CHAPTER 11 1. Have evidence of normal healing of surgical wound(s) 3. Have no evidence of wound or urinary tract infection 4. Have no signs and symptoms of postoperative complications 5. Demonstrate care of suprapubic catheter if present 6. Demonstrate the ability to measure residual urine 7. State signs and symptoms to report to the health care provider 8. Verbalize an understanding of and a plan for adhering to recommended follow-up care including future appointments with health care provider, medications prescribed, activity restrictions, and measures to prevent constipation Preoperative—Refer to Standardized Preoperative Care Plan. Postoperative—Use in conjunction with the Standardized Postoperative Care Plan. Definition: Incomplete emptying of the bladder • Obstruction of the urethral and/or suprapubic catheters if present • Impaired urination after removal of the catheter(s) associated with: • Edema of the bladder neck and urethra resulting from surgical trauma • Increased tone of the urinary sphincters resulting from sympathetic nervous system stimulation (can result from pain, fear, and anxiety) • Decreased perception of bladder fullness resulting from the depressant effect of anesthesia and some medications (e.g., narcotic [opioid] analgesics) • Relaxation of the bladder muscle resulting from the depressant effect of anesthesia and some medications (e.g., narcotic [opioid] analgesics) and stimulation of the sympathetic nervous system (can result from pain, fear, and anxiety) • Urethral obstruction resulting from excessive elevation of the bladder neck • Decreased gastrointestinal motility associated with manipulation of the bowel (if an abdominal approach was used), decreased activity, and the depressant effect of the anesthetic and narcotic (opioid) analgesics • Reluctance to defecate associated with fear of pain and possible disruption of sutures Definition: Surgery-related bladder injury Related to: Accidental tear or ligation during the surgical procedure Definition: At risk for invasion of the body by pathogenic organisms • Increased growth and colonization of microorganisms associated with urinary stasis • Introduction of pathogens associated with the presence of urethral and/or suprapubic catheters and performance of intermittent catheterizations if being done • Wound contamination associated with introduction of pathogens during or after surgery (particularly high risk with a vaginal approach because of the proximity of the incision to the perianal area) • Decreased resistance to infection associated with factors such as diminished blood flow to wound area or an inadequate nutritional status Cystectomy is the removal of the bladder and is accompanied by a procedure to divert urinary flow. It may be performed to treat a malignancy of the bladder, congenital bladder anomalies, neurogenic bladder, and irreparable bladder trauma. A cystectomy may also be performed to prevent further deterioration of renal function associated with chronic bladder infection. In some cases, the surgery includes removal of just the bladder (simple cystectomy), but when there is an invasive malignancy, a more radical procedure is performed. In men, a radical cystectomy usually includes removal of the bladder, prostate, seminal vesicles, a portion of the vas deferens, and some or all of the pelvic lymph nodes. In women, a radical cystectomy usually includes removal of the bladder, urethra, uterus, fallopian tubes, ovaries, a portion of the anterior vaginal wall, and some or all of the pelvic lymph nodes. 1. Maintain an adequate urine output via the urinary diversion 2. Have surgical pain controlled 3. Have evidence of normal healing of surgical wound 4. Have a medium pink to red, moist stoma and intact peristomal skin 5. Have no signs and symptoms of postoperative complications 6. Verbalize a basic understanding of the anatomical changes that have occurred as a result of the surgery 7. Demonstrate the ability to change the urostomy appliance and maintain stomal and peristomal skin integrity 8. Demonstrate the ability to properly clean reusable urostomy equipment 9. Demonstrate the ability to drain and irrigate a continent internal reservoir if present 10. Identify ways to control odor of the urostomy drainage and appliance 11. Identify ways to prevent urinary tract infection 12. State signs and symptoms to report to the health care provider 13. Share thoughts and feelings about altered urinary elimination and its effect on body image and lifestyle 14. Identify appropriate community resources that can assist with home management and adjustment to changes resulting from the urinary diversion 15. Verbalize an understanding of and a plan for adhering to recommended follow-up care including future appointments with health care provider, wound care, activity level, and medications prescribed For a full, detailed care plan on this topic, go to http://evolve.elsevier.com/Haugen/careplanning/. The surgical approach used to perform a nephrectomy depends on the extensiveness of the planned surgery; the client’s age, body build, and physiological status; the underlying pathology; and prior surgical incisions. The approach commonly used for a simple nephrectomy (removal of just the kidney) is the subcostal flank approach. Other approaches (e.g., thoracoabdominal, transabdominal, dorsolumbar) may be necessary when greater visualization, improved access, or a radical nephrectomy (removal of the kidney, renal artery and vein, adrenal gland, proximal ureter, regional lymph nodes, and surrounding fat and fascia) is necessary. Although it is most often necessary to remove the entire kidney, advances in renal imaging, earlier diagnosis of renal disease, and improved surgical techniques have provided surgeons with an option of performing a partial nephrectomy (nephron-sparing nephrectomy) in some instances. In these situations, a laparoscopic rather than an open approach is often feasible. 1. Have evidence of normal healing of the surgical wound 2. Have adequate functioning of the remaining kidney 3. Have clear, audible breath sounds throughout lungs 4. Have no signs and symptoms of postoperative complications 5. Verbalize ways to maintain health of the remaining kidney 6. State signs and symptoms to report to the health care provider 7. Share thoughts and feelings about the loss of the kidney 8. Verbalize an understanding of and a plan for adhering to recommended follow-up care including future appointments with health care provider, medications prescribed, activity level, wound care, and plans for subsequent treatment of the underlying disorder. See Standardized Preoperative and Postoperative Care Plans for additional diagnoses. Definition: Inspiration and/or expiration that does not provide adequate ventilation • Increased rate of respirations associated with fear and anxiety • Decreased rate of respirations associated with the depressant effect of anesthesia and some medications (e.g., narcotic [opioid] analgesics, some antiemetics) • Decreased depth of respirations associated with: • Depressant effect of anesthesia and some medications (e.g., narcotic [opioid] analgesics, some antiemetics) • Reluctance to breathe deeply resulting from incisional pain and fear of dislodging chest tube if present (a chest tube is usually inserted after a thoracoabdominal approach and may be needed after a flank approach) • Positioning, weakness, fatigue, and elevation of the diaphragm (can occur if abdominal distention is present)
The Client with Alterations in the Kidney and Urinary Tract
BLADDER NECK SUSPENSION (VESICOURETHRAL SUSPENSION)
OUTCOME/DISCHARGE CRITERIA
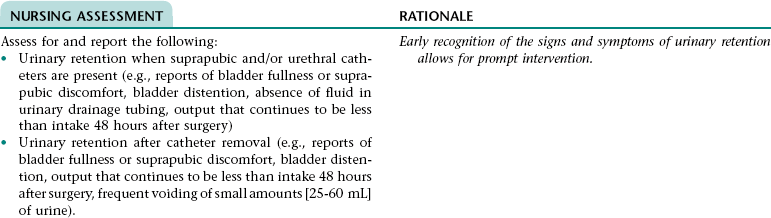
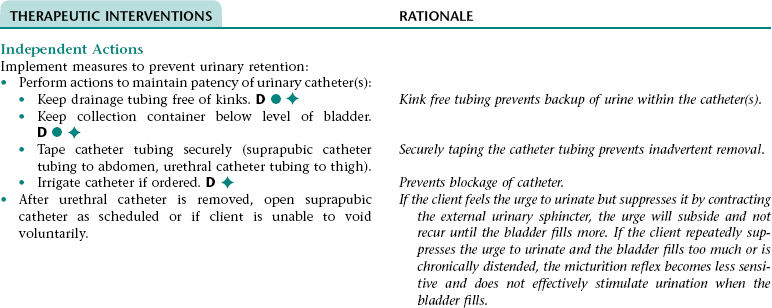
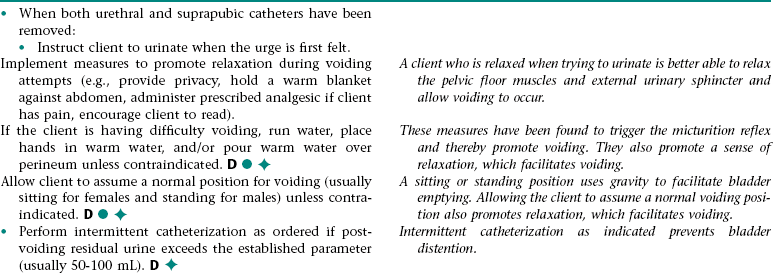
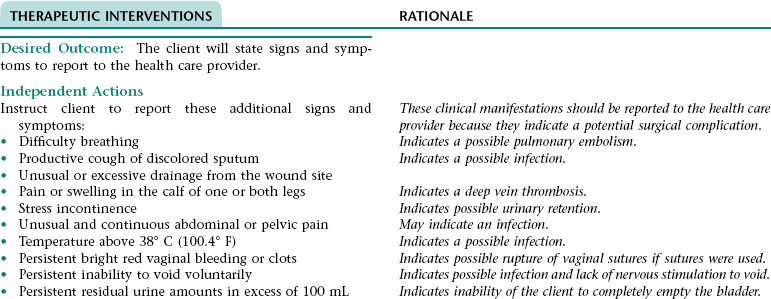
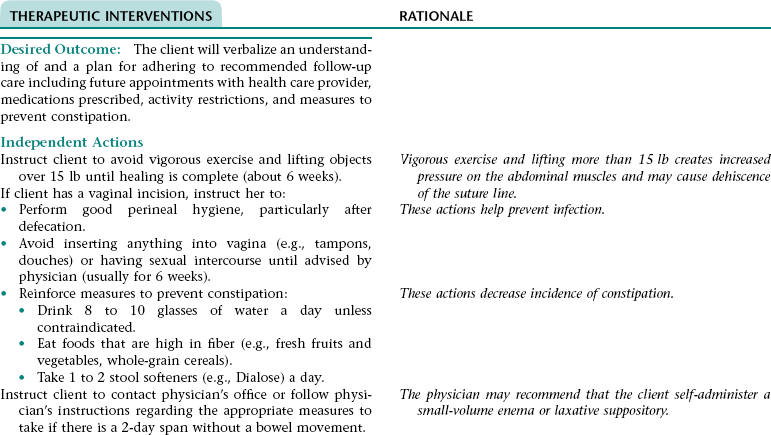
Nursing Diagnosis URINARY RETENTION NDx
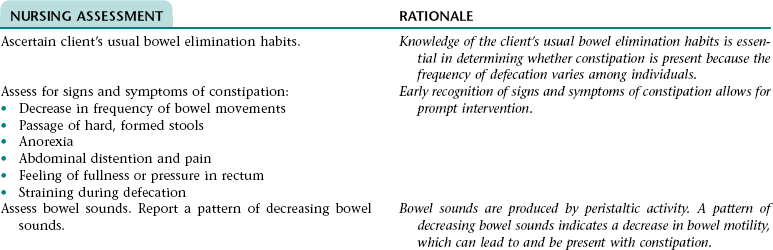
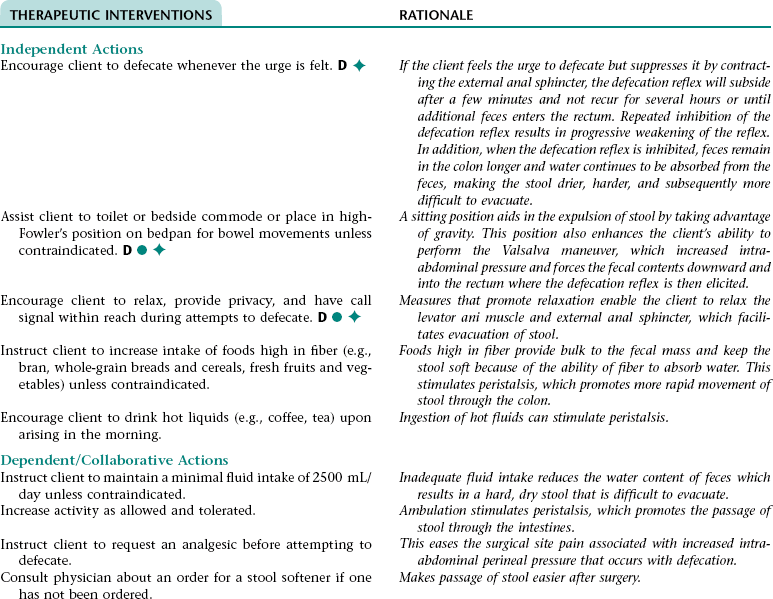
Nursing Diagnosis RISK FOR CONSTIPATION NDx
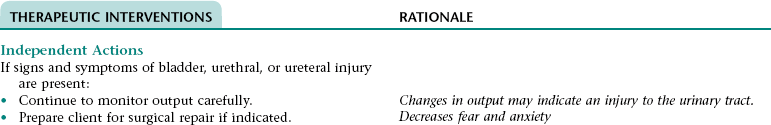
Collaborative Diagnosis RISK FOR BLADDER, URETHRAL, OR URETERAL INJURY
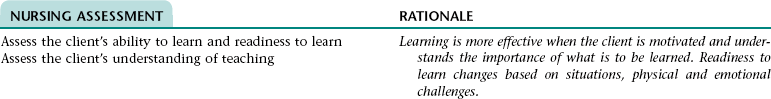
NURSING ASSESSMENT
RATIONALE
Assess for and report signs and symptoms of bladder, urethral, or ureteral injury (e.g., persistent or increasing hematuria or backache, urine output less than 200 mL in first 6-8 hours after surgery).
Early recognition of signs and symptoms of urinary tract injury allows for prompt intervention.
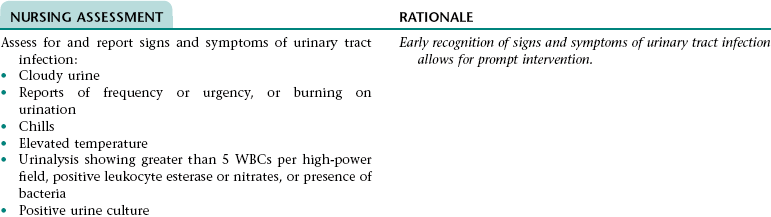
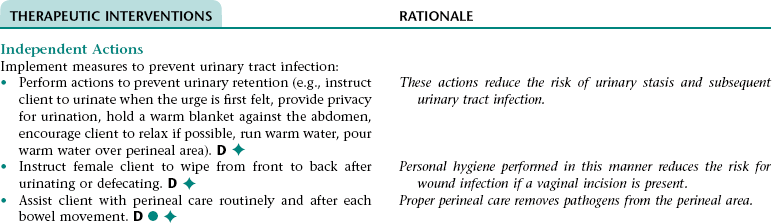
Collaborative Diagnosis RISK FOR URINARY TRACT INFECTION; WOUND INFECTION
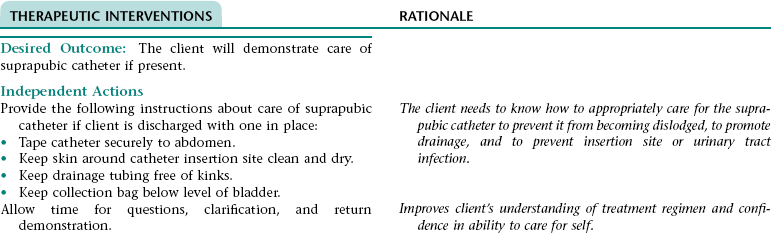
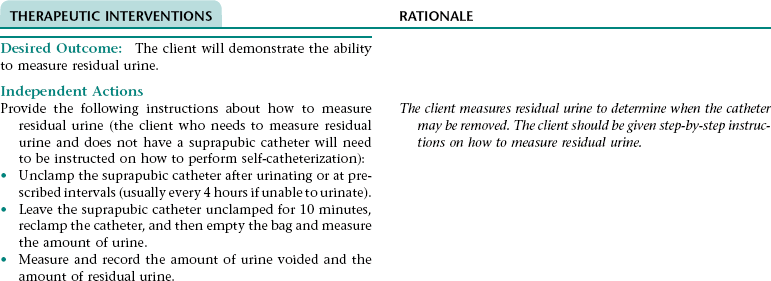
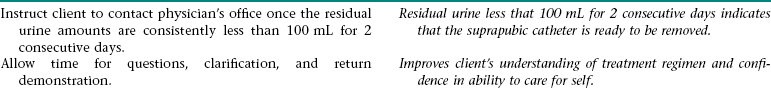
Nursing Diagnosis DEFICIENT KNOWLEDGE NDx; INEFFECTIVE FAMILY THERAPEUTIC REGIMEN MAINTENANCE NDx; or INEFFECTIVE SELF-HEALTH MANAGEMENT* NDx
 CYSTECTOMY WITH URINARY DIVERSION
CYSTECTOMY WITH URINARY DIVERSION
OUTCOME/DISCHARGE CRITERIA
NEPHRECTOMY
OUTCOME/DISCHARGE CRITERIA
Nursing Diagnosis INEFFECTIVE BREATHING PATTERN NDx
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


The Client with Alterations in the Kidney and Urinary Tract
Get Clinical Tree app for offline access