14 The heart and blood vessels
The heart
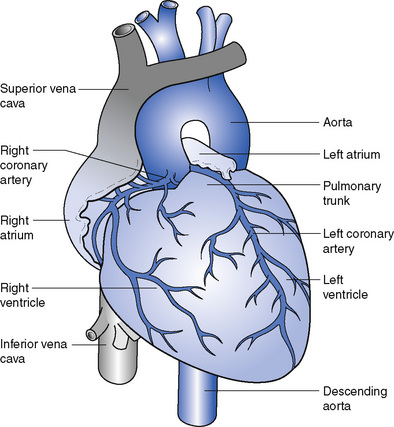
The heart is a hollow, muscular, cone-shaped organ (Fig. 14.1). It lies between the lungs in an area called the mediastinum, behind the body of the sternum with two-thirds of its bulk on the left side. The circular base of the cone is directed upwards and to the right and the apex points downwards, forwards and to the left. It is usually on the level of the fifth intercostal space about 9 cm from the midline. The heart measures about 12 cm from base to apex and about 9 cm in width; it is about 6 cm thick.
General structure
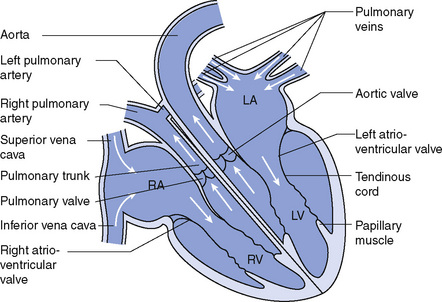
The heart is divided from base to apex by a muscular partition called the septum. The two sides of the heart have no communication with each other in health. Additionally, each side is subdivided into an upper and lower chamber. The upper chamber on each side, the atrium, is smaller and is a receiving chamber into which the blood flows through veins. The lower chamber, the ventricle, is the discharging chamber from which the blood is driven into the arteries. Each atrium communicates with the ventricle below it on the same side of the heart through an opening, guarded by a valve called the atrioventricular valve (Fig. 14.2).
Valves
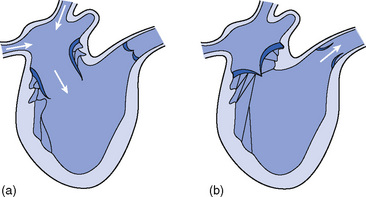
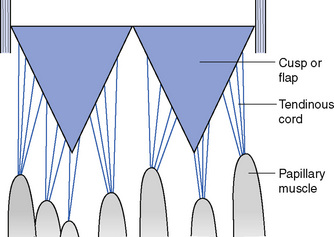
The right atrioventricular (or tricuspid) valve lies between the right atrium and the right ventricle. It consists of three triangular flaps or cusps, each consisting of a double layer of endocardium strengthened with fibrous tissue. The undersurface of the cusps provides attachment for a number of fine, tendinous cords, called the chordae tendinae, which originate in the papillary muscles in the wall of the ventricle. When the ventricle contracts, the blood is pushed back towards the atrioventricular opening but is prevented from entering the atrium by the cusps of the valve, which close because of the increased pressure in the ventricle. The contraction of the papillary muscles exerts tension on the chordae tendinae, which prevent the valve cusps from being carried into the right atrium (Figs 14.3 and 14.4).
The left atrioventricular valve is also called the mitral valve (due to its resemblance to a bishop’s mitre) (Fig. 14.5). The structure is similar to that of the right atrioventricular valve. It prevents the backflow of blood into the left atrium during contraction of the left ventricle.
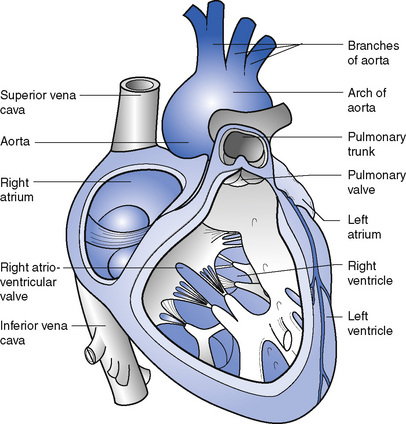
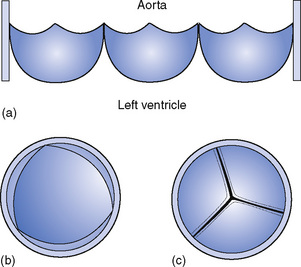
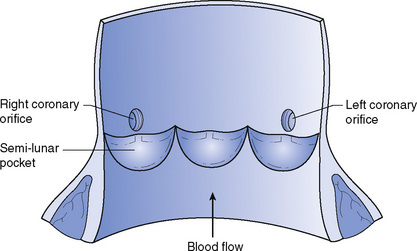
The aortic valve consists of three cusps, which surround the entrance into the aorta from the left ventricle (Figs 14.6 and 14.7). The cusps are half-moon-shaped and are fixed by their curved edges to the wall of the aorta, the straight edge being free so that pockets are formed facing into the aorta. As the blood flows from the left ventricle into the aorta the cusps lie flat against the vessel wall; as the ventricle relaxes the pockets fill with blood and bulge out, meeting in the centre and blocking the opening completely, thus preventing blood flowing back into the ventricle. The coronary arteries, which supply the heart muscle with oxygenated blood, arise from the aorta just above the attached edges of the cusps of the aortic valve.
Function
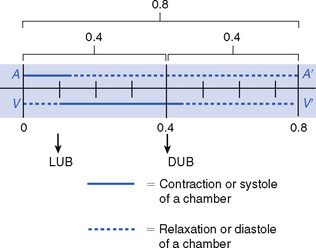
The heart contracts about 70–80 times each minute throughout life, though the rate varies with age, emotion, exercise and other influences. Each beat is a cycle of events that lasts about 0.8 second (Fig. 14.8).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree