in patients allergic to soybean oil, egg lecithin, or glycerol
Dissociative Anesthetic
Ketamine (Ketalar)
Profound analgesia and unconsciousness; provides amnesia; may be used alone, may be given IV, IM, or PO
Produces cardiovascular and respiratory stimulation; may increase blood pressure and heart rate 10%-50%; increases intracranial pressure
Monitor for and prevent emergent reactions; minimize stimulation of the patient during emergence; titrate pain medications; benzodiazepines or dexmedetomidine may help reduce agitation during emergence
Butyrophenones
Haloperidol (Haldol)
Limited use in anesthesia because of long duration; antipsychotic; antiemetic
—
High incidence of extrapyramidal reactions
Potential for torsade de pointes due to prolongation of QT interval
Droperidol (Inapsine)
Major tranquilizer; works with CNS as dopamine antagonist; hepatic metabolism; used in low doses for antiemetic prophylaxis
Prevents and treats nausea and vomiting; in higher doses acts as neuroleptic, causing amnesia or indifference to surroundings; adrenergic blocker, causing extrapyramidal muscle movements, hypotension, and peripheral vasodilation
Postanesthetic dysphoria (internalized overwhelming fear); effects last longer than those of opioids (rare in low doses); prolongs QT interval
Benzodiazepines
Diazepam (Valium)
Rapid onset; long half-life; anterograde amnesic; effective anxiolysis; renal excretion
—
Titrate opioid medications and monitor for respiratory depression; used orally as premedicant
Midazolam (Versed)
Rapid onset; short duration; potent amnesic; effective anxiolysis; hepatic metabolism
—
Reduce dose in older adults, debilitated, use cautiously in patients with myocardial ischemia, COPD, and hepatic disease; titrate opioid medications; monitor for respiratory depression
Lorazepam (Ativan)
Slow onset of action; long duration; anticonvulsant action; hepatic metabolism; renal excretion; no active metabolites
Pronounced sedation; minimal cardiovascular effects
Poor IV compatibility; titrate opioid medications and monitor for respiratory depression; watch for orthostatic hypotension
Benzodiazepine Antagonists
Opioid Intravenous Anesthetics
CLINICAL USES
IMPLICATIONS
CONSIDERATIONS
Preoperative sedation
Monitor for hypotension
Keep naloxone (Narcan) available
Induction of anesthesia
Monitor for bradycardia
Keep resuscitation equipment available
Maintenance of anesthesia
Monitor for respiratory depression
Respiratory depressant effect may outlast analgesia
Postoperative pain management
May cause nausea and vomiting
Opioid Antagonists
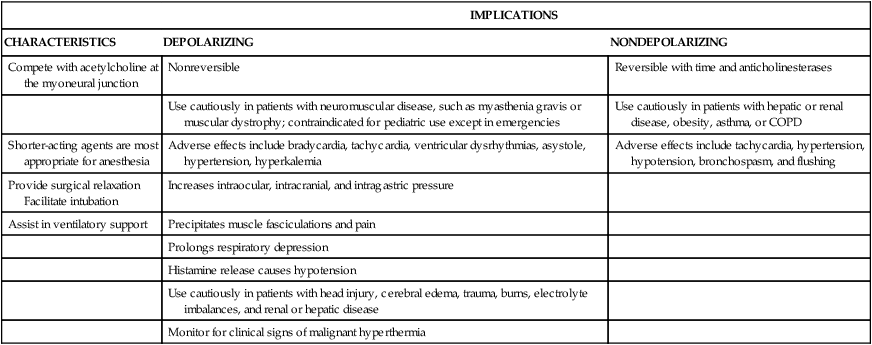
Neuromuscular Blocking Agents
IMPLICATIONS
CHARACTERISTICS
DEPOLARIZING
NONDEPOLARIZING
Compete with acetylcholine at the myoneural junction
Nonreversible
Reversible with time and anticholinesterases
Use cautiously in patients with neuromuscular disease, such as myasthenia gravis or muscular dystrophy; contraindicated for pediatric use except in emergencies
Use cautiously in patients with hepatic or renal disease, obesity, asthma, or COPD
Shorter-acting agents are most appropriate for anesthesia
Adverse effects include bradycardia, tachycardia, ventricular dysrhythmias, asystole, hypertension, hyperkalemia
Adverse effects include tachycardia, hypertension, hypotension, bronchospasm, and flushing
Provide surgical relaxation Facilitate intubation
Increases intraocular, intracranial, and intragastric pressure
Assist in ventilatory support
Precipitates muscle fasciculations and pain
Prolongs respiratory depression
Histamine release causes hypotension
Use cautiously in patients with head injury, cerebral edema, trauma, burns, electrolyte imbalances, and renal or hepatic disease
Monitor for clinical signs of malignant hyperthermia
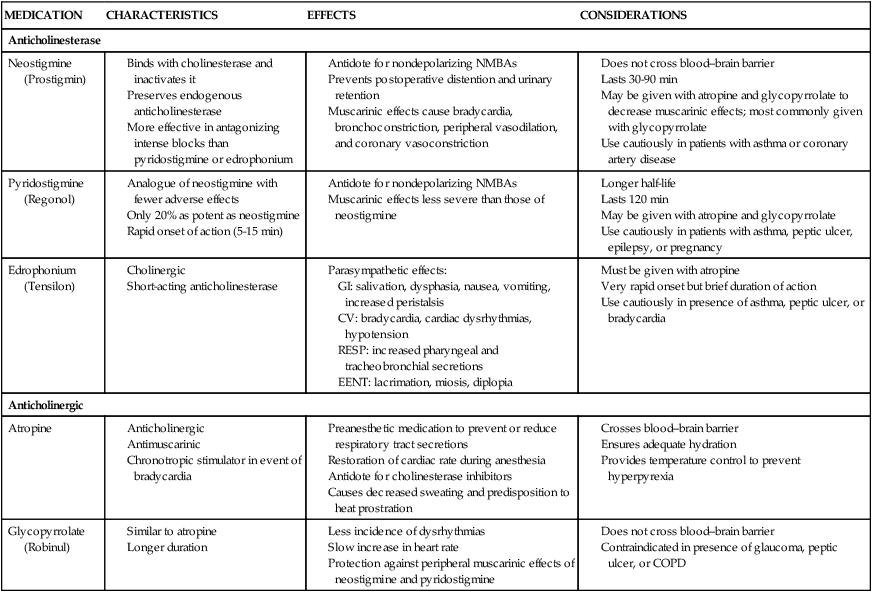
Neuromuscular Blocking Agent Antagonists
MEDICATION
CHARACTERISTICS
EFFECTS
CONSIDERATIONS
Anticholinesterase
Neostigmine (Prostigmin)
Pyridostigmine (Regonol)
Edrophonium (Tensilon)
Anticholinergic
Atropine
Glycopyrrolate (Robinul)
Perianesthesia Assessment and Care
Respiratory Function
Stir-Up Regimen
Deep-Breathing Exercises.
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


The Perianesthesia Patient
Get Clinical Tree app for offline access
