4. The neck and upper limbs
In this chapter, the anatomy, examination and common injuries of the arm are discussed.
Most of the injuries which are treated in minor areas are to the hand. It is a difficult structure to examine and its practical and psychological importance for every patient is the main reason why the care of minor injuries is an important task. Injuries are often occult, showing themselves fully only when it has become difficult to treat them. This can have legal as well as medical repercussions. A sound knowledge of the anatomy, examination and injuries of the hand is therefore the key skill for any minor injury practitioner.
The neck is a different issue to the arm in terms of anatomy and pathology. However, some of the structures which cause problems in the arm originate in the neck, and the neck itself can be the cause of pain in the arm. Therefore this chapter will begin with a limited discussion of the neck, looking at musculoskeletal problems which arise in minor injury areas.
The neck
The neck is constructed around the upper part of the spine, which does double service as a part of the skeleton and a channel for nerves and blood vessels. Its musculoskeletal function is to attach, carry and move the head. It is also a transit point for essential services between head and body. It contains large blood vessels which supply the brain, and a multiplicity of nerves. It is also the channel to the respiratory and gastrointestinal systems. These structures emerge from and disappear into better protected areas in the head and chest, but they are superficial and vulnerable in the neck.
Physical forces which would cause no injury elsewhere, such as moderate compression or twisting, can be lethal in the neck. Wounds are very dangerous. Closed injuries which involve angulation or axial compression can be a threat to life. Serious injuries rarely arise as a result of ordinary daily activity, but injuries where the mechanism is more severe because of speed, height or violent contact expose the neck to great risk which it is very difficult to protect against.
Manage patients who present with possible neck injuries with care. Follow the guidelines and policies which are in place in your area. When there is doubt, use a hard collar and spinal immobilisation until the neck can be fully assessed.
Concern about musculoskeletal injury to the neck is focused on the cervical spine, on the bone, cartilage and ligaments. Injuries do occur to the muscles of the neck, but, in isolation, these are not dangerous, and they are probably diagnosed more often than they actually occur. The muscles of the neck are not often subjected to the complicated stresses which are common for the muscles in other parts of the body. Referral of pain is also a significant phenomenon at the neck and shoulders: pain which is felt around muscle may originate from the spine. Often the patient with discomfort at a neck muscle has gone to bed with no symptoms and wakened with pain. There is no history to suggest which tissue is causing the problem.
Displacement or destruction of a part of the spine may damage, or threaten to damage, the spinal cord. Such injuries can kill or paralyse the patient for life. Dangerous injuries may also occasionally appear to be less serious in the first instance. The presence of severe muscle spasm, so that the neck is rigid, in a patient with a significant history of injury, should lead you to suspect unstable ligament or other serious injury.
Many of the neck injuries which are classed as minor can still cause considerable difficulties. There are four common considerations.
1. A neck problem may be minor in the sense that it is not a threat to life or limb, that no vital structure has been damaged, or that there is no advanced treatment to offer the patient. However, the problem may not be easy to diagnose or treat, and the patient may suffer from recurrence or prolonged pain and disability.
2. Many patients who present as ‘injured’ with neck pain have no history of injury. You have the task of deciding whether the pain has a musculoskeletal cause, or whether the patient is ill. Is the pain referred from a vital organ, or is some other disease process, such as neoplasm or infection, causing the symptoms? This is a heavy responsibility. Have a low threshold for seeking a senior medical opinion.
3. It can be difficult, when examining patients with pain in the neck and surrounding areas (including the head, the upper back and the arms), to distinguish between well-localised pain and tenderness at the site of a muscle injury, pain which is referred to those areas from the spine and the spinal nerves, and pain from other sources. The rules for assessment of those problems are the same as for the limbs, but it is difficult in a clinical setting to diagnose the cause of pain in the neck or the back. If, as it often does, the differential diagnosis includes something serious, obtain a senior medical opinion.
4. X-rays of the neck are often sought by patients when they have pain, even though they are not injured. Virtually everyone who has reached middle age shows degenerative changes on a neck X-ray, whether or not they have pain. Patients who are having an acute attack of neck pain and are otherwise healthy are unlikely to gain anything from an X-ray of the neck. Focus on a thorough clinical examination to exclude non-musculoskeletal causes and to evaluate the severity of the patient’s problem.
Anatomy
The cervical section of the spine comprises the upper seven vertebrae and their ligaments and cartilage-covered intervertebral discs. It is a structure which, perhaps more than any other in the body, copes with conflicting demands. It is stable enough to support the weight of the head, yet it is the most flexible part of the spine to permit the mobility which the head requires. At the same time, it provides the armour which protects the spinal cord from damage. It also allows passage for the fibres of the cord, through a multitude of outlets, to the tissues which it supplies. The vertebral artery passes along the cervical spine to the brain.
Bone supplies the rigid elements in the spine. The vertebrae are a vertical stack of irregular bones separated in their frontal sections by pads of fibrocartilage filled with a semiliquid substance called the nucleus pulposus and linked in their rear sections by a succession of pairs of synovial facet joints. The pads, called intervertebral discs, allow flexibility between the bony parts of the spine, and they also function as shock absorbers.
The spine is arranged in a straight line when seen from the front or back, but in a series of alternating curves when seen from the side. The cervical section has a concave curve on its posterior aspect. The thoracic spine (the 12 vertebrae which articulate with the ribs) is convex. The lumbar (five vertebrae which lie in the lower back and link the whole structure through the sacrum, to the pelvic girdle and the lower limbs) is concave. The sacrum, the section of five fused vertebrae which articulates with the two wings of the pelvis at the back, is convex. The erect posture of the human is the result of a succession of resilient, variable, dynamic compensations rather than simple straightness, and problems with the alignment of the spine, and the balance of the structures which support it, may be a cause of chronic pain and recurring injury.
Scoliosis is a term which means that the spine has an abnormal curve to the side. Kyphosis means an increase in the normal convexity of the thoracic spine, seen from the side, and lordosis refers to the opposite phenomenon in the lumbar area, an accentuation of the curve of the lower back.
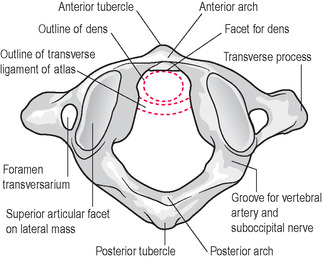
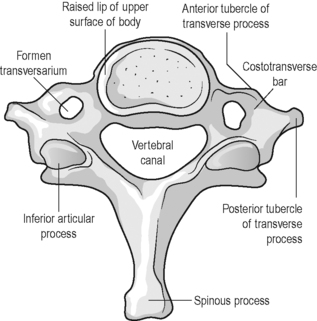
The vertebrae are similar in shape and structure along the whole length of the spine. They become larger as they descend to the pelvis. However, the first and second cervical vertebrae (Figure 4.1 and Figure 4.2), sometimes called the upper cervical spine, are specially adapted for the task of uniting the spine to the skull and permitting the head to flex, extend and rotate.
The vertebrae of the lower cervical spine (Figure 4.3), C3 to C7, consist of an anterior part, which is a disc of bone, the body, and a posterior part, the vertebral arch. The arch is made up of small bony processes united to form an enclosed space. Two small rods project backwards, one on each side, from the vertebral body. These are called the pedicles. On each side, the bony projections which begin as the pedicles continue at a new angle, still backwards but turning towards each other so that they meet in the midline, where they fuse. These projections now look flattened rather than rounded. They are called laminae. The space which is enclosed by the posterior border of the body, the pedicles and the laminae is called the vertebral foramen.
Continuing backwards from the point of fusion of the laminae there is, in the cervical region, a bifid (meaning, in two parts) bony projection, the spinous process of the vertebra. The spinous processes collectively are the most accessible parts of the spine for the examiner. They form the series of bony projections which can be felt in the midline of the back from the top of the neck to the beginning of the cleft of the buttocks.
Each vertebra also has two transverse processes, one projecting from each side of the vertebral body and both pointing in an opposite lateral direction. The transverse processes of the cervical spine are unusual in having a smaller version of the vertebral foramen, a small opening called the transverse foramen, enclosed within each process. The vertebral artery passes up through the channel created by these openings to make its way to the cranium.
These three processes, the two transverse and the spinous in the midline, are used as attachment points for ligaments and muscles. In the thoracic area, the transverse processes are part of the articulation with the ribs at the back.
On the superior and inferior aspects of the arch, at the points where the pedicles meet the laminae, there are articular projections called the zygapophyses. The zygapophyses on the upper surfaces of the arch articulate with those on the underside of the vertebral arch above throughout the spine. These zygapophyseal joints are synovial and allow a limited amount of movement, variable from one to another. The surfaces of these articular processes, which are covered with hyaline cartilage, are called facets.
There are six intervertebral discs in the cervical area. These are made of a combination of three substances. There is a coating of hyaline cartilage on the opposing surfaces of the two vertebral bodies, which are linked by the disc. These are called the cartilage end plates. The disc proper is connected to these. The disc itself has a soft centre, a thick, jelly substance called the nucleus pulposus, which gives the disc its resilience but which can herniate if its retaining outer layer is ruptured (the event known as a slipped disc). The outer layer of the disc is an arrangement of multiple bands of fibrocartilage, the annulus fibrosus, which contains the nucleus.
There is space between the pedicles of neighbouring vertebrae for the passage of spinal nerves into and out of the spine. These gaps between the pedicles are called the intervertebral foramina (meaning, openings between vertebrae).
The chain of vertebral foramina which is formed by the arches of the spine is called, in combination, the vertebral canal, and it is through this structure that the spinal cord passes from head to pelvis.
The spinal cord runs through the vertebral canal. It forms a part of the central nervous system. It is described as being divided into a series of segments; each segment has a pair of spinal nerves, and these nerves pass out into the body through the intervertebral foramina of the spine, where they form part of the peripheral nervous system. The parts of the spinal nerve which joins the spinal cord are called the roots. Each nerve has two roots, a ventral (front) and a dorsal (back) root. The ventral root carries efferent (from the Latin, to carry out of) motor fibres from the cord to the spinal nerve. These nerves ultimately pass to muscles and stimulate them to contract. The dorsal root delivers afferent (from the Latin, to carry to) sensory fibres from the spinal nerve to the cord. The cervical segments are numbered from one to eight. C1 to C7 nerve roots emerge from above the vertebra for which they are numbered, and C8 emerges from between C7 and T1.
The brachial plexus (see also lumbar plexus, Chapter 5) is a combination into a network of the ventral nerves from C5 to T1, with exchanges of fibres between the different segmental nerves. It occurs after the nerve has emerged from the spine but before it reaches its peripheral distribution. The brachial plexus supplies the shoulder and arm with motor and sensory fibres (Figure 4.4).
The intervertebral discs which lie between each vertebral body are also, on their posterior aspects, in close contact with the spinal cord, and any injury which causes a herniation of the disc in a backward direction may interfere with the function of the cord. Cyriax & Cyriax (1993) point out that the anterior dura mater covering the spinal cord where it meets the vertebral bodies and discs, and the dura mater, which covers nerve roots as they pass out from the spine, are innervated, and pain will be felt if either is overstretched or compressed. There are two possibilities.
1. A backward herniation of the disc will impinge first on the dura mater where it covers the central cord and cause extrasegmentally referred pain, usually on one side only (see pain referral, Chapter 3). In the cervical area, this pain may be felt in the neck, over to the forehead, or, most commonly, in the scapular and shoulder area.
2. A herniation which is backwards but to one side or other, rather than central, will impinge upon the nerve root on that side, which is also covered at that point in a sleeve of dura mater. This will only cause pain if the pressure is slight but will cause signs of nerve compression (weakness, paraesthesia and reflex suppression) if the pressure is deep enough to reach the nerve within the sheath. These symptoms will refer to the dermatome for that nerve root.
Three of the cervical vertebrae have special features which require further description. C7 (Figure 4.3) has a larger body than the other cervical vertebrae and a longer, non-bifid, spinous process. It offers a conspicuous landmark at the base of the back of the neck, at the point of transition between the cervical and the thoracic spine. T1 is also seen, even more prominent than C7, and just below it.
In the upper cervical spine, C1, also called the atlas (Figure 4.1), after the mythic Titan who carried the weight of the heavens upon his shoulders, bears the weight of the skull. It has two articular facets on its upper surface, and the occipital bone lies upon them at the atlanto-occipital joints. These joints permit some degree of flexion and extension of the head. The undersurfaces of the atlanto-occipital joints are also adapted for articulation with the upper surfaces of C2, at the atlanto-axial joints. The atlas has no vertebral body or intervertebral disc. It is simply a bony ring made up of a front and rear arch, linked at the sides by its articular masses. The atlas has a transverse process on each side, which can be felt just under the mastoid processes (the prominences behind the ears) of the skull. Unlike the other vertebrae it does not have a projecting spinous process at the rear. There is only a posterior tubercle, a little button of bone which is difficult to palpate.
C2 (Figure 4.2) is also called the axis. It does possess a vertebral body but has a unique feature: a peg-like bony projection rises from its superior surface like a tooth (hence, its names, the dens, or the odontoid process; both derive from terms for teeth). This peg projects upwards through the arch of the atlas. It is stabilised there by ligaments, inside the foramen magnum (meaning, large opening) of the skull, which gives access to the cranium on the underside of the occipital bone. The transverse ligament crosses behind the dens and the alar ligaments pass from the dens to the occipital bone on each side. The atlas, and with it, the skull, rotate about the fixed point of the axis. Half of the neck’s range of rotation occurs at this joint. The alar ligaments are placed to prevent excessive rotation on the side opposite to each ligament (i.e. the alar ligament on the left tightens as the head rotates to the right). The alar ligament also prevents separation of the axis from the atlas. It becomes tighter as the neck is flexed. Injury which involves forced flexion and rotation of the head may rupture the ligament, allowing excessive rotation on the side which is opposite to the tear. Patients will sometimes demonstrate the frightening sense of instability which this type of injury inspires by holding onto their heads as if to prevent them from falling off.
Other ligaments stabilise the spinal column as a whole. The anterior longitudinal ligament is strong and passes down the front of the spine, attaching to vertebrae and to discs. It limits the range of extension of the spine. The posterior longitudinal ligament passes up the back of the spine, attaching to the intervertebral discs. This limits the range of spinal flexion. Ligamenta flava, a series of individual ligaments rather than a continuous band, reinforce the rear of the spine, linking neighbouring laminae and forming a part of the vertebral canal. In the cervical area the ligamentum nuchae also passes from the occipital area to the spinous process of C7.
Movement in the cervical spine is allowed and limited by the same forces, the action of the various ligaments, the disposition of the zygapophyseal joints and the mobility of the intervertebral discs, which have a capacity for compression, rotation and for stretching. In the cervical area, the discs are relatively thick, and this adds to the range of movement. The muscles of the neck offer a dynamic force for stability and mobility, and they exert a powerful protective influence when injury occurs by going into spasm to immobilise the injured area. This is one of the factors which can, initially, conceal the extent of the instability caused by an injury. Box 4.1 gives the normal cervical spine ranges of movement.
Box 4.1
The ranges of movement quoted here are the composite ranges, made up of smaller movements in different parts of the spine.
• Capsular pattern a greater limitation of side-flexion and rotation, a lesser limitation of extension.
• Joint positions close packed is extension; loose packed is a small degree of extension.
• Flexion approximately to 90°; endfeel firm.
• Extension approximately to 70°; endfeel firm.
• Rotation occurs to each side to approximately 80°; endfeel firm.
• Side-flexion occurs to each side up to approximately 45° (there is a wide variation between individuals); endfeel firm.
• Circumduction rotation of the head achieved by combining a fluent sequence of the above movements.
The cervical spine houses the vertebral artery. This is a branch of the subclavian artery. It joins the cervical spine at the transverse processes on each side of the C6 vertebra. It then passes up to enter the skull through the spine’s point of access to the cranial cavity, the foramen magnum, at the back and underside of the skull in the occipital region. The two branches of the artery unite at this level to form the basilar artery within the cranium. This artery, along with the internal carotid artery, carries the brain’s blood supply. The vertebral–basilar contribution is about one-fifth of the total. Interruption of its function may be caused, among other things, by degeneration or subluxation of the cervical spine, which may stretch or compress the vessels and will affect cerebral activity. Excessive movements of extension and rotation of the neck, common in so-called whiplash injuries, may compromise the artery in the region of the foramen magnum. The pathological process will be of ischaemia in the areas supplied. Be aware of suggestive elements in a patient’s history. Patients who suffer from cervical spondylosis or rheumatoid arthritis may be affected. A common first complaint, which should alert to the possibility of vertebral artery insufficiency in a patient with neck pain or injury, is of dizziness, and there may be light headedness and nystagmus. These symptoms are not specific to vertebral artery insufficiency alone.
Examination
Always have the vulnerability and complexity of the neck in mind. Have a low threshold for precaution, consultation and referral. Begin with ABC and the patient’s Glasgow Coma Scale (see Chapter 7).
Elicit clearly whether the patient has a history of injury. If he or she has been injured, assess the severity of the mechanism and ask about pain, movement and any neurological changes at any time since the injury until now. If you have concerns that the patient has suffered a significant injury to the spine defer examination, immobilise the neck in a hard collar, ask the patient to lie flat. Obtain a senior medical opinion.
The history of neck pain is often of an unexplained onset felt on waking. Ask about activities on the preceding day. Was an unusual amount of alcohol taken before bed? How are the patient’s pillows arranged? Does the patient sleep in a prone position with the head rotated, a posture which is thought to stress the facet joints?
Has the patient been unwell in any way around the time of the onset of pain? Is there headache, vomiting, fever or rash? Be wary of any hint of cerebral or meningeal signs. Is there chest pain, breathlessness or palpitations? Is there a cough, sore throat or earache? Does the complaint involve any change in normal salivation, are there any new swellings around the neck?
Where is the pain? Does it radiate to the shoulder? Does it pass down the arm? How far does it radiate, and in to which part of the arm? Is there dizziness or blackout; vision or hearing changes; any change in sensation or power; loss of coordination or symptoms in the lower part of the body including changes in bladder and bowel function?
Ask about any diseases which might affect the spine or spinal cord, and any long-standing symptoms which might confuse examination. Certain diseases such as rheumatoid arthritis can predispose to a spontaneous dislocation in the spine. Take care even if there is no history of injury.
A posterior disc herniation will refer pain in a non-segmental way, as will injuries to facets and ligaments in the neck. Such pain may cause headache or scapular pain. Posterior/lateral herniations, compressing nerve roots, will cause dermatomal referral (see Chapter 3, p. 63).
The pain of an injured neck may be quite severe; consider the need for analgesia and examine with care.
Look
Ask the patient to undress to expose the neck, both shoulders and the back. You will also make a neurological assessment of the arms (see below on this page and Chapter 7). A full examination of the legs is not always necessary. A patient with a stiff neck will rotate the trunk from the waist in order to turn the head. The patient may have a torticollis, an abnormal posture of the head which is commonly a combination of rotation and side-flexion. This is usually caused by muscle spasm; however, on occasion, more serious rotational deformities at the facets of the spine may occur. Assess spinal posture for kyphosis and scoliosis (see p. 139). Look at the posture of the shoulders. The medial border of each scapula should be about 5 centimetres from the spine. Note any asymmetry, wasting, spasm, bruising, redness or swelling.
If the patient has any infection signs examine the throat and the canals of the ears, and you may see raised lymph nodes around the neck.
Feel
Palpation of the cervical spine is most easily accomplished if the patient lies face down on a trolley with the chin pulled in. This flattens the hollow of the neck and makes the spine more prominent. Some examination trolleys have a space cut in the head rest which allows more flexion of the neck. At the top of the neck, in the midline, it is easy to feel the spinous process of C2. Below that, the next clearly prominent landmarks are the large processes of C7 and T1. The intervening processes of the cervical spine can be felt, with more or less difficulty, depending on the patient, in the central hollow of the neck. Establish that each process is present, with no gaps or deviations. The transverse processes of the atlas are large and placed just below the mastoid processes of the skull. The others are felt by placing the fingers lateral to the central columns of muscle in the middle of the neck. Once again, the processes of C7 are particularly large.
Palpation of the muscles of the neck and shoulder may reveal tenderness and spasm. Feel for raised lymph nodes from below the mandible to the occipital area, and ensure that there are no other swellings around the neck.
Move
Assess movement with particular care when the neck has been injured. Remember that the purpose of resisted tests is to demonstrate muscle or motor nerve deficits, and the purpose of passive movements is to clarify whether a joint may be causing symptoms (see Chapter 3). In all cases of neck pain and injury, the patient should first demonstrate the active range of movement which feels safe and comfortable. A patient will not willingly move an unstable neck. Any passive testing should be very gentle. In cases where there has been an injury, and its nature and severity are not yet known, passive movement should be avoided completely. Be careful not to exacerbate the patient’s symptoms or worsen the problem.
 The active movements of the neck are shown in Figure 4.5.
The active movements of the neck are shown in Figure 4.5. |
 |
 |
 |
| Figure 4.5 • |
Ask the patient to tell you if movements worsen or diminish the pain of which he or she is complaining. Ask if there are any other symptoms, including dizziness, faintness, weakness or tingling.
Nerve tests in the arms
Reflex testing is shown in Chapter 7.
Exclude a loss of sensation or power to the arms in any patient who has suffered a neck injury. Awareness, with the eyes closed, of light touch, comparing one side with the other in each dermatome (see Chapter 3) is usually an adequate assessment of sensation in a minor injury area. If any defect is found, further investigation is required. The area of any deficit should be mapped with its depth and nature to allow a distinction between problems at the root and the peripheral system.
Power in the myotomes (see Chapter 3) supplied by segments C5 to T1 can be assessed by resisted tests of the following movements:
• C5: shoulder abduction (deltoid)
• C6: elbow flexion (biceps)
• C7: elbow extension (triceps)
• C8: thumb extension (extensor pollicis longus)
• T1: finger adduction (intrinsics).
These tests are all illustrated later in this chapter and a range of similar tests for the leg is shown in Chapter 5.
Once again, any weakness will require further investigation, and a distinction should be made between a root lesion and a peripheral nerve problem. If weakness is present assess the full limb and map any deficits. The pattern of the problem will give indications of the probable source.
A patient who has a very painful, acute injury, such as a whiplash or an onset of severe neck pain, may not be able to comply with resisted tests, and any weakness or pain may be misleading. Such a patient may need an immediate senior medical opinion or further assessment at a later stage, perhaps by a physiotherapist.
Neck pain and injury
Patients should be assumed to have a serious neck injury if there is a severe mechanism of injury, such as a fall from above 10 feet (3 metres), a dive onto the head from a height into shallow water or a car crash at greater than 30 miles per hour, and if they have severe signs and symptoms of injury, such as a very painful, rigid or unstable neck, neurological deficits, loss of consciousness or collapse. The neck should be immobilised in a hard collar, the spine kept in neutral alignment with the patient lying flat and the head taped and held in position with sandbags. It may be necessary to initiate resuscitation. The neck must be assessed for all patients who present with complaints of head injury or shoulder pain (see Chapter 7 and later in this chapter).
There are two main categories of neck problems: trauma and pain with no history of injury.
The NEXUS guidelines select two clinical indications of possible severe injury, midline C spine tenderness and focal neurological deficit, a motor or sensory change, usually in the arms (Box 4.2). The other parts of the guideline select factors which may make it harder to fully assess the neck. These guidelines do not refer to the patient’s range of movement or severity of mechanism of injury. The Canadian C spine guidelines share common features with NEXUS, but are organised around elements of the history including severe mechanism and the effect of the patient’s injury on movement and behaviour since the event, and they also select one neck movement, rotation, as a predictor of severity of injury (Box 4.3).
Box 4.2
• No midline cervical spine tenderness
• No focal neurological deficit
• Normal alertness
• No intoxication
• No painful distracting injury
= NO X-RAY
Box 4.3
Low risk factors
• Simple rear-end road traffic accident (RTA)
• In sitting position in emergency department (ED)
• No midline cervical spine tenderness
• Ambulatory at any time after trauma
• Delayed onset neck pain
• Able to actively rotate neck left and right 45 degrees
High risk factors
• Age 65 or over
• Dangerous mechanism (fall >3ft/5stairs, axial load to head, RTA >60mph, RTA with rollover or ejection, bicycle crash)
• Paraesthesia of extremities
Neck trauma: whiplash
The commonest traumatic neck complaint which patients bring to minor injury clinics is so-called whiplash (Box 4.4). The term is controversial, but that is only of interest here to the extent that a standard pattern of injury should not be assumed in any given case, even though the description of how the injury happened may be rather similar from one patient to another. The patient has been involved in a car crash and will probably be distressed and unclear about the exact mechanism of injury.
Box 4.4
Examination of the patient should include:
• LOOK: posture, torticollis, guarding
• FEEL: palpation of the neck and surrounding structures to assess tenderness and spasm
• MOVE: assessment of active range of movement only (avoiding any manipulation, including passive movement)
Make a neurological assessment of power and sensation in the arms and reflexes (see Chapter 7). A patient who is walking and shows normal coordination and agility in leg movements does not require a full examination of the lower limb. Wardrope & English (1998) recommend that legs can be functionally assessed by asking the patient to stand on one leg, and then the other, with the eyes closed.
Factors such as the position of the head at the moment of impact are important in assessing the risk of fractures, subluxations and ligament injuries. Other aspects include the exact position of the patient in the car, the direction and speed of both vehicles, the sizes and types of vehicles, the point where the vehicles struck each other and movement of the patient’s car afterwards. Was the patient wearing a seatbelt? Was there a headrest? Did an air bag deploy? Which way was the patient looking at the time of collision and was the impact anticipated or completely unexpected? Did the patient’s head hit anything? Was there broken glass?
The patient’s signs and symptoms should be established from the time of the injury to the time of the examination. If the symptoms have resolved, when did that happen? Was the patient knocked out? Is the patient suffering from headache, amnesia, discharge from nose or ears, neck pain, blackouts, visual disturbances, nausea and vomiting, hearing disturbances, dizziness, coordination problems or weakness or loss of sensation in the limbs? Does the patient have any wounds, bruises or swelling? Are there injuries to clavicle or chest caused by the seat belt?
The patient’s posture and demeanour should be observed. Patients who have just emerged from a car crash may look pale and sweaty or they may be distressed and tearful because they are reacting to the incident rather than because of injury. However, you must take a history and make a careful assessment before accepting that that is the case.
A common account is of a patient stopping the car for a traffic light, or making an emergency stop, and a vehicle behind driving into the rear. The patient’s head is thrown about, and neck pain follows some minutes or hours later.
Corrigan & Maitland describe (1998) the mechanism:
1. The impact drives the patient’s body forward, throwing the head back and hyperextending the neck
2. The muscles at the front of the neck reflexively contract, and the neck is flexed
3. The head and neck decelerate.
The most traumatic aspect of this event is the hyperextension, because the chin will hit the chest before any significant hyperflexion of the neck can occur. Hyperextension can damage muscles, ligaments (especially the anterior longitudinal ligament), the discs (by compression at the back of the disc, overstretching at the front, or tearing of the whole disc from the endplate) and the zygapophyseal joints, which may suffer fractures.
The degree of severity of presentation varies widely. The Quebec classification of severity of whiplash-associated disorders is shown in Table 4.1.
| Grade | Presentation |
|---|---|
| 0 | No neck pain, no physical signs |
| 1 | Neck pain, stiffness and tenderness, no physical signs |
| 2 | Neck complaint and musculoskeletal signs |
| 3 | Neck complaint and neurological signs |
| 4 | Neck complaint and fracture or dislocation |
Patients who present in a minor injury clinic will most commonly have injuries at grades 1 or 2. In fact, X-rays are not likely to demonstrate many of the problems which the patient may have, especially in the initial period after injury. However, it is widely accepted that, as a part of correct management of whiplash injuries, the patient should have an X-ray to exclude fracture. The Royal College of Radiologists (2007) recommends X-ray of the cervical spine for patients in line with the stipulations of the Canadian C spine rules (see above).
Local guidelines or protocols will give specific routes to follow with patients who have whiplash injuries.
Treatment
If you have access to a physiotherapist, negotiate guidelines for the referral of patients with this type of injury. It is likely that the physiotherapist will favour early and active intervention for some patients, but that the larger number will be expected to be referred through the GP in the situation where the injury has not settled. This situation will obviously be related to the guidelines for medical management and X-ray requests.
Follow the guidelines for the treatment of soft tissue injuries (Chapter 3). Soft collars are generally avoided because they encourage stiffness and muscle weakness. If there is spasm, or if the muscles are painful or tired, the patient can relieve this by reclining so that the head is supported. The hollow of the neck can be further supported with a rolled up towel. Moderate use of heat is also helpful for muscle spasm, but ice is preferable for the first day or two (see Chapter 3). Gentle movements in the same pattern as for neck examination, within the limits of pain, will help to prevent unnecessary stiffness.
In bed, supporting the head and neck in a neutral position, using rolled up towels or the like to support the hollow in the back of the neck when lying flat, and higher pillows when lying on the side, will maintain comfort.
The pain may worsen over the first few days. Ibuprofen, for patients who can tolerate it, has analgesic and anti-inflammatory benefits. It can be combined with paracetamol. Advise the patient to see a GP if pain relief is a problem.
Neck pain with no history of injury
There are many degenerative, inflammatory and mechanical causes of neck pain, and other illnesses may refer pain to the neck. Patients with such problems require a medical assessment, and, perhaps, the exclusion of a serious condition. Refer such patients in accordance with the urgency of the situation and your local policies.
Torticollis or wry neck
Torticollis is a description of a clinical appearance rather than a diagnosis, and it should be treated with caution. The cervical spine is twisted, muscle spasm is present and the patient cannot straighten the head. This may be a non-specific response to something wrong in the neighbourhood of the spasm. In the absence of a clear history of injury, keep an open mind about what that might be. Infection and neoplasm are among the possible causes. The problem is commonest in young adult women, and the usual history is of waking with a sudden pain in the neck. The neck is usually twisted away from the painful side (this is more marked in some cases than others), and attempts to move it back will hurt and feel impeded. There are usually no neurological deficits. Corrigan & Maitland (1998) ascribe the cause, tentatively, to a zygapophyseal joint derangement. They think that the youth of the typical patients makes a degenerative disc problem unlikely. They recommend physiotherapy to treat it.
Neck injuries in children
Children can suffer unstable ligament injuries and fractures to the spine. The pattern of injury is similar to that of adults when the child is near to full growth. In younger children, the difference in physical proportion, larger heads and relatively short, weak necks, means that injury occurs at the upper part of the neck, at C1 and 2, with fractures often of the odontoid peg. A severe mechanism, especially when the child has marked pain, stiffness and spasm should be taken seriously. See Box 4.5 on clearing a child’s neck.
Box 4.5
• Alert asymptomatic children with normal examination can be cleared without X-ray
• Children with C-spine signs require X-ray (pain, tenderness, restricted ROM, alterations in limb function)
• Children with impaired consciousness (head injury) require careful assessment and ?MRI scan as well as X-ray
• Spinal cord injury without radiological abnormality happens to children because there is less bone and more ligament laxity in the spine. The spine can sublux, damage the cord, and reduce to a normal position
The flexibility of a child’s spine may permit a serious injury to the spinal cord with no fracture, a phenomenon named SCIWORA (spinal cord injury without radiological abnormality). The mechanism will usually be severe: a road traffic accident or a fall from a height of 5 metres. If a child has suffered a mechanism which could produce neck injury, such as a significant head, trunk or spine injury, leg fractures, or if the patient has neck pain, radiating pain or neurological deficits, the neck should be immobilised in a hard collar with sandbags to position the head until a full assessment can be carried out (Box 4.6).
Box 4.6
• SCIWORA happens to children because there is less bone and more ligament laxity in the spine. The spine can sublux, damage cord, and reduce to a normal position
• The signs may not be present on examination, and a history of previous signs is important
• Usually patient is < 8 years. If in doubt, keep immobilised. May need MRI scan
• Older children are nearer to the adult pattern of injury with lower C-spine presentations
A child with torticollis should be seen by a doctor. A local infection (such as tonsillitis) should be ruled out. Atlanto-axial rotatory fixation (AARF) is a traumatic, fixed spinal rotation at C1 and C2, which requires early treatment. Other reasons for torticollis include congenital problems and minor injury (Box 4.7).
Box 4.7
• Back of the head tilts towards affected side and chin rotates to other side, caused by contracted sternocleidomastoid on affected side caused by a minor injury to head or shoulder. Treat symptoms
• Inflammatory disorders (retropharyngeal abscess and mastoiditis are serious but uncommon) can cause torticollis. Treat underlying cause
• Atlanto-axial rotatory fixation is the atlas (C1) locking in a turned position in relation to axis (C2). X-rays required. May need traction
The shoulder
The function of the arm is to deliver the hand to where we want it in the position which is best suited to our intention. Each of the main joints in the arm, and the structures which lie around them, has its own contribution to make to this activity.
The shoulder is not actually a joint, although it is often referred to as though it is: it is a group of joints whose common identity is based on a shared purpose. It connects the arm to the trunk and provides the bone, muscle and joint structures which allow the hand to be placed to the front and to the side to the limit of the length of our arms. We can also combine rotation with other movements, to reach behind our backs. These are clumsier movements than those to the front but they still allow us to touch any part of our bodies with our hands.
The human shoulder is adapted for mobility compared to the same structure in quadruped mammals. The chest is wider and the bony girdle projects more to the side, throwing the limbs outwards from the trunk. The muscles are larger. There is also a bigger difference between the bones of upper and lower limb than is found in a four legged creature. This is seen most clearly in the bones of the forearm.
The ways in which the shoulder tends to get injured suggest that these adaptations have only been partly successful. We are well designed to hold our hands comfortably to the front, where our eyes can see them. Much of our ordinary activity occurs in this position. Mobility far beyond this is present, but movement in the further reaches of the range, especially when the arm is held above shoulder level, causes stress and compression of delicate tissues between the bony surfaces of the humerus and the shoulder girdle. This can result in acute inflammation and degeneration and sudden rupture of important muscles. The main joint in the shoulder, the glenohumeral, is very shallow. This allows the freedom of movement which the humerus requires but the joint is unstable and it often dislocates.
Recurring patterns of shoulder pain and disability are therefore often linked to ‘impingement’ of muscles and other tissues between bone surfaces, rupture of the muscles of the rotator cuff and dislocation. Violent injuries will often cause fractures, most often of the proximal humerus and the clavicle, as well as dislocation of the glenohumeral and the acromioclavicular joints.
Anatomy
The dynamic relationship of the arm to the trunk is established by a bony girdle the main feature of which is mobility rather than stability. Such stability as the shoulder has is maintained by soft tissues, muscles, ligaments and capsular tissues.
The bones of the shoulder girdle are the scapula, the clavicle and the humerus. The scapula articulates with the chest wall at the back (the scapulothoracic joint), the clavicle laterally (the acromioclavicular joint) and the humerus, also laterally (the glenohumeral joint) (Figure 4.6). In addition, the clavicle articulates at its medial end with the sternum (the sternoclavicular joint).
 |
| Figure 4.6 • |
The scapula
The scapula is a triangular plate of cupped bone, with its concave anterior surface lying on the wall of the posterior thorax between the second and seventh ribs (Figure 4.7). It is attached to the trunk by muscles only (the term ‘scapulothoracic joint’ is used for this relationship, but there is no synovial joint between the ribs and shoulder blades). The apex of the triangle points downwards. A prominent bony ridge, called the spine of the scapula (a visible and palpable landmark on the upper back), crosses the dorsal surface of the scapula from high on its medial border to the superior, lateral corner of the bone, where it expands to become the acromion process (process means bony projection). This process articulates with the lateral end of the clavicle at the synovial acromioclavicular joint.
 |
| Figure 4.7 • |
The dorsal surface of the scapula is divided by the spine into a small supraspinous fossa (meaning, the hollow above the spine), and a larger infraspinous fossa (hollow below the spine). The front surface of the scapula forms a single hollow called the subscapular fossa. Many of the muscles of the shoulder girdle are attached to these surfaces. At the acromial angle of the scapula, slightly inferior to the bony arch, two important structures are found. The glenoid fossa is the shallow socket which articulates with the head of the humerus to form the shoulder joint. The coracoid process is a bony hook which points forwards and offers attachment for muscles and ligaments. It lies above the glenoid fossa, in the shelter of the acromion process. The bony arch over the shoulder is reinforced by the coracoacromial ligament, which crosses from the acromion to the coracoid process.
The scapula has a large repertoire of movements and contributes much to the mobility of the shoulder. It can be moved straight up and down, it can be adducted and abducted and it can rotate so that the glenoid fossa faces up or down. This allows the arm to move up and down and forwards and backwards as an integral unit. It also contributes internally to shoulder movement. Flexion and abduction are not simply glenohumeral movements. When the shoulder is abducted, a movement which has a total range of 180 degrees, the first 90 degrees occur at the glenohumeral joint, then the scapula rotates laterally and upwards, carrying the arm for another 60 degrees, and the glenohumeral joint takes over again for the final 30 degrees. It is important, when assessing shoulder movement, to observe the scapula.
The acromioclavicular joint
The acromioclavicular joint forms the bony arch which covers the shoulder joint proper. The joint has, in addition to its own capsule, the reinforcement of the coracoclavicular ligament, a two-part ligament made up of the conoid and trapezoid ligaments, which anchors the clavicle to the coracoid process of the scapula. No muscles cross this joint and its movement is passive only. The joint moves to allow movements of the scapula laterally and medially round the chest wall, up and down, and to allow scapular rotation when the shoulder is flexed.
The clavicle
The clavicle, seen from above, is a bone with curves following a long, flattened S-shape from the sternoclavicular joint, medially, to the acromioclavicular joint at its lateral end. It is superficial and forms a very distinctive dividing line between neck and chest. The clavicle braces the arm at the distance from the trunk which is necessary for it to have freedom of movement.
The sternoclavicular joint
The synovial sternoclavicular joint is the only point where the shoulder girdle is fixed to the trunk. Like the acromioclavicular joint, it has no capacity for active movement because no muscles cross it. It permits the clavicle to angle up and down, and forwards and backwards, and to rotate to a limited extent on its own axis (a movement which is initiated by rotation of the scapula).
The humerus
The humerus is the long bone of the upper arm (Figure 4.8). At its proximal end its rounded head, tilting up and backwards, articulates with the glenoid fossa of the scapula to form the glenohumeral joint. The head is separated from the tubercles of the humerus by the anatomical neck. There are two tubercles (a tubercle is a rounded bony projection for the attachment of muscles), which crown the top of the shaft of the humerus. The greater tubercle is just lateral to the head of the humerus. The lesser tubercle is on the anterior aspect of the humerus under the anatomical neck. Between the tubercles is the intertubercular sulcus (sulcus means groove) also called the bicipital groove. The tendon of the long head of the biceps muscle lies in this groove. The humerus narrows below the tubercles, at the surgical neck, and continues as the shaft of the bone.
 |
| Figure 4.8 • |
The glenohumeral joint
The glenohumeral or shoulder joint is an unstable ball and socket joint. The glenoid fossa is shallow but slightly deepened by a fibrocartilaginous rim, the glenoid labrum. The capsule of the joint passes round the anatomical neck of the humerus and is strengthened in front by three ligaments: the superior, middle and inferior glenohumeral ligaments. The capsule is also reinforced by the insertion around it, on the humerus, of the tendons of four scapular muscles, known collectively as the rotator cuff (Figure 4.9). These muscles are supraspinatus, which abducts the shoulder, infraspinatus and teres minor, which are lateral rotators of the shoulder, and subscapularis, which medially rotates the shoulder. They can be remembered by the acronym SITS.
 |
| Figure 4.9 • |
The tendons of the supraspinatus muscle and the long head of the biceps pass over the humerus and under the bony arch of the girdle. Between the tendons and the bone, lies the subacromial bursa, to minimise friction. These soft tissues are vulnerable to various forms of degeneration, inflammation and trauma because they are liable to compression, or impingement, between two mobile bony surfaces. This can be aggravated if the subacromial space is narrowed for any reason (such as the formation of osteophytes) or if the soft tissues swell.
Movement at the shoulder
Box 4.8 gives the movement statistics for the shoulder.
Box 4.8
Capsular pattern restriction in three movements, the largest being lateral rotation, the next abduction, and the least is medial rotation.
Capsular pattern restriction in three movements, the largest being lateral rotation, the next abduction, and the least is medial rotation.
• Joint positions loose packed is 60° abduction and 30° horizontal adduction; close-packed position is in combined full abduction and external rotation, and in combined full extension and internal rotation.
• Flexion 0–180°; endfeel firm; capsule stretching.
• Extension 0–60°; endfeel firm; capsule stretching.
• Abduction 0–180°; endfeel firm; capsule stretch.
• External rotation 0–90°; endfeel firm; capsule stretch.
• Internal rotation 0–70°; endfeel firm; capsule stretch.
Examination
Every shoulder examination where there is no history of direct trauma to the shoulder should begin with an assessment of neck movement (see Box 4.9). If neck movement triggers or worsens the patient’s pain, a problem at the neck is likely and must at least be excluded.
Box 4.9



 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

Ask the patient to expose both shoulders. Assess distal sensation and circulation:
• l LOOK at the neck.
• Look and compare the shoulders, front, back and sides.
• Is there asymmetry or wasting?
• Is there redness, swelling bruise or deformity?
• l FEEL the main landmarks.
• Feel the cervical spine.
• Feel the anterior structures, the sternoclavicular joint, clavicle, acromioclavicular joint and the coracoid process.
• Feel the upper humerus, the greater and lesser tuberosities, the bicipital groove and the insertion of the supraspinatus.
• Feel the scapula. Find its borders and the superficial ridge of its spine.
• l MOVE
• l Assess ACTIVE NECK MOVEMENTS (see Figure 4.5). Do they cause the patient pain?
• Observe the scapula during shoulder flexion. It contributes 60° of the upper part of the movement by rotating and tilting the glenoid upwards.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access