The Healthcare Industry
Learning Objectives
1. Define, spell, and pronounce the terms listed in the vocabulary.
2. Identify the ancient cultures that contributed a major portion of our medical terminology.
3. Distinguish between and describe the staff of Aesculapius and the caduceus.
4. Explain the philosophy behind the phrase “physicians must learn to despise money.”
7. Explain the roles of the national health organizations.
9. Discuss the various types of ambulatory care.
12. Understand both the allied health professions and how they relate to medical assisting.
Vocabulary
advent Coming into being or use.
ambulatory (am′-bu-la-to-re) Able to walk about and not be bedridden.
amenities Things that contribute to comfort, enjoyment, or convenience.
case management The process of assessing and planning patient care, including referral and follow-up, to ensure continuity of care and quality management.
cited Quoted by way of example, authority, or proof or mentioned formally in commendation or praise.
complementary and alternative medicine (CAM) A group of diverse medical and healthcare systems, practices, and products that are not generally considered part of conventional medicine. Complementary medicine is used in combination with conventional medicine (allopathic or osteopathic); alternative medicine is used instead of conventional medicine.
dissection (di-sek′-shun) The separation into pieces and exposure of parts for scientific examination.
fermentation (fur-men-ta′-shun) An enzymatically controlled transformation of an organic compound.
indicted (in-di′-ted) Charged with a crime by the finding of a jury according to due process of law.
innate Existing in, belonging to, or determined by factors present in an individual since birth.
innocuous (i′-nuh-kyu-wus) Having no effect, adverse or otherwise; harmless.
integrated delivery system (IDS) A network of healthcare providers and organizations that provides or arranges to provide a coordinated continuum of services to a defined population and is willing to be held clinically and fiscally accountable for the clinical outcomes and health status of the population served.
mysticism The experience of seeming to have direct communication with God or ultimate reality.
peer review organizations (PROs) Groups of medical reviewers contracted by the Centers for Medicare and Medicaid Services (CMS) to ensure quality control and the medical necessity of services provided by a facility.
philanthropist (fu-lan′-thruh-pist) An individual who makes an active effort to promote human welfare.
putrefaction (pyu-truh-fak′-shun) Decomposition of animal matter, which results in a foul smell.
robotics Technology dealing with the design, construction, and operation of robots in automation.
staff privileges The permission granted by a facility to a healthcare professional to practice in that facility.
subluxations (suh-bluk-sa′-shuns) Slight misalignments of the vertebrae or a partial dislocation.
teleradiology The use of telecommunication devices to enhance and improve the results of radiologic procedures.
Scenario
Carlos Santos, CMA, is a medical assisting instructor with 10 years’ experience in the clinical area. He worked for a group of family practitioners and for an allergist during his career as a medical assistant before becoming an instructor. Mr. Santos believes that it is very important to give his students an overview of the history of medicine early in their training. He knows that it is exciting to show them the progress of medicine and to introduce students to the pioneers who contributed to the field. This helps the student to understand where he or she fits into the whole picture as a medical assistant. Often Mr. Santos assigns the students a short report on one person who played a role in the progress of medicine. He finds that this is a good way to encourage students to use the Internet and to conduct research right from the start of their training; also, the students get a chance to grow more comfortable speaking in front of a group when they give their reports in class. Mr. Santos knows that his students will develop an appreciation for those who contributed to the medical profession, which will influence their own dedication to both peers and patients.
Mr. Santos knows that his students must recognize the different members of the healthcare team and their responsibilities. Once the students begin their externship or practicum, they will be able to work effectively with each person in the facility and understand each one’s role in the treatment of patients. Mr. Santos also introduces them to the current types of facilities available for patient care on both a national and a local level. The knowledge the students gain about the different areas of patient care will be useful once they graduate and begin working in a healthcare facility. All of these skills will make Mr. Santos’ students more versatile and valuable to their eventual employers.
While studying this chapter, think about the following questions:
• What recent events could be included as groundbreaking discoveries in medicine?
• How can the individual medical assistant contribute to the progress of medicine in today’s world?
The growth of today’s healthcare industry seems unstoppable. Thanks to modern technologic advances, medicine speeds forward faster than ever in its quest to improve the health of humankind. Modern advances, such as telemedicine, are experiencing significant growth, and the images produced with teleradiology have vastly improved in their resolution. Robotics is assisting healthcare professionals in surgery and even delivers drugs to hospital floors using laser sensors. Education in medicine has grown exponentially: computers, the Internet, and video have enabled an instructor in New York to communicate with a student in Los Angeles. The key to this technology lies in the development and widespread use of elaborate information systems that have revolutionized the way medicine is practiced today. Technology is advancing at an astounding rate; the healthcare environment of the future is barely imaginable. This chapter looks back at the history of medicine, gazes at its present, and glances toward its future.
The History of Medicine
Medical Language and Mythology
Today’s medical professional uses words with origins stemming from the romance and fantasy of classical and ancient languages. The study of anatomy reaches back to the dawn of recorded history. Today’s modern terms often are similar to their original versions. Some terms are inaccurate when translated literally, because the ancients did not fully understand bodily functions. The word artery, for example, which comes from the Greek word arteria, literally means “a windpipe.” The early Greeks believed that the arteries carried air, not blood. Greek and Roman mythologies have contributed a major portion of our medical terminology, but we have also borrowed liberally from Arabic, Anglo-Saxon, and Germanic sources. Several terms originate from the Bible.
The human head rests on the first cervical vertebra, which is called the atlas. Atlas was the famous Greek Titan who was condemned by Zeus to bear the heavens on his shoulders. Achilles’ mother held him by the heel as she dipped him into the river Styx so that he would become invulnerable. However, his heel was not immersed, and he later died from a wound in that area. Achilles heel is a common expression used today to indicate a point of weakness. Aphrodite, the Greek goddess of love and beauty, is the source of the name for drugs used to enhance sexual arousal, called aphrodisiacs. The equivalent Roman goddess of love, Venus, is associated with lustful desires. A portion of the female anatomy, the mons veneris (mons pubis), and venereal diseases were named after her.
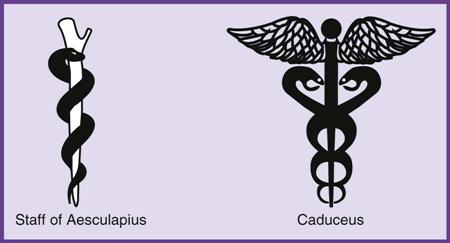
Aesculapius, the son of Apollo, was revered as the god of medicine. The early Greeks worshiped the healing powers of Aesculapius and built temples in his honor where patients were treated by trained priests. His daughters were Hygeia, goddess of health, and Panacea, goddess of all healing and restorer of health. Our modern word hygiene has its origin in Hygeia, and the modern meaning for panacea is “a remedy for all ills and difficulties.” The staff of Aesculapius is a common medical icon. It depicts a serpent encircling a staff and signifies the art of healing. The staff of Aesculapius has been adopted by the American Medical Association as the symbol of medicine. The mythological staff belonging to Hermes, the messenger of the gods, is the caduceus, which was thought to have magical powers. The caduceus is a winged staff encircled by two serpents. This icon is the medical insignia of the U.S. Army Medical Corps, although it often is misused as a symbol of the medical profession (Figure 2-1).
Medicine in Ancient Times
Although religious and mythological beliefs were the basis for care for the sick in ancient times, evidence suggests that drugs, surgery, and other treatments based on theories about the body were used as early as 5000 BC. In the well-developed societies of the Egyptians, Babylonians, and Assyrians, certain men acted as physicians and used the little knowledge they had to try to treat illness and injury.
Moses presented rules of health to the Hebrews in approximately 1205 BC. He was the first advocate of preventive medicine and is considered the first public health officer. Moses knew that some animal diseases could be passed to humans and that contamination existed; therefore a religious law was developed forbidding humans to eat or drink from dirty dishes. The people of that era believed that doing so would defile their bodies and they would lose their souls.
Hippocrates, known as the Father of Medicine, is the most famous of the ancient Greek physicians (Figure 2-2). He was born in 450 BC on the island of Cos in Greece. He is best remembered for the Hippocratic Oath, which has been administered to physicians for more than 2,000 years. Hippocrates is credited with taking mysticism out of medicine and giving it a scientific basis. During this period of history, most believed that illness was caused by demonic possession; for the illness to be cured, the demon had to be removed from the body. Hippocrates’ clinical descriptions of diseases and his volumes on epidemics, fevers, epilepsy, fractures, and instruments were studied for centuries. He believed that the body had the capacity to heal itself and that the physician’s role was to help nature. He described four “humors”—blood, phlegm, yellow bile, and black bile—that he believed must be in balance for the body to maintain a healthy state.
Galen was a Greek physician who migrated to Rome in AD 162 and became known as the Prince of Physicians. He is said to have written more than 500 treatises on medicine. He wrote an excellent summary on anatomy as it was known at the time, but his work was faulty and inaccurate, because it was largely based on the dissection of apes and swine. He is considered the Father of Experimental Physiology and the first experimental neurologist. He was the first to describe the cranial nerves and the sympathetic nervous system, and he performed the first experimental section of the spinal cord, producing hemiplegia. Galen was a champion of medical ethics; he thought that physicians “must learn to despise money,” and that if a physician was interested in profit, he was not serious in his devotion to the art of medicine. Galen’s beliefs about monetary profit from medicine parallel the views of many modern healthcare professionals, who understand the nature of the healthcare crisis the world faces today. Although much of what he believed about the body was incorrect, Galen’s teachings remained intact until human dissections began and physicians were able to visualize exactly what was inside the human body.
Because both Hippocrates and Galen were highly respected, the authority of their observations went unquestioned. This had a negative effect on the progress of science throughout the Dark Ages and well into the sixteenth century. Their theories and descriptions were considered immutable principles; therefore, few physicians were innovative and curious enough to challenge them. Those who did experiment in medicine were scorned by their colleagues, and physicians continued to use methods that were at best ineffectual or innocuous and at worst harmful to the patient. However, the establishment of universities led to a study of theories of disease rather than observation of the sick.
Early Development of Medical Education
Medical knowledge developed slowly, and distribution of such knowledge was poor. Before the printing press was invented in the middle of the fifteenth century, very little exchange of scientific knowledge and ideas occurred; scientists were not well informed about the investigations of other scientists. The printing press allowed books to be distributed faster and over a widespread area.
In the seventeenth century, European academies or societies were established, consisting of small groups of men who met to discuss subjects of mutual interest. The academies provided freedom of expression that, with the stimulus of exchanging ideas, contributed significantly to the development of scientific thought. One of the earliest of the academies was the Royal Society of London, formed in 1662. The development of communication during this era was important, and these societies contributed to the exchange of information.
In the United States, medical education was greatly influenced by the Johns Hopkins University School of Medicine in Baltimore, Maryland, established in the early 1890s. The school admitted only college graduates with at least one year’s training in the natural sciences. The clinical education at Johns Hopkins was superior, because the school partnered with Johns Hopkins Hospital, which had been created expressly for teaching and research by members of the medical faculty.
The earliest medical school accreditation resulted from a report published by Abraham Flexner. He received a grant from the Carnegie Foundation Commission to study the quality of medical colleges in the United States and Canada. His report, called the Flexner Report, resulted in the closure of many low-ranking schools and the upgrading of others. These events legitimized medical education and opened new doors for many individuals to the world of medicine.
Early Medical Pioneers
Andreas Vesalius (1514-1564) was a Belgian anatomist known as the Father of Modern Anatomy (Figure 2-3). At the age of 29, he published his great De Corporis Humani Fabrica, in which he described the structure of the human body. This work marked a turning point by breaking with the traditional belief in Galen’s theories. Vesalius introduced many new anatomic terms, but because of his radical approach, he was subjected to persecution by his colleagues, teachers, and pupils.
Other important advances and discoveries took place throughout the world. Gabriele Fallopius (1523-1562), an Italian student of Vesalius, also was an accurate dissector. He described and named many parts of the human anatomy. He named the fallopian tubes after himself and also named the vagina and placenta. In 1628 English physician William Harvey (1578-1657) announced his discovery that the heart acts as a muscular pump, forcing and propelling the blood throughout the body. He revealed that the blood’s motion is a continuous cycle. He based his conclusion on his experimental vivisection, ligation, and perfusion, as well as brilliant reasoning. Harvey’s writings were recognized in Germany before the English permitted their publication at home. Modern England considers Harvey its medical Shakespeare.
The unseen world of microorganisms was first revealed by Anton van Leeuwenhoek (1632-1723), a Dutch linen draper and haberdasher. He ground more than 400 lenses during his lifetime, some of which were no larger than a pinhead. In the grinding process, Leeuwenhoek learned how to use a simple biconvex lens to magnify the minute world of organisms and structures never before seen. Leeuwenhoek was the first ever to observe bacteria and protozoa through a lens, and his accurate interpretations of what he saw led to the sciences of bacteriology and protozoology.
Marcello Malpighi (1628-1694) was born near Bologna, Italy, and attended the University of Bologna, where he earned a doctorate in both medicine and philosophy. He pioneered the use of the microscope in the study of plants and animals. Microscopic anatomy became a prerequisite for advances in physiology, embryology, and practical medicine. In 1661 he described the pulmonary and capillary network connecting the smallest arteries with the smallest veins. This was one of the most important discoveries in the history of science, and it validated Harvey’s work. Malpighi is commonly regarded as the first histologist.
Medical Advances in the Eighteenth and Nineteenth Centuries
English scientist John Hunter (1728-1793) is known as the Founder of Scientific Surgery. An army surgeon, he became an expert on gunshot wounds and experimented with tissue transfer. His surgical procedures were soundly based on pathologic evidence. He was the first to classify teeth in a scientific manner, and he introduced artificial feeding by means of a flexible tube passed into the stomach. He provided a classic description of the syphilitic chancre, which sometimes is called a hunterian chancre. During his studies of venereal diseases, he inoculated himself with what he thought was gonorrhea, but instead he acquired syphilis. His results in this study actually caused confusion in the medical community, because he mistakenly thought that gonorrhea was a symptom of syphilis. This misconception was not corrected until the beginning of the twentieth century. His collection of anatomic and animal specimens formed the basis for the museum of the Royal College of Surgeons. Hunter is considered the Founder of Scientific Surgery, and today, the John Hunter Hospital in Australia serves more than 600 inpatients and 1,000 outpatients a day.
Edward Jenner (1749-1823) was a student of John Hunter and a country physician from Dorsetshire, England. He is considered one of the immortals of preventive medicine for his development of the smallpox vaccine. While Jenner was serving as an apprentice, he assisted in treating a dairymaid. Smallpox was mentioned, and she commented, “I cannot take that disease, for I have had cowpox.” Smallpox at that time was a deadly pandemic. Jenner observed that those who had contracted cowpox never contracted smallpox. Later, as a practicing physician, Jenner continued investigating the relationship between cowpox and smallpox almost obsessively, but the medical society members grew bored with his obsession and threatened to expel him from their ranks. On May 14, 1796, Dr. Jenner took purulent matter from a pustule on the hand of Sarah Nelmes, a dairymaid, and inserted it through two small superficial incisions into the arm of James Phipps, a healthy 8-year-old boy. This was the first vaccination. Phipps’ vaccination kept him safe from the dreaded disease, and Jenner’s method of vaccination spread throughout the world. Today smallpox has been eradicated worldwide as a result of a planned program of global vaccination.
Austrian physician Leopold Auenbrugger (1722-1809) developed the use of percussion in diagnosis. Although scorned and ignored by his contemporaries, his techniques later made him famous and are still used today during physical examinations. René Laënnec (1781-1826) was a French physician who developed the stethoscope in 1819. At first he used only a cylinder of rolled paper in his hands; later he used a wooden device because of its sound-conducting properties. With today’s sophisticated stethoscopes, physicians are able to hear sounds in the body, including a fetus inside the mother. Laënnec’s book, Treatise on Mediate Auscultation and Diseases of the Chest, was readily accepted and translated into many languages. The book is said to be the most important treatise on diseases of the thoracic organs ever written.
Several men of the early 1800s are remembered for their fight against puerperal fever and their concern for women’s health. Puerperal fever, an infectious disease that can be contracted during childbirth, was also called puerperal sepsis or childbed fever. The term puerperal, denoting a woman in childbed, originates from the Latin puer, “a child,” and pario, “to bring forth.”
The best known of these men was the Hungarian physician Ignaz Philipp Semmelweis (1818-1865); history has called him the Savior of Mothers. His fight against puerperal fever is a sad story of hardships. His theories were resisted by many professionals, including his instructors. Semmelweis noted that the fever often attacked women who were delivered by medical students coming straight from the autopsy or dissecting rooms. Semmelweis directed that in his wards the students were to wash and disinfect their hands before going to examine the women and deliver the children. As his theories were proved correct, Semmelweis felt an incredible guilt that doctors themselves had caused so many deaths. He died at the age of 47, ironically, from the very disease he had fought. He was infected with puerperal fever from a cut on his finger during an autopsy. His grave had hardly been closed when scientists began to understand the causes of this disease, largely as a result of the investigations of two great scientists, Louis Pasteur and Joseph Lister.
Louis Pasteur (1822-1895) was a Frenchman who did brilliant work as a chemist, but it was his studies in bacteriology that made him one of the most famous men in medical history (Figure 2-4). The title of Father of Bacteriology was bestowed on him, and he also has been honored as the Father of Preventive Medicine. Pasteur’s adventures included studying the difficulties involved in the fermentation of wine. He averted disaster in France’s critical winemaking industry by a process he developed, now called pasteurization. This achievement alone would have made him an immortal among the French. Through a process of supplying enough heat to destroy microorganisms, wine was prevented from turning to vinegar. Pasteur’s research efforts were impeded when he was stricken with hemiplegia, but after a long, difficult recovery, he was able to continue with a stiff hand and a limp.
Convinced that the infinite world of bacteria held the key to the secrets of contagious diseases, Pasteur left chemistry again to continue studying his theory. Many renowned scientists denied the germ theory of disease and devoted themselves to degrading Pasteur’s theories and experiments. In the midst of this controversy, he became involved in the prevention of anthrax, which threatened the health of cattle and sheep. Pasteur eventually was honored for his work with many other diseases, such as rabies, chicken cholera, and swine erysipelas. He devoted the last 7 years of his life to the Pasteur Institute, which was founded as a clinic for rabies treatment, a research center for infectious disease, and a teaching center. The Pasteur Institute still exists. Pasteur died in 1895, with his family at his bedside. It is said that his last words were, “There is still a great deal to do.”
Joseph Lister (1827-1912) revolutionized surgery through the application of Pasteur’s discoveries. He understood the similarity between infections in postsurgical wounds and the processes of putrefaction. Pasteur proved that these processes were caused by microorganisms. Before this time, surgeons accepted that infections in surgical wounds were inevitable. Lister reasoned that microorganisms must be the cause of infection and should be kept out of wounds. His colleagues were indifferent to his theories, because most believed infections were God-given and natural. Lister disagreed, and he developed antiseptic methods by using carbolic acid for sterilization. By spraying the rooms with a fine mist of the acid, soaking instruments in carbolic solutions, and washing his hands in a similar solution, he was able to prove his theories. He is honored as the Father of Sterile Surgery. Pasteur and Lister met after years of great mutual admiration. The meeting was filled with emotion, and it was written in Pathfinders in Medicine that “a new star should have appeared in the heavens to commemorate the event.” Medicine truly owes a deep gratitude to these two pioneers for the knowledge they imparted to the art.
Robert Koch (1843-1910) was a German physician, famous for his Koch’s Postulates; that is, his theory of rules that must be followed before an organism can be accepted as the causative agent in a given disease. He introduced many of the tools used in the laboratory, such as the culture plate method of isolating bacteria. He discovered the cause of cholera and demonstrated its transmission by food and water. This discovery completely transformed health departments and proved the importance of bacteriology in everyday life. Koch’s greatest disappointment was his failure to find a cure for tuberculosis, but in his attempt, he isolated tuberculin, the substance produced by tubercle bacteria. Its use as a diagnostic aid was of immense value to medicine. He became a Nobel Laureate in 1905.
One of Koch’s students was a German physician named Paul Ehrlich (1854-1915). He pioneered the fields of bacteriology, immunology, and especially chemotherapy. Ehrlich was only 28 when he wrote his first paper on typhoid, but his greatest gift to humanity was called his “magic bullet,” or formula 606, which was designed to fight syphilis. With the organism identified by scientists Bordet and Wasserman, Ehrlich set out to find a chemical that would destroy the organism but not harm the host, specifically, the human body. The six hundred sixth drug Ehrlich tried finally brought about healing. He called it salvarsan, because he believed that it offered humankind salvation from the disease. This endeavor also marked the beginning of the practice of injecting chemicals into the body to destroy a specific organism. In 1908 Ehrlich shared the Nobel Prize with Eli Metchnikoff, who is remembered for his theory of phagocytosis and immunology.
Crawford Williamson Long (1815-1878) was the first to use ether as an anesthetic agent. Early in 1842, a group of students would have a social gathering after chemistry lectures and inhale ether, a chemical commonly found in chemistry laboratories, as a form of amusement. Ether, an intoxicant similar to nitrous oxide, functions as a soporific, or sleep-inducing agent. However, at one of these “ether frolics,” as they were called, Dr. Long also observed that people under the influence of ether did not seem to feel pain. After considerable thought, he decided to use ether for a surgical procedure. In March, 1842, he removed a tumor from the neck of James M. Venable after placing him under the influence of ether. Dr. Horace Wells was a dentist who reported using nitrous oxide as an anesthetic in 1844. Another dentist, Dr. William T. G. Morton, reported using ether in 1846 when he extracted a tooth from a patient, and he also used the gas at Massachusetts General Hospital for a surgical procedure.
Surgeons are grateful to Wilhelm Konrad Roentgen (1845-1923), a professor of physics at the University of Wurzburg, Germany. Roentgen discovered the x-ray in 1895 while experimenting with electrical currents passed through sealed glass tubes. He was awarded the Nobel Prize in Physics in 1901. Although he called it an x-ray, history has honored him by calling it the roentgen ray. Marie and Pierre Curie discovered radium in 1898, and they were awarded the 1902 Nobel Prize in Physics for their work on radioactivity. Unfortunately, Pierre was killed 3 years later while crossing a street in a rainstorm. Marie was awarded his teaching position at the Sorbonne, a medical university in France; no woman had taught at the school in its 650-year history. In 1911 she was awarded the Nobel Prize for her discoveries of radium and polonium, the first person to receive the award twice. She died in 1934 from pernicious anemia, which was believed to have been caused by her overexposure to radiation and years of overwork.
Nineteenth Century Women in Medicine
Many women made great contributions to medicine in the early nineteenth century, at a time when women were not considered to be as capable as men outside the home environment. Florence Nightingale (1820-1910) is known as the founder of nursing and is fondly called the Lady with the Lamp (Figure 2-5). She was of noble birth, and somewhat late in life she sought nursing training in both England and Europe. By the dawn of the Crimean War in 1854, she had established a fine reputation for her work in hospital organization. She was invited by the British Secretary of War to visit the Crimea to help correct the terrible conditions that existed in caring for the wounded. She created the Women’s Nursing Service in Scutari and Balaklava. The physicians treated her and the other 38 nurses poorly until a crisis brought thousands of wounded and sick soldiers to the army hospitals. The bravery and competence of the nurses helped the doctors realize their value to the medical profession. In 1860 she founded the Nightingale School and Home for Nurses in London, which marked the beginning of professional nursing education.
Clara Barton (1821-1912), an American, began her nursing career early in life. When she was 11 years of age, her brother fell from the roof of their barn, and Clara nursed him back to health over a 2-year period. She later was a battlefield nurse and philanthropist, whose work during the Civil War led her to recognize that very poor records were kept in Washington to aid in the search for missing men who were wounded or killed in combat. Her efforts to remedy this led to the formation of the Bureau of Records. Her organization and recruitment of supplies for the wounded led to her eventual involvement with the Red Cross in the Franco-Prussian War. In 1881 she organized a Red Cross Committee in Washington, the original formation of the American Red Cross. She served as its first president, from 1881 to 1904. She retired at the age of 82, just after personally leading dangerous expeditions to help victims of fires, hurricanes, and floods. The American Red Cross remains a vital organization to this day.
Elizabeth Blackwell (1821-1910) was the first woman in the United States to receive the Doctor of Medicine degree from a medical school. She began her medical education by reading medical books and later obtained private instruction. Medical schools in New York and Pennsylvania initially refused her applications for formal study, but finally, in 1847, she was accepted at the Geneva Medical College in New York.
Lillian Wald (1867-1940), a social worker and nurse, made great contributions to medical care when she founded the Henry Street Settlement in New York City. Wald operated a visiting nurse service from this establishment. When one of her nurses was assigned to the city’s public schools in 1902, the New York City Municipal Board of Health established the world’s first public school nursing system.
Margaret Sanger (1883-1966) was born in Corning, New York, and trained as a nurse at the White Plains Hospital. She became the American leader of the birth control movement. While working among the poor in New York City, she came to understand the public’s need for information about contraception. In 1873 the federal Comstock Law declared it illegal to import or distribute any device, medicine, or information designed to prevent conception or induce abortion or to mention in print the names of sexually transmitted diseases. Nurses and physicians were legally prohibited from providing this information to their patients. In 1914 Sanger was indicted for circulating the magazine The Woman Rebel, in which she attacked the legislative restrictions of the Comstock Law. The case was dismissed 2 years later. In the same year, she established the first American birth control clinic; this led to her arrest, conviction, and incarceration in the county jail. She continued her work, and after World War II, she successfully advocated research into hormonal contraception because of the newfound concern about population growth. This research ultimately led to development of the birth control pill. When the Planned Parenthood Federation of America was formed in 1941, she was named honorary chairperson.
Modern Milestones in Medicine
In recognition of the achievements of scientists of the past, Sir Isaac Newton spoke of our innovative ability in the medical field. He humbly said, “If I have seen a little further than others, it is because I have stood on the shoulders of giants.” Great strides in medicine occurred in the twentieth century, and technology began to advance rapidly. Medical leaders continued their contributions, and knowledge, treatment, and research grew by leaps and bounds.
Walter Reed, a U.S. Army pathologist and bacteriologist, proved that yellow fever was transmitted by the bite of a mosquito. Individuals with diabetes should be grateful to Sir Frederick Grant Banting, a Canadian physician who isolated insulin for treatment, along with Charles Herbert Best, a Canadian physiologist. In 1928 Sir Alexander Fleming discovered penicillin accidentally while researching influenza and working with staphylococcal bacteria. He found a substance in mold that prevented the growth of bacteria even when the substance was diluted 800 times.
Cardiologist Helen Taussig and surgeon Alfred Blalock explored the health issues of children born with cyanosis resulting from a malformed heart. Dr. Taussig collaborated with Dr. Blalock to develop a lifesaving operation for these children, called “blue babies.” History often omits the contributions of Vivien Thomas, an African-American man who was Dr. Blalock’s surgical research technician at Johns Hopkins Hospital. Thomas was a former carpenter who constructed several of the medical instruments used in the Blalock-Taussig procedure. Thomas actually created the blue baby condition in dogs, on which he regularly practiced the surgical procedure. When Dr. Blalock and Dr. Taussig performed the first blue baby operation at Johns Hopkins University, Thomas stood over Blalock’s shoulder and advised him during the procedure, because Thomas had done the surgery several more times than Blalock. This happened at a time when African-Americans were not allowed on the main floors of the hospital, much less in the surgical suite. This surgery became known as the Blalock-Taussig procedure, and although the first blue baby operation prolonged the patient’s life by only 2 months, subsequent operations were successful, and children were able to leave the hospital with the hope of a healthy life.
Jonas Edward Salk and Albert Sabin almost eradicated poliomyelitis, once the killer and crippler of thousands in the United States. Salk’s injectable vaccine was developed in 1952, and after wide-scale testing in 1954, it was distributed nationally, greatly reducing the incidence of the disease. Sabin’s live-virus vaccine, in a form that could be swallowed, became available less than a decade later.
Werner Forssmann, a German surgeon, originated a cardiac technique called catheterization that is used in the diagnosis and treatment of heart disease. Christiaan Barnard, a South African surgeon, performed the first human heart transplantation in 1967. Dr. Elisabeth Kübler-Ross, a Swiss-born psychiatrist who died in 2004, was shocked at the treatment of terminally ill patients at her hospital in New York. She wrote the best-selling book On Death and Dying, which helped professionals and laypersons alike understand the stages of grief.
Edwin Carlyle “Carl” Wood is best known for his pioneering work developing and commercializing the technique of in vitro fertilization (IVF). Although some of Dr. Wood’s work was controversial, his medical career spanned over 50 years. He wrote 23 books, 59 chapters, and over 400 papers in refereed medical and scientific journals.
Some diseases, conditions, and anatomical structures are named for the person who first discovered them or pioneered the disease. Dr. Virginia Apgar (1909-1974) founded neonatology. She developed the Apgar score, which is a method of assessing the health of newborns at the time of birth. The assessment has greatly reduced infant mortality by quickly determining whether a newborn needs immediate medical treatments. Henry Jay Heimlich, MD, is credited for the Heimlich maneuver, which uses abdominal thrusts to relieve choking. Aloysius Alzheimer (1864-1915) was a German physician who was credited with identifying the first published case of pre-senile dementia, later known as Alzheimer’s disease. Parkinson’s disease is named for Dr. James Parkinson, an English surgeon, geologist, and paleontologist. Down’s syndrome, which is a chromosomal condition caused by an extra twenty-first chromosome, was first described by British doctor John Langdon Haydon Down. Asperger syndrome was named for Hans Asperger of Austria, who wrote hundreds of publications about autism. Asperger’s is characterized by significant difficulties in social interaction along with restricted and repetitive patterns of behavior and interests. Thomas Hodgkin (1798-1866) was considered one of the most prominent pathologists of his time and pioneered preventative medicine. Dr. Hodgkin provided the first description of Hodgkin’s disease or Hodgkin’s lymphoma, characterized by the orderly spread of disease from one lymph node to another and by the development of systemic symptoms with advanced disease. Those familiar with the common diseases related to human immunodeficiency virus infection (HIV) and acquired immunodeficiency syndrome (AIDS) will recognize Kaposi’s sarcoma, a skin tumor discovered by Hungarian physician Moritz Kaposi. In the 1980s, Kaposi’s sarcoma, or KS, was determined to be caused by a viral infection and became widely known as one of the AIDS-defining illnesses.