CHAPTER 9 Abdominal trauma involves injury to the body structures located between the diaphragm and the pelvis. Injury to abdominal contents occurs from a direct impact or movement of organs within the body as a result of rapid deceleration, causing rupture, lacerations, and/or tears in organs or blood vessels. Organs injured with abdominal trauma include the spleen, liver, stomach, large and small intestines, pancreas, kidneys, and urinary bladder. The large vessels in the abdomen, the aorta and vena cava, may also be injured. 1. Have evidence of normal healing of trauma and/or surgical wound 2. Have clear, audible breath sounds 4. Have surgical pain controlled 5. Have no signs and symptoms of complications 6. State signs and symptoms to report to the health care provider 7. Verbalize an understanding of and a plan for adhering to recommended follow-up care including future appointments with health care provider, medications prescribed, activity level, and wound care. Definition: Inspiration and/or expiration that does not provide adequate ventilation • Increased rate of respirations associated with: • Decreased rate of respirations associated with injury and/or the depressant effect of anesthesia and some medications (e.g., narcotic [opioid] analgesics, some antiemetics) • Decreased depth of respirations associated with: • Deficient fluid volume NDx related to excessive blood loss, loss of fluid associated with vomiting and nasogastric tube drainage (if present) • Hypokalemia and metabolic alkalosis related to loss of electrolytes and hydrochloric acid associated with blood loss, vomiting, and nasogastric tube drainage DESIRED OUTCOMES: The client will maintain fluid and electrolyte balance as evidenced by: a. Blood pressure (B/P) and pulse within normal range for client and stable with position change b. Capillary refill time less than 2 to 3 seconds e. Urine specific gravity within normal range f. Soft, nondistended abdomen with active bowel sounds g. Absence of cardiac dysrhythmias, muscle weakness, paresthesias, twitching, spasms, and dizziness h. BUN, Hct, serum electrolyte, and ABG values within normal range Definition: Decrease in blood circulation to the periphery that may compromise health DESIRED OUTCOMES: The client will maintain adequate tissue perfusion as evidenced by: NOC OUTCOMES: Circulation status; tissue perfusion: abdominal organs; tissue perfusion: cardiac; tissue perfusion: cerebral; tissue perfusion: peripheral; tissue perfusion: pulmonary Definition: Inflammation of the peritoneum • Release of intestinal contents into the peritoneal cavity resulting from abdominal trauma • Exposure of abdominal contents to pathogens associated with a penetrating abdominal wound • Systemic hypoperfusion associated with maldistribution of circulating blood, deficient fluid volume, and decreased myocardial contractility resulting from uncontrolled systemic inflammatory response to severe infection • Hypoperfusion of major organs associated with septic shock • Microvascular thrombosis associated with disseminated intravascular coagulation (DIC) if it occurs DESIRED OUTCOMES: The client will not develop organ ischemia or dysfunction as evidenced by: b. Urine output at least 30 mL/h c. Unlabored respirations at 12 to 20 breaths/min d. Audible breath sounds without an increase in adventitious sounds e. Absence of new or increased abdominal pain, distention, and diarrhea f. BUN, creatinine, aspartate aminotransferase (AST), alanine aminotransferase (ALT), and lactate dehydrogenase (LDH) levels within normal range 1. Have evidence of normal healing of surgical wound 2. Have clear, audible breath sounds 4. Have surgical pain controlled 5. Have no signs and symptoms of postoperative complications 6. State signs and symptoms to report to the health care provider 7. Verbalize an understanding of and a plan for adhering to recommended follow-up care including future appointments with health care provider, medications prescribed, activity level, and wound care. For a full, detailed care plan on this topic, go to http://evolve.elsevier.com/Haugen/careplanning/. 1. Have surgical pain controlled 2. Have evidence of normal healing of the surgical wound 3. Have a medium pink to red, moist stoma and intact peristomal and perianal skin 4. Have no evidence of fluid and electrolyte imbalances 5. Maintain an adequate nutritional status 6. Have no signs and symptoms of postoperative complications 7. Verbalize a basic understanding of the anatomical changes that have occurred as a result of the bowel diversion 8. Identify ways to maintain fluid and electrolyte balance 9. Verbalize ways to maintain an optimal nutritional status 10. Identify methods of controlling odor and sound associated with ileostomy drainage and gas 11. Demonstrate the ability to change the pouch system, maintain integrity of the peristomal and perianal skin, and maintain adequate stomal integrity 12. Demonstrate the ability to properly use, clean, and store ostomy products 13. Demonstrate the ability to drain and irrigate a continent ileostomy if present 14. Identify ways to prevent and treat blockage of the stoma 15. State signs and symptoms to report to the health care provider 16. Share thoughts and feelings about the effect of altered bowel function on self-concept and lifestyle 17. Identify appropriate community resources that can assist with home management and adjustment to changes resulting from the bowel diversion 18. Verbalize an understanding of and a plan for adhering to recommended follow-up care including future appointments with health care provider, wound care, activity level, and medications prescribed. Definition: Absence or deficiency of cognitive information related to a specific topic Deficient fluid volume NDx related to: • Restricted oral fluid intake before, during, and after surgery • Loss of fluid associated with vomiting, nasogastric tube drainage, and/or high-volume ileostomy output • Loss of hydrochloric acid associated with vomiting and nasogastric tube drainage • Loss of bicarbonate ions associated with high-volume ileostomy output (effluent contains bicarbonate ions that would normally be absorbed throughout the large intestine) DESIRED OUTCOMES: The client will not experience deficient fluid volume, hypokalemia, hypochloremia, hypomagnesemia, and acid-base imbalance as evidenced by: d. B/P and pulse rate within normal range for client and stable with position change e. Capillary refill time less than 2 to 3 seconds g. Balanced intake and output within 48 hours after surgery h. Urine specific gravity within normal range i. Return of peristalsis within expected time k. Absence of cardiac dysrhythmias, twitching, muscle weakness, paresthesias, dizziness, headache, nausea, and vomiting l. Negative Chvostek’s and Trousseau’s sign m. BUN, serum electrolyte, and arterial blood gas values within normal range Definition: Damage to mucous membrane, corneal, integumentary, or subcutaneous tissues • Disruption of tissue associated with the surgical procedure • Delayed wound healing associated with factors such as decreased nutritional status and inadequate blood supply to wound area • Irritation of skin associated with: • Contact with wound drainage, ileostomy output (effluent is rich in proteolytic enzymes), soap residue and perspiration under the pouch, and/or mucus drainage from the anus (occurs if rectum was left intact) • Frequent or improper removal of tape, adhesives, or other substances used to secure pouch to the skin • Aggressive cleansing of peristomal area • Sensitivity to tape, pouch material, ostomy paste, and/or substances used to secure pouch to the skin (e.g., adhesive disk, skin barrier, adhesive spray) • Pressure from tubes, appliance belt, and/or pouch drainage valve or clamp
The Client with Alterations in the Gastrointestinal Tract
ABDOMINAL TRAUMA
OUTCOME/DISCHARGE CRITERIA
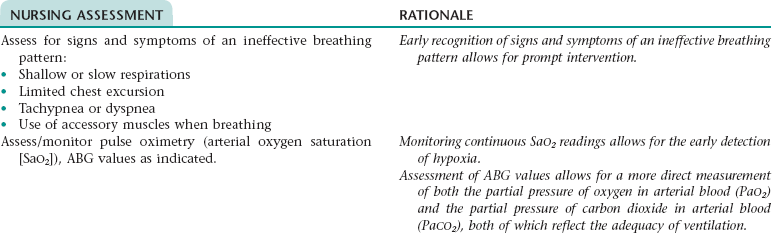
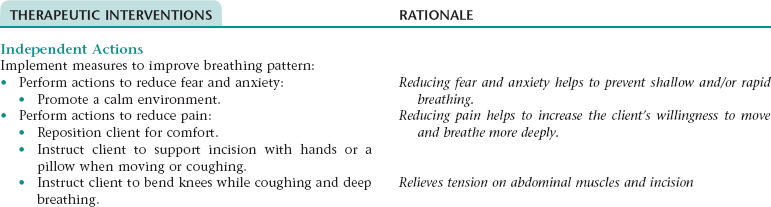
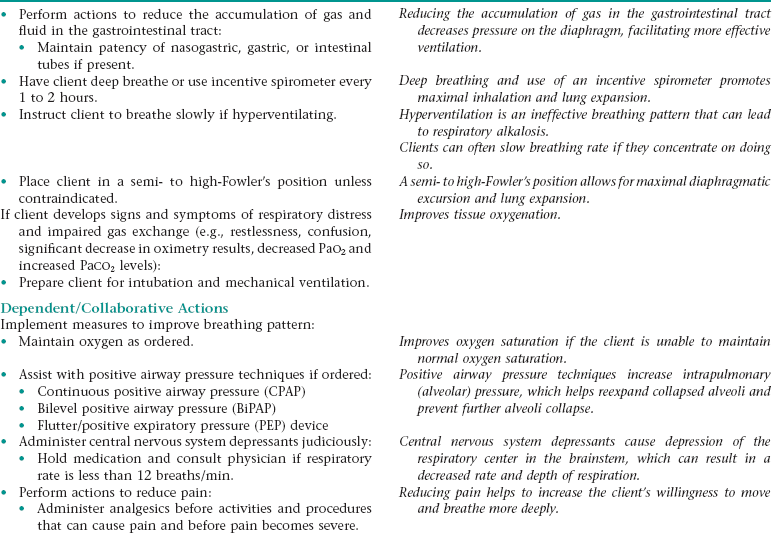
Nursing Diagnosis INEFFECTIVE BREATHING PATTERN NDx
Subjective
Objective
Complaints of shortness of breath
Dyspnea; orthopnea; increased respiratory rate; decreased depth of breathing; decreased minute ventilation; decreased vital capacity; nasal flaring; use of accessory muscles to breathe; altered chest excursion; pursed-lip breathing; decreased oxygen saturation; arterial blood gas (ABG) values: respiratory acidosis
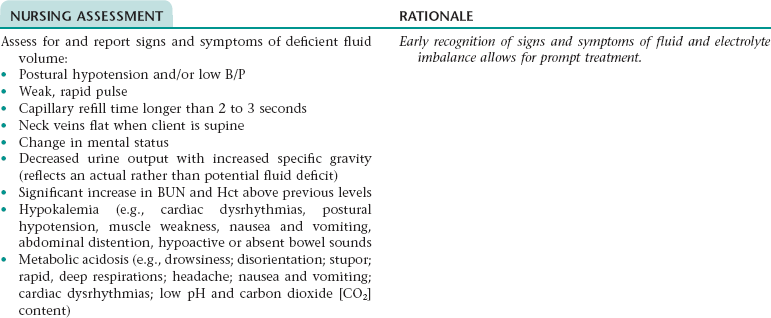
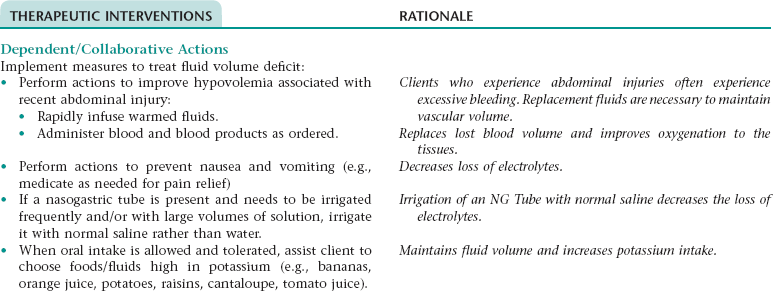
Nursing Diagnosis RISK FOR IMBALANCED FLUID VOLUME NDx; RISK FOR ELECTROLYTE IMBALANCE* NDx
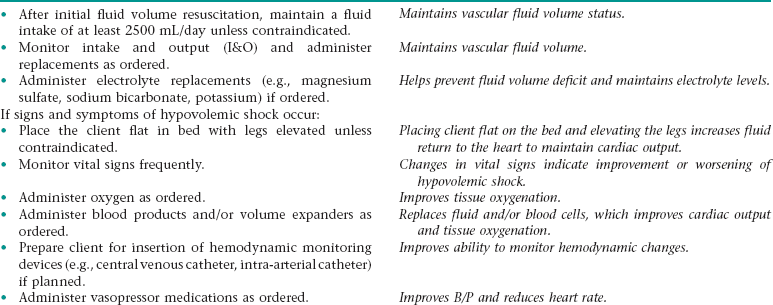
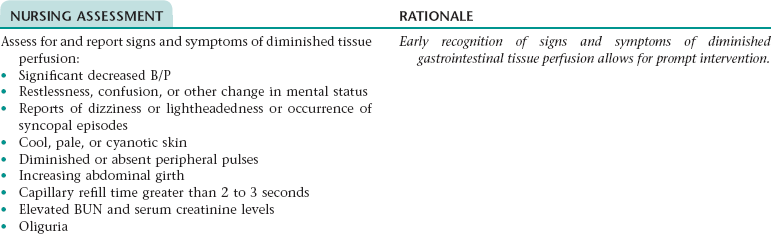
Nursing Diagnosis INEFFECTIVE PERIPHERAL TISSUE PERFUSION NDx
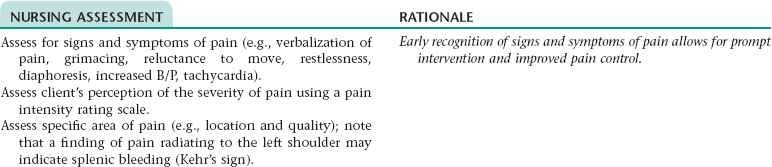
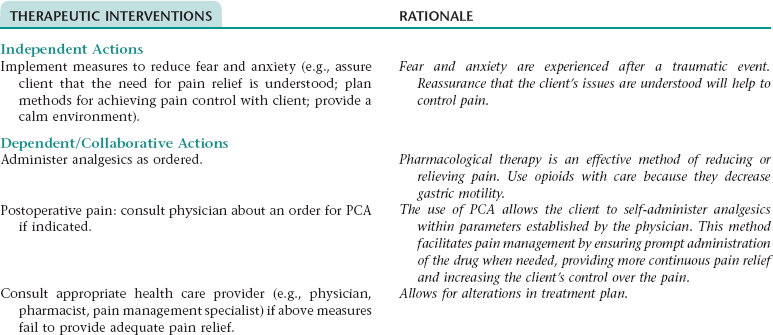
Nursing Diagnosis ACUTE PAIN NDx
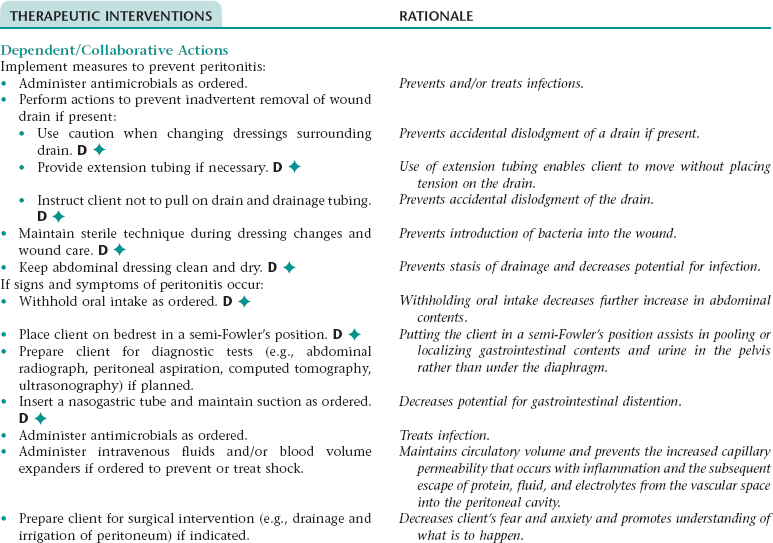
Collaborative Diagnosis RISK FOR PERITONITIS
NURSING ASSESSMENT
RATIONALE
Assess for and report signs and symptoms of peritonitis (e.g., further increase in temperature or temperature above 38° C; distended, rigid abdomen; increase in severity of abdominal pain; rebound tenderness; increased nausea and vomiting; diminished or absent bowel sounds; tachycardia; tachypnea; hypotension; a WBC count greater than 15,000/mm3).
Early recognition of signs and symptoms of peritonitis allows for prompt intervention.
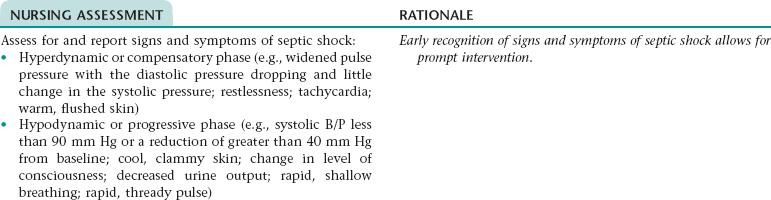
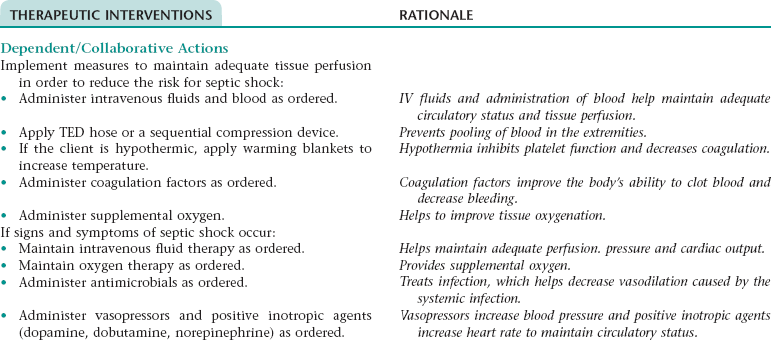
Collaborative Diagnosis RISK FOR SEPTIC SHOCK
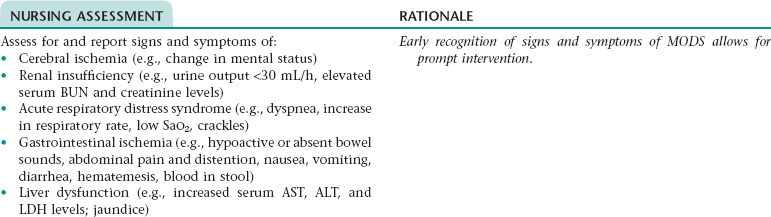
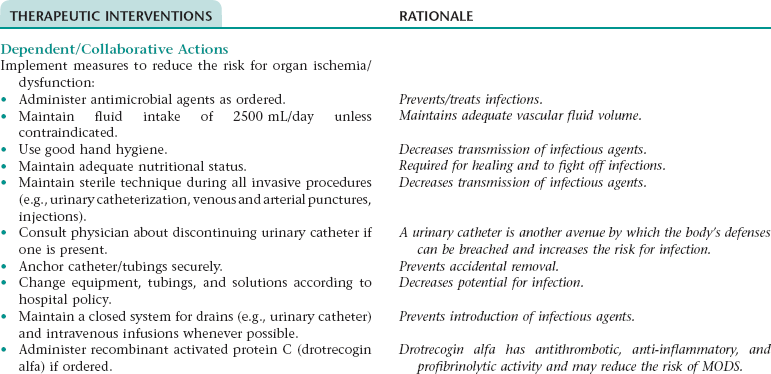
Collaborative Diagnosis RISK FOR ORGAN ISCHEMIA/DYSFUNCTION (MULTIPLE ORGAN DYSFUNCTION SYNDROME [MODS])
Subjective
Objective
N/A
Severe hypotension; tachycardia; urine output less than 30 mL/h; dyspnea, tachypnea; altered arterial blood gas values with low PaO2; elevated BUN and serum creatinine levels; crackles throughout lungs; changes in mental status
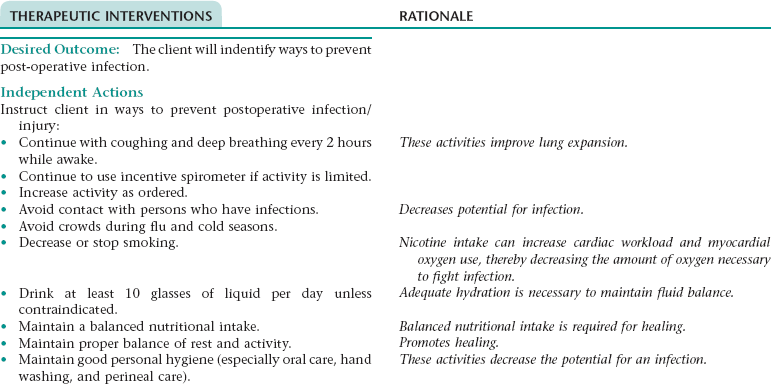
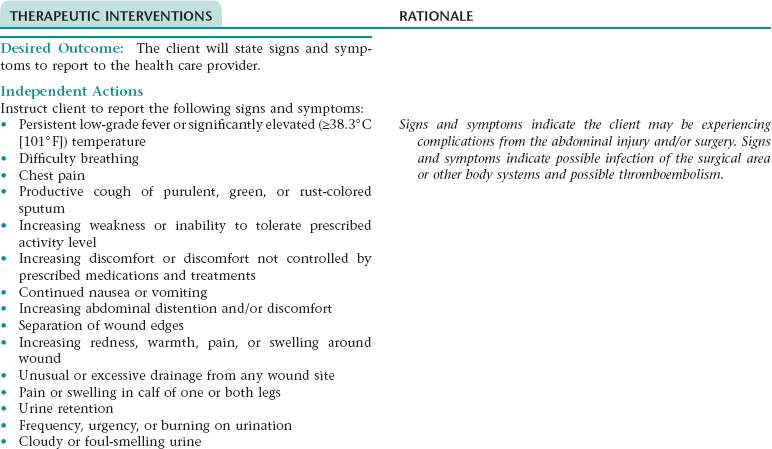
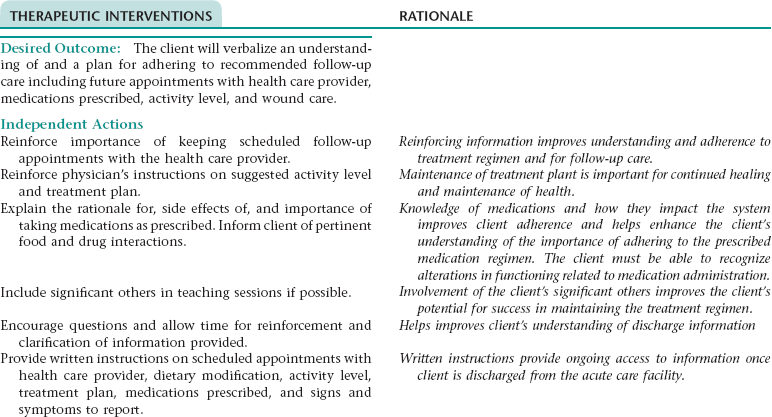
Nursing Diagnosis DEFICIENT KNOWLEDGE NDx; INEFFECTIVE FAMILY THERAPEUTIC REGIMEN MANAGEMENT NDx; OR INEFFECTIVE HEALTH MANAGEMENT* NDx
NURSING ASSESSMENT
RATIONALE
Assess client’s willingness to learn and knowledge related to the disease process.
The client’s willingness to learn and knowledge base provides the basis for education.
Assess for indications that the client may be unable to effectively manage the therapeutic regimen.
Early recognition of inability to understand disease process or self-care allows for change in the teaching plan.
OUTCOME/DISCHARGE CRITERIA
BOWEL DIVERSION: ILEOSTOMY
 An ileostomy is the diversion of the ileum from the abdominal cavity through an opening created in the abdominal wall. It may be performed after abdominal trauma or to treat conditions such as familial polyposis, intestinal cancer, and most commonly, inflammatory bowel disease that is refractory to conservative management. An ileostomy can be temporary or permanent.
An ileostomy is the diversion of the ileum from the abdominal cavity through an opening created in the abdominal wall. It may be performed after abdominal trauma or to treat conditions such as familial polyposis, intestinal cancer, and most commonly, inflammatory bowel disease that is refractory to conservative management. An ileostomy can be temporary or permanent.
OUTCOME/DISCHARGE CRITERIA
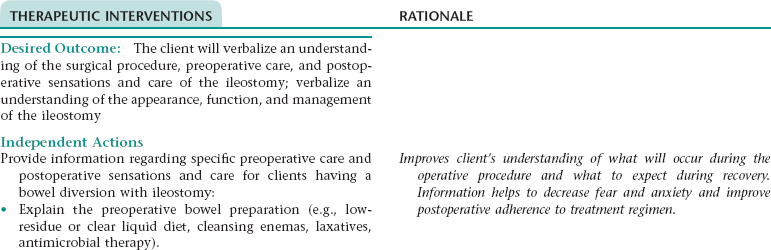
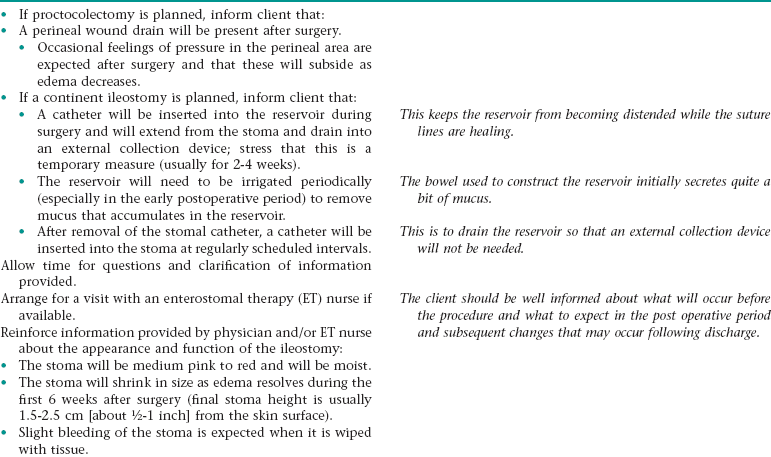
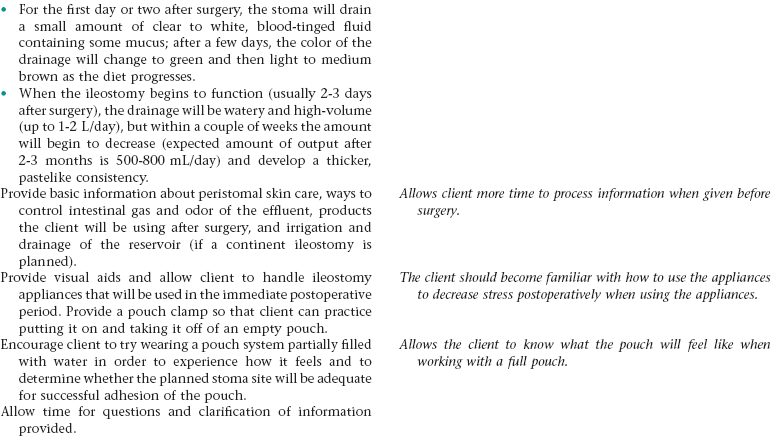
Nursing Diagnosis DEFICIENT KNOWLEDGE NDx
NURSING ASSESSMENT
RATIONALE
Assess client’s understanding of surgical procedure and outcome.
Client’s understanding of what may occur will decrease anxiety.
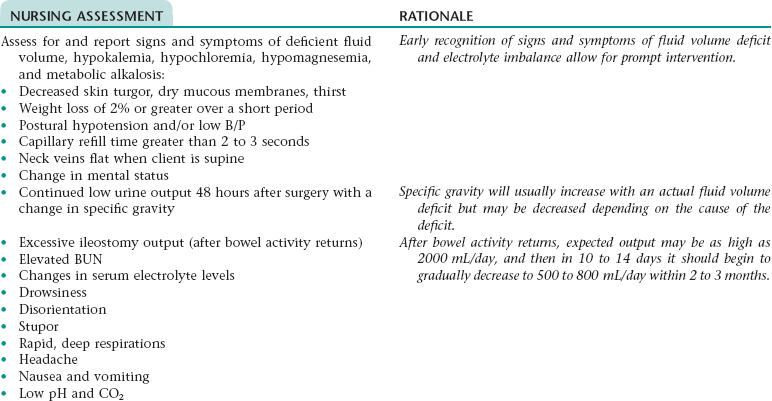
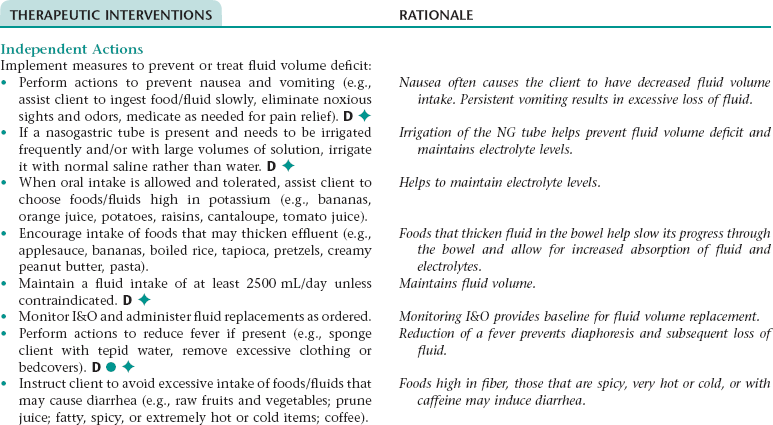
Nursing Diagnosis RISK FOR IMBALANCED FLUID VOLUME NDx; RISK FOR ELECTROLYTE IMBALANCE* NDx
Nursing Diagnosis ACTUAL/RISK FOR IMPAIRED TISSUE INTEGRITY NDx
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Nurse Key
Fastest Nurse Insight Engine
Get Clinical Tree app for offline access