Health care should be within reach of everyone.
After completing this chapter, you should be able to:
• Describe challenges facing health care that impact the delivery of nursing care, including:
• Reduction of costs
• Evidence-based care
• Shortage of health care professionals
• Patient safety
• Nurse staffing
• Delivery changes influenced by the 2010 Institute of Medicine Future of Nursing Report
• Trace the history of the use of nursing care delivery models.
• Consider ways to structure nursing services to improve care while reducing costs, in order to insure that health care is within reach of everyone.
The U.S. health care delivery system has been changing dramatically during the past 40 years. Economic changes around the world and the passage of the Affordable Care Act of 2010, as well as the resulting political responses, have focused the country’s attention on the need to revise the U.S. health care system to improve access and quality while reducing the delivery costs. Nurses practicing in such an environment must be comfortable with change and be willing to embrace the challenges that change brings. A first step to ensuring that your nursing practice evolves in a positive direction is to be knowledgeable about these changes.
What are some Important Challenges Currently Facing Health Care?
Cost of Health Care
High health expenditures in the United States have long been a national problem. There are a number of reasons for this continued growth in the cost of health care, including expansion of prescription of drugs and new medical technologies, as well as administrative costs. The rise in the incidence of chronic disease, which accounts for a large portion of national health care expenditures, is also a major factor. For the past 30 years, various strategies have been instituted to halt this escalation in health care costs. One of the major approaches to reduce costs has been managed care.
Managed Care
In the early 1900s, patients or their families paid the physician or the hospital directly for the care they received. As health care insurance became an employment benefit after the Second World War, third-party payers became more common. These third-party payers paid the provider an agreed-on fee for each service provided. The more the provider charged, the more the payer paid.
In the early 1980s, Medicare introduced the prospective payment system as a way of reimbursing hospitals. This marked the beginning of a movement to control health care costs. Under this system, which insurance companies soon adopted, a fixed fee was paid to the hospital according to a preset reimbursement rate for the diagnosis given at discharge. A hospital could treat a patient so that a shorter length of stay was necessary, reducing the consumption of resources. This allowed the hospital to show a greater profit or smaller loss for caring for a patient if the care was more efficient than was the prearranged rate for the diagnosis. This practice began the trend of managed care in which health care is paid at a prearranged rate rather than as billed.
In the most extreme type of managed care, called capitation, employers pay a set fee each month to an insurance company for each covered employee and dependent. This amount does not vary based on the care given. Potential patients may never need any health care, or they may require extensive hospitalizations. Regardless, the costs of care for all members of a particular employment group must be taken out of the set fee. Under this arrangement, there is incentive for the insurance company and the provider to work aggressively to keep patients healthy, because prevention or early intervention is likely to be less expensive than hospitalization. Conversely, if patients do not stay healthy or if they overuse hospitalization, the health care provider may actually lose money.
As a part of the managed care trend, health maintenance organization (HMO) plans became very popular as a form of insurance. In HMOs, an annual payment is made on behalf of the members to a group of providers who deliver all of the health services covered under the plan, including physician and hospital services. HMOs have grown, because they provide a strong incentive to avoid hospitalization, which consequently reduces costs. HMO members often appreciate the ease of using health care with an HMO, because there are fewer noncovered services and fewer forms to complete. However, the choice of providers is limited; members must use physicians who are part of the HMO network, and they may not see specialty physicians without a referral from their primary care provider.
The preferred provider organization (PPO) is another type of insurance plan designed to meet the goals of managed care. To avoid out-of-pocket expenses, members must use physicians who have agreed to provide services at a lower price to the insurer. However, members may use an “out-of-network” provider without a referral, if they are willing to pay more for that service.
What Impact Has Managed Care Had on Costs?
Initially, managed care reduced the cost of health care. However, costs have increased sharply in response to the backlash from restrictive managed care policies. Between 1999 and 2007, employer-sponsored health insurance premiums increased by 199%, placing cost burdens on both the employers and the workers (Kaiser Family Foundation, 2007).
Given the complexity of the issues surrounding the costs of health care, it is very difficult to say conclusively that managed care is effective, in part because the definition of “effective” may vary. Effectiveness can be measured by profit and loss, quality of care, and/or access to services. Improvement in one of these factors does not necessarily mean improvement in other factors. In addition, there are a number of stakeholders who must judge the effectiveness of care in any given situation, including the managed care organization, the employer, the Centers for Medicare & Medicaid Services (CMS), regulators, and providers, as well as individual patients, their significant others, and society as a whole. Since these groups often have different needs and agendas, one definition of efficient is difficult to agree upon.
Despite these efforts to reduce the cost of health care for the past 25 years, in the fall of 2013 at the Conference on the Brookings Paper on Economic Activity (BPEA), Chandra, Holmes, and Skinner noted that health care consumes nearly 18% of the U.S. gross national product (GNP), making the U.S. the world’s leader in both the level and growth rate of spending in health care. While there has been a moderation in health care spending since 2009, the authors predict that it is unlikely there will be a permanent “bending of the health care cost curve” going forward. The authors predicted that health care will grow at the level of the GDP level, plus 1.2% for the next few decades. Concern over the impact of long-term technology pipeline that could deliver new and expensive technology with very low medical or financial benefits, coupled with high labor costs will likely fuel this continued increase (Chandra, Holmes, & Skinner, 2013).
Affordable Care Act
On March 23, 2010, the Affordable Care Act (ACA) was passed, providing regulations to reduce health care costs, as well as improve access to care. On June 28, 2013, the U.S. Supreme Court rendered a final decision to uphold this health care law. The provisions of the law were implemented over a 5-year period. Table 15.1 provides an overview of the major elements of the bill and the year in which each component was introduced. At the time of publication of this book, there was considerable discussion about repealing all or parts of the ACA.
Strategies to Control Costs
Hospital care accounts for the largest share (32.1%) of health care expenditures; physician services are second, accounting for 19.9%; and prescription drugs account for 9.8% (CDC, 2014). Reducing costs in these areas will have the greatest impact on reducing total costs. Specific efforts to reduce hospital costs that impact the delivery of nursing care include case management, evidence-based practice, appropriate staffing, improving retention of staff, use of the electronic health record (EHR), and reducing patient-care errors.
Case Management
The Case Management Society of America (CMSA) notes that case (or care) managers are advocates who help patients understand their current health status, what they can do about it, and why those treatments are important. In this way, case managers guide patients through the health care delivery process and provide cohesion to other professionals on the health care delivery team. The purpose of case managers is to enable their clients to achieve goals effectively and efficiently. The role may take a variety of forms but generally includes coordination of care, communication, collaboration, and attention to the transition between levels of nursing care. Social workers and therapists may also be case managers, although how they perform their role depends on the scope of practice within their discipline. All case managers must be skilled at communication, critical thinking, negotiation, and collaboration. They must be knowledgeable about resources available to patients. The case manager not only collaborates with individual patients but also with family and other support systems of the patient.
TABLE 15.1
Components of the Affordable Care Act
Adapted from the U.S. Department of Health and Human Services. (2015). Key features of the Affordable Care Act by year. Retrieved from http://www.hhs.gov/healthcare/facts-and-features/key-features-of-aca-by-year/index.html#.
Case management is effective in providing care, but all patients do not need this intensity of interaction. To provide case management services to all patients would be wastefully expensive. Patients should be assigned a case manager only if they:
▪ Have complicated health care needs
▪ Are receiving care that is expensive as well as complicated
▪ Pose discharge planning problems
▪ Receive care from multiple providers
▪ Are likely to have significant physical or psychosocial problems
Case management may also be implemented in levels of care other than acute hospitals, particularly in some outpatient and short-term rehabilitative settings. In many ways, the roles and responsibilities of the case manager are the same regardless of the level of care in which they work. The differences in the emphasis of the role are often influenced by reimbursement.
Nurse navigator programs are a form of case management that is beginning to be more widely used to coordinate patient care. In 1990, Dr. Harold Freeman developed the first nurse navigator role at Harlem Hospital in New York in an effort to expedite diagnosis and treatment, while facilitating access to care for patients with abnormal breast screening results (Pedersen & Hack, 2010). Since that time, the role of the nurse navigator has been used in a variety of settings.
In 2005, the Patient Navigator Outreach and Chronic Disease Prevention Act authorized federal grants to hire and train patient navigators to help patients who had cancer and other serious chronic diseases to receive access to screening, diagnosis, treatment, and follow-up care. In 2006, the CMS funded six demonstration projects to help minority Medicare patients overcome barriers with screening, diagnosis, and treatment, and in 2007, $2.9 million was allocated to this program (Wells et al., 2008).
Although a large number of nurse navigator programs target care of the cancer patient, there is also an opportunity to implement this role when caring for other chronic diseases (Case, 2011). For example, publications show that health care facilities carry out nurse navigator programs for conditions such as high-risk OB care, osteoarthritis, HIV (Horstmann et al., 2010), and asthma (Black et al., 2010).
The navigator role was conceived to reduce patient barriers to care for vulnerable patients who may cope with delays in access, diagnosis, treatment, and/or fragmented and uncoordinated care. An analysis of evaluations of nurse navigator programs from 2000 to 2010 identified improved patient satisfaction, positive changes in patient attitudes and understanding of disease processes, and better patient perception of a timelier and more accessible treatment process (Case, 2011).
Disease Management
Disease management refers to multidisciplinary efforts to improve the quality and cost of care for patients suffering from chronic diseases. It involves interventions designed to improve adherence to appropriate scientific guidelines and treatments. The goal is similar to case management—to support patients with chronic diseases who may receive services from various levels of care (acute care to home-based care). However, it is a population health strategy as well as an approach to personal health.
A variety of national organizations involved with consumer health or the health care delivery system at large have supported the use of disease management strategies to improve health care. For example, the American Heart Association’s Expert Panel on Disease Management recommends the following guiding principles for disease management initiatives.
▪ The main goal of disease management should be to improve the quality of care and patient outcomes. Evaluations of disease management programs should not be based solely on their ability to reduce health care expenditures.
▪ Scientifically derived, peer-reviewed guidelines should be the basis of all disease management programs. These guidelines should be evidence based and consensus driven.
▪ Disease management programs should help increase adherence to treatment plans based on the best available evidence.
▪ All disease management efforts must include ongoing and scientifically based evaluations, including clinical outcomes.
▪ Disease management programs should exist within an integrated and comprehensive system of care in which the patient-provider relationship is central (Faxon, et al., 2004).
Although disease management shows considerable promise, significant additional attention is needed in testing and demonstrating best practices and sharing information on successful components across a variety of care settings within this evolving area.
Do Disease Management Programs Reduce the Cost of Health Care?
In 2007, the RAND Health Study reported a review of all past research (317 studies) on disease management programs related to six chronic conditions: heart failure, coronary artery disease, diabetes, asthma, depression, and obstructive pulmonary disease. The interventions ranged from prerecorded telephone reminders to home visits by medical professionals. The results showed that these programs often improved the quality of the patient’s care. However, there was no conclusive evidence that disease management programs actually saved money. The authors suggested that the breadth of the definition of disease management might influence the findings. For example, some programs may have been better than others, but there is not enough research to assess properly which program is the most effective or why it is effective. In addition, most of the studies followed patients for only 1 year, which may not be long enough to determine the long-term effect of the program (RAND Corp., 2007).
Similarly, in 2015, the Cameron Institute reviewed and analyzed available literature from the past decade on disease management programs with an eye to determining their effectiveness in the Medicaid population. Although it was somewhat challenging to extrapolate the studies’ results to a larger context, several recurring themes emerged, which provided perspective on the current state of knowledge:
▪ The robust results of many studies, across disease types, show that disease management programs were most likely to be cost-effective and improve quality of care when dealing with severely ill enrollees who are at high risk for hospitalization, near term.
▪ Self-management and monitoring were found to be especially effective. Provider education of patients was also found to be effective in increasing medication adherence, vaccination rates, and screening.
▪ Telephonic care management also was found to be effective.
▪ Physician- and pharmacist-led interventions positively influenced prescription medication adherence and attainment of guidelines for lipid and HbA1c levels (Schatz, 2008).
What Tools Are Used to Support Care Coordination?
Clinical pathways and disease management protocols are similar strategies that support the work of the coordinator of care to reduce expensive variations in care.
These pathways support the coordination and delivery of high-quality care. There are four essential elements of a clinical pathway:
▪ A timeline outlining when specific care will be given
▪ The categories of care or activities and their interventions
▪ Intermediate- and long-term outcomes to be achieved
▪ A variance record
The variance record allows caregivers to document when and why the progress of individual patients varies from that outlined in the pathway. Clinical pathways differ from practice guidelines, protocols, and algorithms, because they are used by the interprofessional disciplinary team and have a focus on quality and coordination of care for individual patients. A sample of a clinical pathway can be found in the Evolve resources.
Clinical Guidelines
Both critical pathways and disease management protocols are generally based on clinical guidelines that incorporate nationally acceptable ways to care for a specific disease. The National Heart, Lung, and Blood Institute (NHLBI), a component of the U.S. Department of Health and Human Services, defines clinical practice guidelines as “practice regulations that are systematically developed statements to assist practitioner and patient decisions about appropriate health care for specific clinical circumstances.” These recommendations include specific diagnostic and treatment options based on evidence from a rigorous systematic review and synthesis of the published literature. In short, they recommend practices that meet the needs of most patients in most circumstances; however, the clinical judgment is always required to fit the guideline to the individual patient (NHLBI, n.d.).
Clinical guidelines are typically developed by government agencies, such as the Agency for Healthcare Research and Quality (AHRQ), or an organization devoted to health promotion and disease prevention, such as the American Public Health Association and the Centers for Disease Control and Prevention. A website developed by AHRQ, in collaboration with the American Medical Association (AMA) and the American Association of Health Plans (now America’s Health Insurance Plans [AHIP]) provides a resource for clinical practice guidelines at www.guideline.gov.
Pay for Performance
Pay for performance (P4P) is increasingly being used to reduce costs and improve quality in health care. Physicians, hospitals, medical groups, and other health care providers are rewarded for meeting certain performance measures for quality and efficiencies. Disincentives, such as eliminating payments for negative consequences of care (medical errors) or increased costs, have also been proposed. An example of such disincentives includes hospitals not receiving reimbursement for care given to treat health care–associated infections (HAIs), such as catheter-acquired urinary tract infections (CAUTI) and surgical site infections (SSIs). There are several ways in which the P4P can be implemented. Chief among them is nonpayment for treatment of preventable complications such as falls and pressure ulcers (Thomas & Caldis, 2007). Although P4P continues to be considered an important approach for continuing to reduce cost while ensuring quality, there are mixed results from research regarding its effectiveness in reducing costs (Schatz, 2008; Torgan, 2013).
Evidence-Based Practice
How Do We Know That Critical Pathways and Disease Management Protocols Reflect the Latest and Best Practice?
In 2000, the Institute of Medicine (IOM) released a report, “Crossing the Quality Chasm: A New Health System for the 21st Century” (IOM, 2000). This report noted that it takes 17 years for the results of research in health care to be transmitted consistently into practice.
Evidence-based practice is the use of the current best evidence in making decisions about patient care. It flows from clinicians asking, “What is the best way to manage a particular situation?” Melnyk and Fineout-Overholt (2011) believe that evidence-based practice uses the following steps to answer clinical questions:
▪ Systematic search for the most relevant evidence to the question (What is the most relevant evidence?)
▪ Critical evaluation of the evidence found (Is the evidence logical and valid?)
▪ Your own clinical experience (Does your experience fit with the evidence?)
▪ Patient preferences and values (Will your patients accept the recommendations drawn from the evidence?)
The answers to these questions can then be implemented in practice or incorporated into critical pathways and disease management processes.
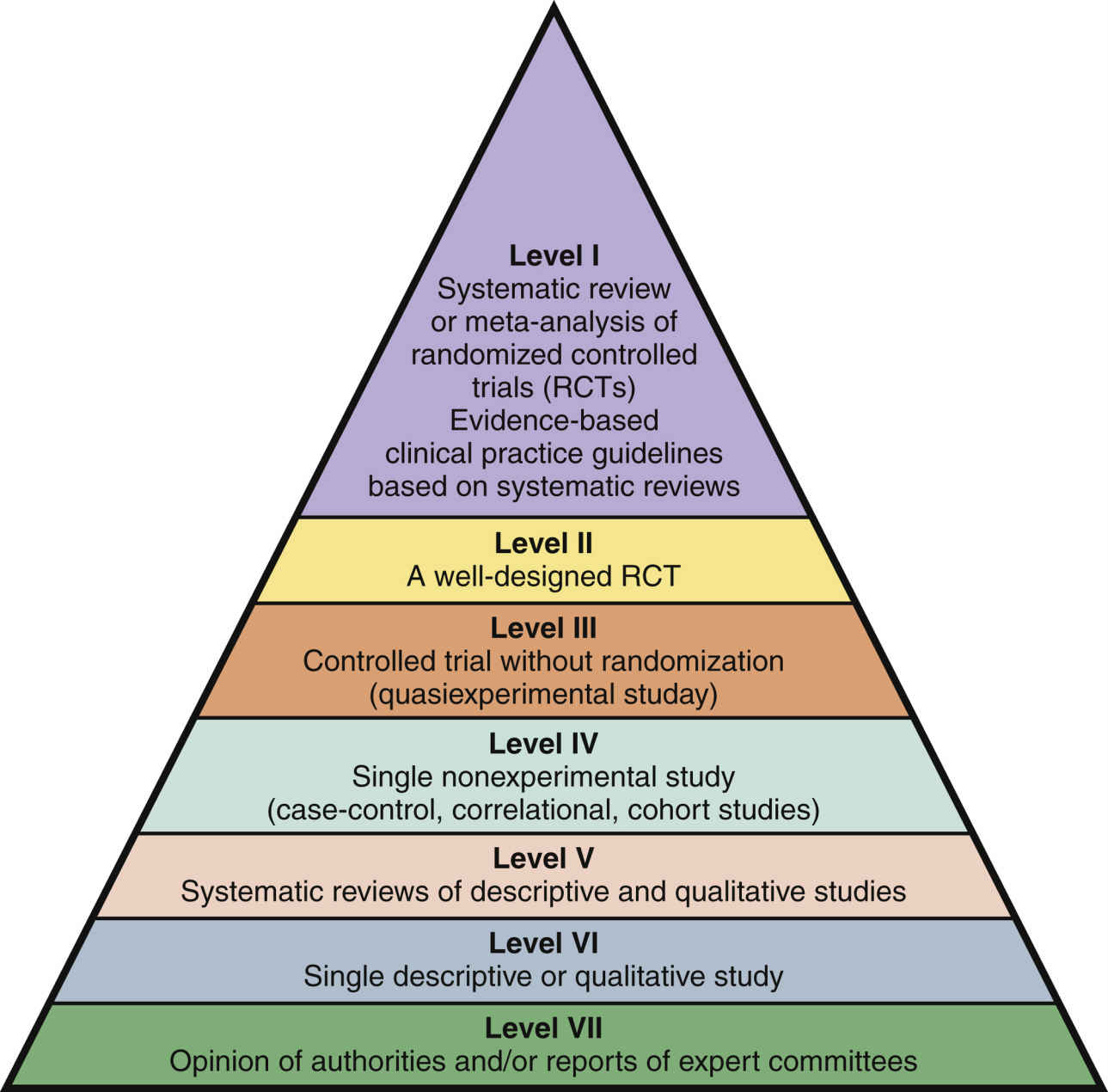
Most nurses use their own clinical experience with patient preferences and values in planning nursing care. However, searching for the evidence to address the question at hand and critically evaluating the evidence may be more difficult. Fig. 15.1 outlines a rating system to help you know how strong the evidence from research or other sources might be.
There are a number of evidence-based nursing centers around the world that provide the best available evidence to inform clinical decision making at the point of care. One of the largest is the Joanna Briggs Institute (JBI), an international not-for-profit research and development arm of the School of Translational Science based within the Faculty of Health Sciences at the University of Adelaide, South Australia, which collaborates internationally with more than 70 entities across the world (http://joannabriggs.org/) (Critical Thinking Box 15.1). See Chapter 24 for more information on how evidence-based practice affects economics. Relevant websites and online resources are listed at the end of this chapter.
Shortage of Nurses
Although hospitals and other health care organizations have experienced nursing shortages during the past 50 years, the most recent shortage, which began in 1998, seems to be the most persistent (Buerhaus, 2009). Although the United States was in a recession in 2009, Buerhaus and colleagues found that despite the easing of the nursing shortage because of the recession, the U.S. nursing shortage is projected to continue growing. According to the Bureau of Labor Statistics’ Employment Projections 2012–2022 released in December 2013, registered nursing (RN) is listed among the top occupations in terms of job growth through 2022. The RN workforce is expected to grow from 2.71 million in 2012 to 3.24 million in 2022, an increase of 526,800, or 19%. The bureau also projects the need for 525,000 replacements nurses in the workforce, bringing the total number of job openings for nurses due to growth and replacements to 1.05 million by 2022 (AACN, 2014, para 1).
According to the U.S. Registered Nurse Workforce Report Card and Shortage Forecast published in the January 2012 American Journal of Medical Quality, an ongoing shortage of nurses is predicted to spread across the country, especially in the South and West. In February 2012, the Bureau of Labor Statistics Employment Projections (2010–2012) indicated that the RN workforce is the top occupation for job growth, with 2.74 million jobs in 2010 growing to an expected total of 3.45 jobs in 2025, which is an increase of 26%. In addition, 495,500 RNs will retire or leave the workforce, resulting in a total number of job openings for RNs of 1.2 million by 2020 (AACN, 2014, para 2). This ongoing shortage of nurses will continue to impact the cost and quality of health care provided in the United States for the foreseeable future.
How Can Health Care Organizations Retain Nurses?
Retention of nurses in their place of employment is as important as recruitment. The number of nurses who retired during the Great Recession from December 2007 to June 2009 was significantly lower than predicted. As the economy improved, nurses in their 60s began to choose to reduce the amount of time they work each week or perhaps retire completely. In addition, the demands of the rapidly changing health care environment are reducing the satisfaction of nurses of all ages, which often drives a reduced retention rate in employment sites. To combat the need to change jobs frequently, administrators are emphasizing attractive compensation packages; focusing on a culture of training, including mentoring; providing constructive positive feedback; and providing recognition for excellence. Offering a variety of scheduling options to meet the needs of a variety of ages is also a popular retention strategy.
Currently, there is particular interest in providing support for novice nurses in their first job. McDonald and Ward-Smith (2012) reviewed the evaluation reports of transition programs for new graduates, including internships, externships (programs prior to graduation), and postorientation buddy programs. This review determined that the longer the intervention to support the novice nurse lasted, the higher the retention of the participants. In addition, the authors identified key elements of any orientation as
▪ Providing evaluation of baseline knowledge
▪ Inclusion of higher level skill practice
▪ Support for an experienced individual
▪ Providing of opportunities to clarify existing knowledge and expand knowledge
▪ Evaluation of individual program outcomes
Regardless of the age of the employee, addressing the negatives associated with the work environment is a key to maintaining a robust workforce.
Magnet Hospitals
Recognizing the characteristics that influence a positive work environment on nurse retention is not new. In the early 1980s, during a previous nursing shortage, the American Academy of Nursing conducted research to identify the organizational attributes of hospitals that experienced success in recruiting and retaining nurses. The American Academy of Nursing Fellows nominated 165 hospitals throughout the nation that had reputations for successfully attracting and retaining nurses and delivering high-quality nursing care. Ultimately, 41 hospitals were distinguished by high nurse satisfaction, low job turnover, and low nurse vacancy rates, even when hospitals located in the same area were experiencing nursing shortages. These hospitals were called magnet hospitals, because of their success in attracting and keeping nurses.
The Magnet Recognition Program identifies characteristics or outcomes, known as “Forces of Magnetism,” which exemplify excellence in nursing (see Box 15.1). Ten years after the identification of the original magnet hospitals, the American Nurses Credentialing Center (ANCC) established a new magnet hospital designation process, similar to accreditation by The Joint Commission (TJC). Recently, the recognition program has been expanded to provide national recognition for excellence in long-term care nursing facilities and smaller community hospitals. In the current competitive environment, receiving the magnet status may serve as a recruiting and marketing tool for hospitals, attesting to a professional work environment and quality nursing (Critical Thinking Box 15.2).
The Impact of the 2010 Institute for Medicine Future of Nursing Report
The convergence of the concerns about the challenges of the U.S. health care system (high cost, primary care shortages, an aging and sicker population, health care disparities, and fragmentation of care) stimulated a national reaction regarding the need to transform the U.S. health care system. In response, the Robert Wood Johnson Foundation’s Initiative on the Future of Nursing (INF) at the Institute of Medicine (IOM) was launched in 2009 (IOM, 2010).
As a part of this 2-year review process, the IOM brought together experts and thought leaders from multiple disciplines (nursing, business, law, medicine, and others) to develop a plan of action to transform the U.S. health care system. Since nurses compose the largest group of health care providers, the IOM believed that focusing on the challenges of the nursing profession would benefit the entire health care delivery system (IOM, 2010). The IOM and the Task Force held three national forums and numerous technical and policy-oriented workshops to gather insight into the challenges of nursing and to develop a transformational report on the future of nursing. On October 5, 2010, the IOM released a landmark report, The Future of Nursing (IOM, 2010).
The key messages of The Future of Nursing report (2010) include
▪ Nurses should practice to the full extent of their education and training through an improved education system that promotes seamless academic progression.
▪ Nurses should be full partners, with physicians and other health care professionals, in redesigning health care in the United States.
▪ Effective workforce planning and policy making require better data collection and an improved information infrastructure.
The recommendations that were derived from these key messages were as follows:
1. Remove scope-of-practice barriers.
3. Implement nurse residency programs.
4. Increase the proportion of nurses with baccalaureate degrees to 80% by 2020.
5. Double the number of nurses with doctorates by 2020.
6. Ensure that nurses engage in lifelong learning.
7. Prepare and enable nurses to lead change to advance health.
8. Build an infrastructure for the collection and analysis of interprofessional health care workforce data (IOM, 2010).
At the time of this writing, the website Campaign for Action Dashboard (http://campaignforaction.org/sites/default/files/2015-Dashboard-Final-5.27.15.pdf) provides the 2013 results of some of the initiatives. For example, in 2010, 49% of the RNs working held BSNs; in 2013, 51% hold this degree. A number of states have moved from a restricted scope of practice to full practice, which allows nurse practitioners (NPs) to evaluate patients, diagnose, order and interpret diagnostic tests, initiate and manage treatment, including prescribing drugs since 2010. In addition the number of DNP graduates has doubled between 2010 and 2013. There is much optimism that the Future of Nursing initiative has stimulated many stakeholders to reach for the goals established by the IOM Future of Nursing report.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree