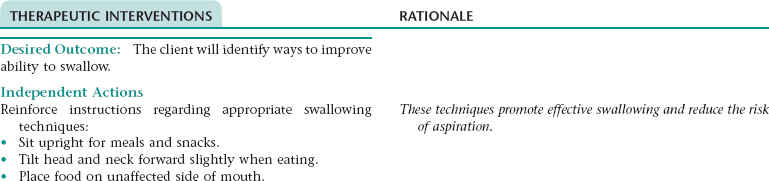
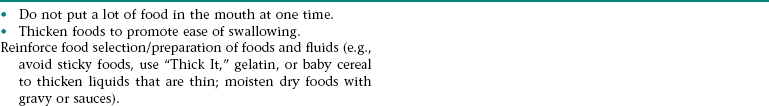
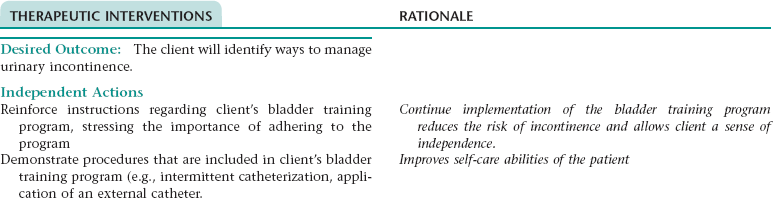
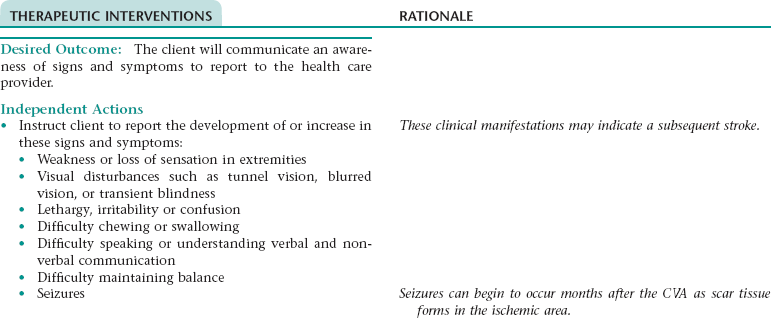
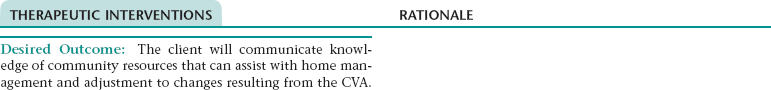
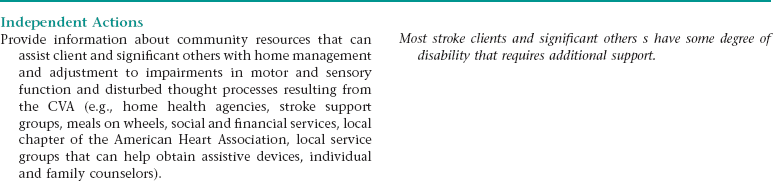
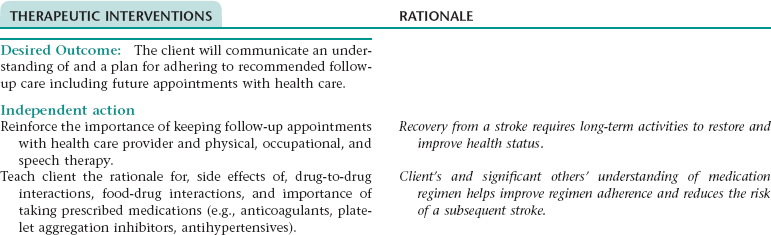
CHAPTER 6 There is no cure for Alzheimer’s disease. Treatment focuses on retaining memory, cognitive and physical functioning, and slowing the progression of the disease. Drug therapy consists of four medications that have been approved by the United States Food and Drug Administration: donepezil, rivastigmine, galantamine, and memantine. These medications regulate the neurotransmitters that transmit information from neuron to neuron. They are thought to help maintain cognitive and memory functioning and may control some of the behavioral symptoms. Other medications may be used to control the symptoms of insomnia, agitation, depression, and anxiety. 1. Maintain cognitive functioning as long as possible 2. Have a decline in number of wandering incidents 3. Have minimal episodes of aggressive behavior 4. Avoid behaviors that may harm self or others 5. Participate in activities of daily living 6. Engage in appropriate social interaction with others Related to: Cognitive changes in the client Related to: Degeneration of the CNS and cognitive functioning Definition: Inability to maintain a safe and growth-promoting immediate environment NOC OUTCOMES: Family functioning; safety behavior; home physical environment; self-care: instrumental activities of daily living Definition: Difficulty in performing family caregiver role 1. Have improved cerebral tissue perfusion 2. Have improved or stable neurological function 3. Experience optimal control of urinary elimination 4. Have no signs or symptoms of complications 5. Communicate an awareness of ways to decrease the risk of a recurrent CVA 6. Identify ways to manage sensory and speech impairments and disturbed thought processes 7. Identify ways to improve ability to swallow 8. Identify ways to manage urinary incontinence 9. Demonstrate measures to facilitate the performance of activities of daily living and increase physical mobility 10. Communicate an awareness of signs and symptoms to report to the health care provider and share thoughts and feelings about the effects of the CVA on lifestyle, roles, and self-concept 11. Communicate knowledge of community resources that can assist with home management and adjustment to changes resulting from the CVA 12. Communicate an understanding of and a plan for adhering to recommended follow-up care including future appointments with health care provider and therapists and medications prescribed. Definition: Inability to clear secretions from the respiratory tract to maintain patent airway • Stasis of secretions associated with decreased activity • Poor cough effort due to fatigue, changes in neuromuscular functioning Related to: Changes in neuromuscular functioning Related to: Ischemia within the sensory transmission pathways of the brain DESIRED OUTCOMES: The client will experience a reduction in and/or demonstrate beginning adaptation to disturbed sensory perception as evidenced by: Related to:Ischemia primarily of the parietal lobe of the nondominant cerebral hemisphere DESIRED OUTCOMES: The client will experience a reduction in and/or demonstrate beginning adaptation to unilateral neglect as evidenced by: DESIRED OUTCOME: The client will perform self-care activities within cognitive and physical limitations. Related to:Damage to cerebral tissue NOC OUTCOMES: Information processing; neurological status: consciousness; cognitive ability; disoriented thought self-control; memory; mood equilibrium Related to decreased oral intake associated with difficulty chewing, swallowing, and feeding self • Decreased gastrointestinal motility associated with decreased activity • Decreased intake of fluids and foods high in fiber associated with difficulty chewing, swallowing, and feeding self • Failure to respond to the urge to defecate associated with decreased level of consciousness or inability to recognize sensation of rectal fullness • Increased intracranial pressure (ICP) • Accumulation of blood in the cerebral tissue (can occur if CVA resulted from conditions such as ruptured cerebral aneurysm) • Cerebral edema associated with increased capillary permeability of cerebral vessels and disruption of the sodium pump within the cells (both occur as a result of cerebral hypoxia) • Increase in cerebral vascular volume associated with vasodilation of the cerebral vessels • Corneal irritation and abrasion related to inability to close eye on affected side if facial nerve paresis or paralysis has occurred • Subluxation of shoulder related to muscle weakness in affected upper arm and shoulder and gravity pull on affected arm • Activity limitations associated with decreased motor function and spatial-perceptual impairments • Loss of muscle tone during period of flaccidity of affected extremities (flaccid paralysis is usually present during the first few days after a CVA) • Hypertonia of affected extremities (as muscle tone returns after period of flaccidity, it often progresses to spasticity within about 6-8 weeks) • Reluctance to move associated with fear of injuring self (occurs mainly with ischemia of the dominant hemisphere) • Loss of muscle mass, tone, and strength associated with prolonged disuse • Increased reflex activity of the bladder and loss of voluntary control of urinary elimination associated with upper motor neuron involvement if it has occurred • Decreased ability to control urination associated with decreased level of consciousness or inability to recognize sensation of bladder fullness • Inability to get to bedside commode or bathroom in a timely manner associated with: • Delay in obtaining assistance resulting from inability to communicate the urge to urinate • Change in appearance (e.g., hemiplegia, facial droop, ptosis) • Lifestyle and role changes associated with motor and spatial-perceptual impairments and disturbed thought processes • Impaired verbal communication • Loss of self-control (e.g., automatic speech, emotional lability, inappropriate behavior) or exaggerated emotional responses Craniocerebral trauma is classified according to location (e.g., skull, epidural area, brainstem), effect (e.g., concussion, DAI, depressed fracture of the skull, contusion, subdural hematoma), and/or severity. The severity of trauma ranges from minor (usually a concussion with no alteration in consciousness or a loss of consciousness lasting 5 minutes or less) to severe, in which extensive contusion and/or laceration of brain tissue and possible brainstem injury occurs. Severe craniocerebral trauma usually involves a period of prolonged unconsciousness and results in permanent neurological impairments that require extensive rehabilitation and long-term care. 1. Have improved cerebral tissue perfusion 2. Have improved or stable neurological function 3. Have an adequate nutritional status 4. Have no signs or symptoms of complications 5. Identify ways to adapt to neurological deficits that may persist after craniocerebral trauma and/or surgery 6. Identify ways to reduce headache 7. State signs and symptoms to report to the health care provider 8. Share thoughts and feelings about residual neurological impairments 9. Identify community resources that can assist with home management and adjustment to changes resulting from craniocerebral trauma and/or craniotomy 10. Verbalize an understanding of and a plan for adhering to recommended follow-up care including future appointments with health care provider and therapists and medications prescribed 11. Use in conjunction with Preoperative and Postoperative Care Plan if the patient underwent surgery.
The Client with Alterations in Neurological Function
ALZHEIMER’S DISEASE/DEMENTIA
 Alzheimer’s disease is a slowly progressive disease that is characterized by stages of declining memory, cognitive and behavioral functioning. Approximately 5 million Americans have been diagnosed with Alzheimer’s disease, with a predicted increase to 7.7 million by 2031 It is the most common form of dementia and affects more women than men (possibly because women live longer), and the risk for and incidence of this disease is slightly higher in African Americans and Hispanics than in other populations.
Alzheimer’s disease is a slowly progressive disease that is characterized by stages of declining memory, cognitive and behavioral functioning. Approximately 5 million Americans have been diagnosed with Alzheimer’s disease, with a predicted increase to 7.7 million by 2031 It is the most common form of dementia and affects more women than men (possibly because women live longer), and the risk for and incidence of this disease is slightly higher in African Americans and Hispanics than in other populations.
OUTCOME/DISCHARGE CRITERIA
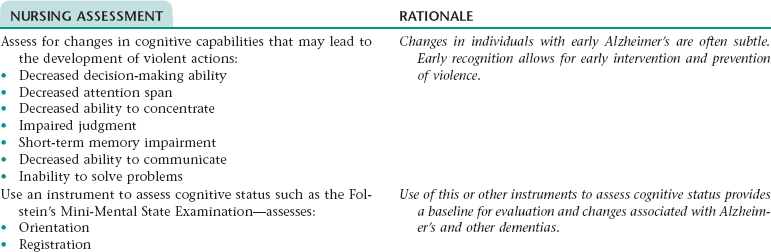
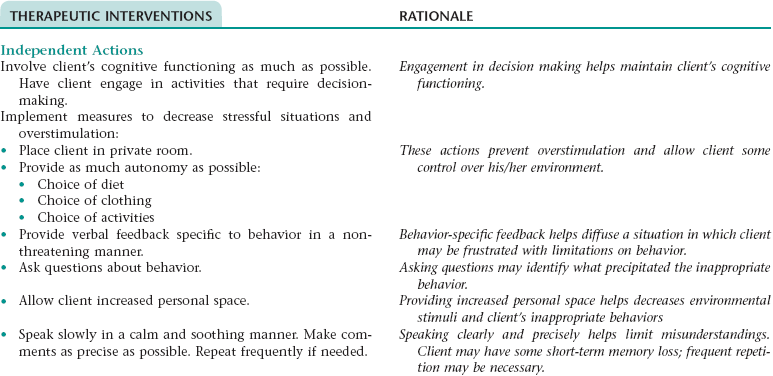
Nursing Diagnosis RISK FOR VIOLENCE: SELF-DIRECTED OR OTHER-DIRECTED NDx
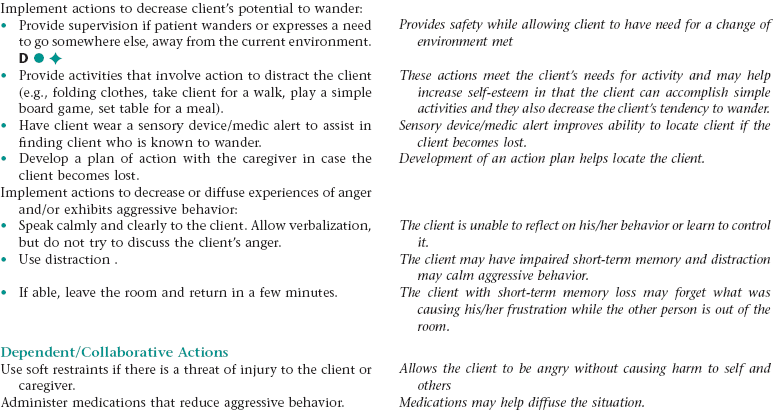
Nursing Diagnosis SELF-CARE DEFICIT: DRESSING, BATHING, FEEDING, AND TOILETING NDx
NURSING ASSESSMENT
RATIONALE
Assess client’s current self-care habits.
Provides a baseline of client’s ability and where interventions should be implemented
Assess client’s cognitive and physical ability to perform selfcare habits.
When a client’s cognitive abilities are impaired, the client is unable to determine self-care needs.
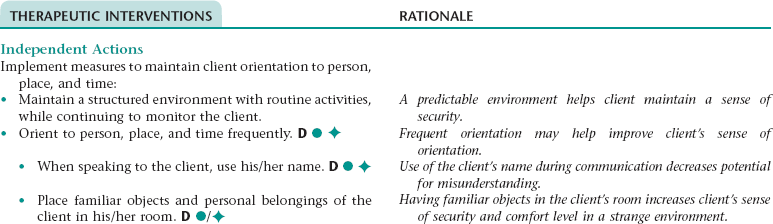
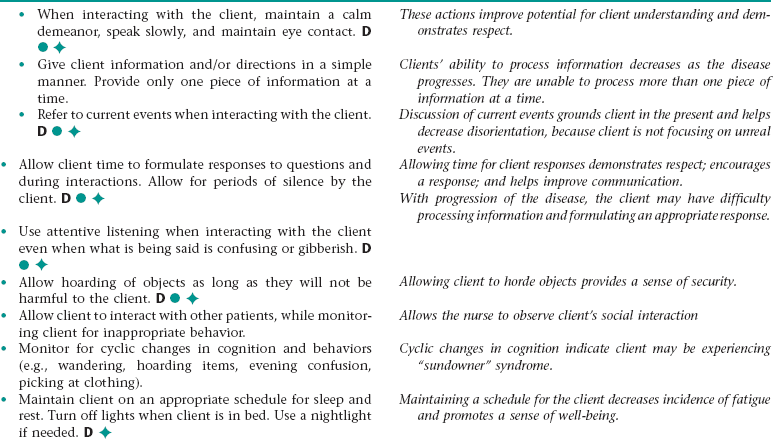
Nursing Diagnosis CHRONIC CONFUSION NDx
NURSING ASSESSMENT
RATIONALE
Assess for episodes of disorientation to person, place, and time, episodes of inappropriate behavior, impaired decision-making ability, impaired memory and judgment, delusions, impaired attention span.
Early recognition of signs and symptoms of confusion allows for prompt intervention.
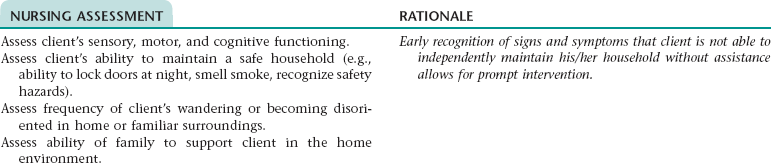
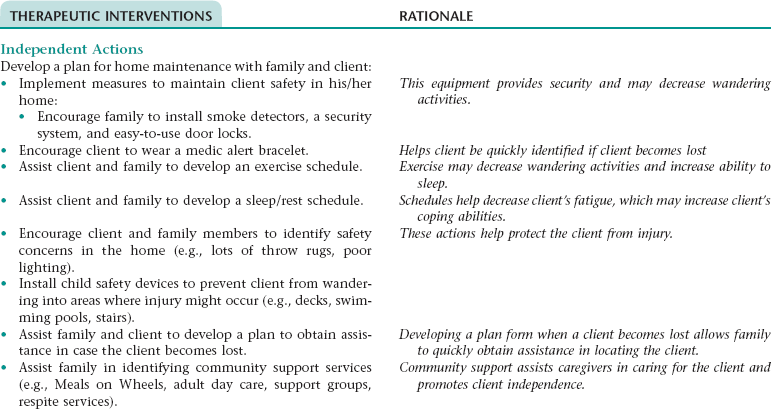
Nursing Diagnosis IMPAIRED HOME MAINTENANCE NDx
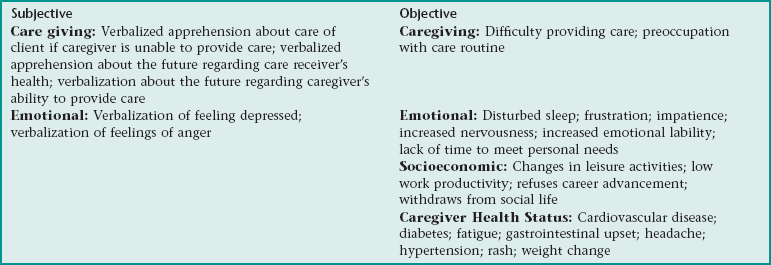
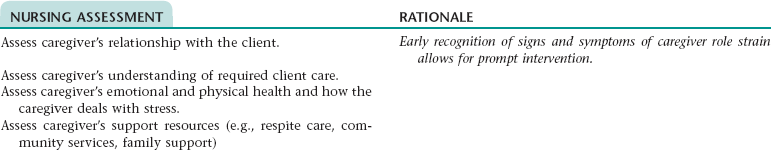
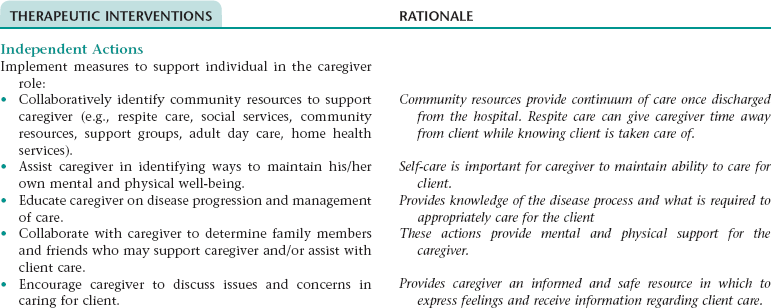
Nursing Diagnosis RISK FOR CAREGIVER ROLE STRAIN NDx
CEREBROVASCULAR ACCIDENT
 A cerebrovascular accident (CVA, stroke, brain attack) is the result of an interruption in the blood flow in areas of the brain and is characterized by the sudden development of neurological deficits that last for at least 24 hours. These deficits range from mild symptoms such as tingling, weakness, and slight speech impairment to more severe symptoms such as hemiplegia, aphasia, dysphagia, loss of portions of the visual field, spatial-perceptual changes, altered cognitive function, and loss of consciousness. Clinical manifestations depend on factors such as the area(s) of the brain affected, the adequacy of collateral cerebral circulation, and the extensiveness of subsequent cerebral edema.
A cerebrovascular accident (CVA, stroke, brain attack) is the result of an interruption in the blood flow in areas of the brain and is characterized by the sudden development of neurological deficits that last for at least 24 hours. These deficits range from mild symptoms such as tingling, weakness, and slight speech impairment to more severe symptoms such as hemiplegia, aphasia, dysphagia, loss of portions of the visual field, spatial-perceptual changes, altered cognitive function, and loss of consciousness. Clinical manifestations depend on factors such as the area(s) of the brain affected, the adequacy of collateral cerebral circulation, and the extensiveness of subsequent cerebral edema.
OUTCOME/DISCHARGE CRITERIA
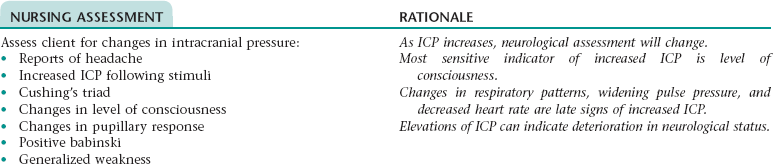
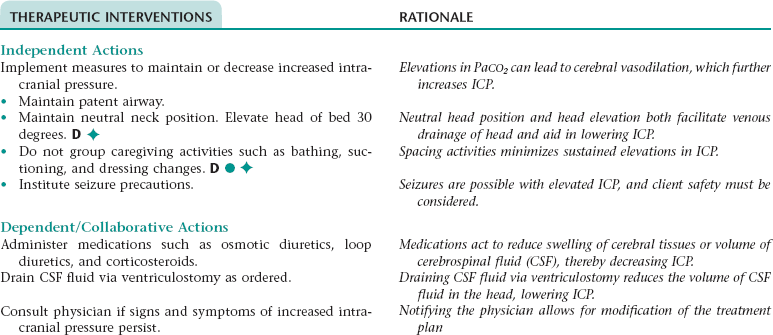
Collaborative Diagnosis DECREASED INTRACRANIAL ADAPTIVE CAPACITY RELATED TO TRAUMA/NEUROLOGICAL ILLNESS
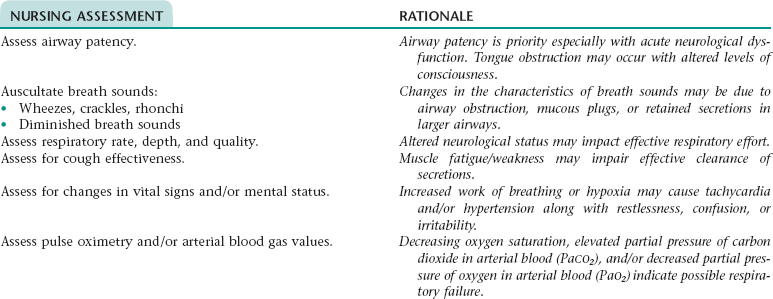
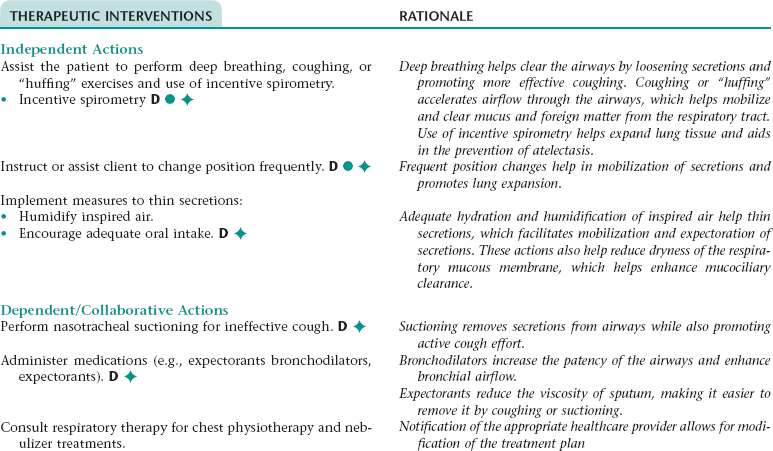
Nursing Diagnosis RISK FOR INEFFECTIVE AIRWAY CLEARANCE NDx
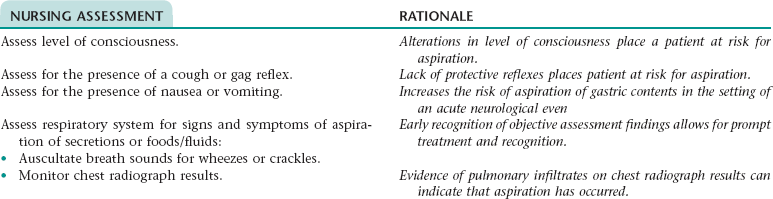
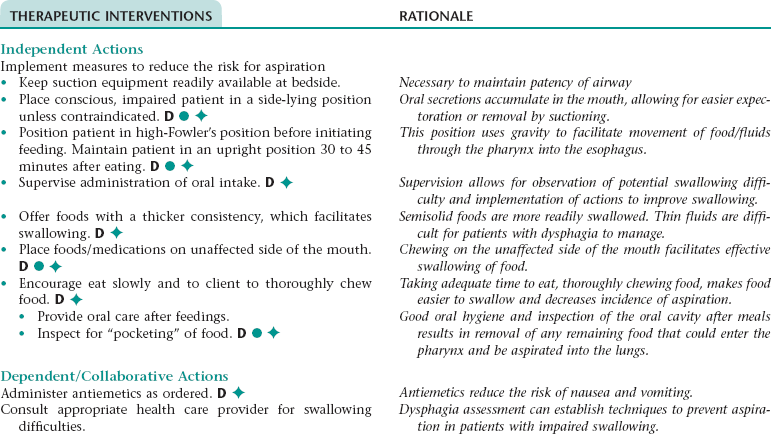
Nursing Diagnosis RISK FOR ASPIRATION NDx
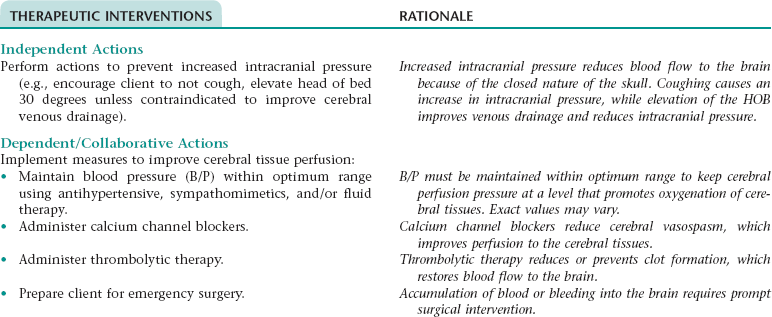
Collaborative Diagnosis INEFFECTIVE TISSUE PERFUSION: CEREBRAL NDx
NURSING ASSESSMENT
RATIONALE
Assess neurological status hourly during acute phase (e.g., dizziness, visual disturbances, aphasia, irritability, restlessness, decreased level of consciousness, paresthesias, weakness, and paralysis).
Provides baseline assessment data and determines signs of decreased tissue perfusions. Changes may be reflective of increased intracranial pressure.
Assess vital signs hourly during the acute phase.
Vitals signs must be maintained at a level that supports adequate oxygenation and perfusion of cerebral tissues.
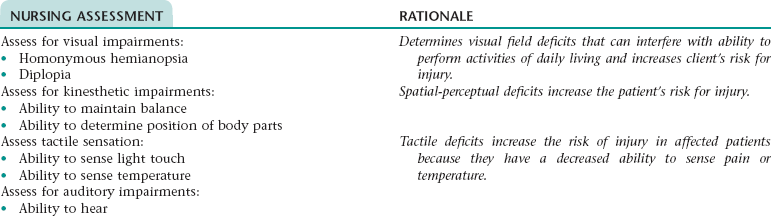
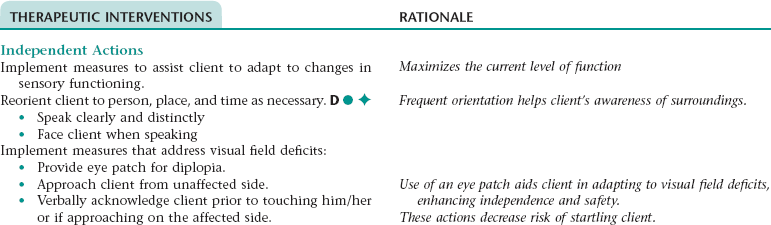
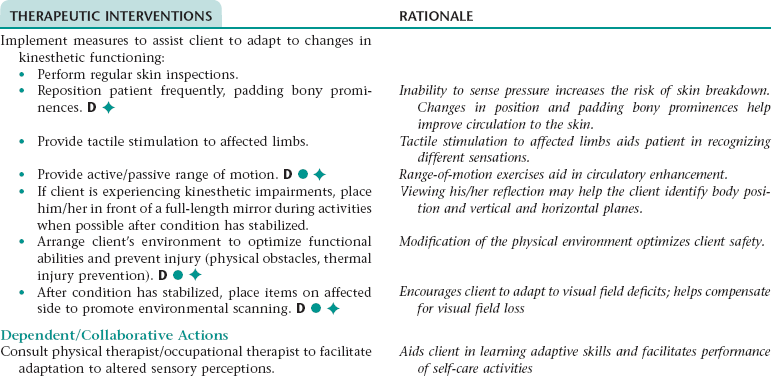
Nursing Diagnosis DISTURBED SENSORY PERCEPTION NDx (AUDITORY, KINESTHETIC, VISUAL, TACTILE)
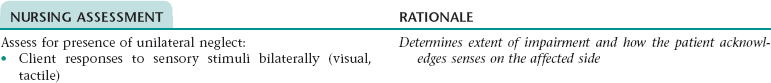
Nursing Diagnosis UNILATERAL NEGLECT NDx
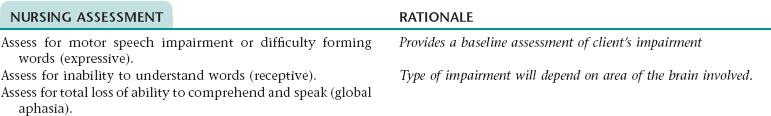
Nursing Diagnosis IMPAIRED VERBAL COMMUNICATION NDx
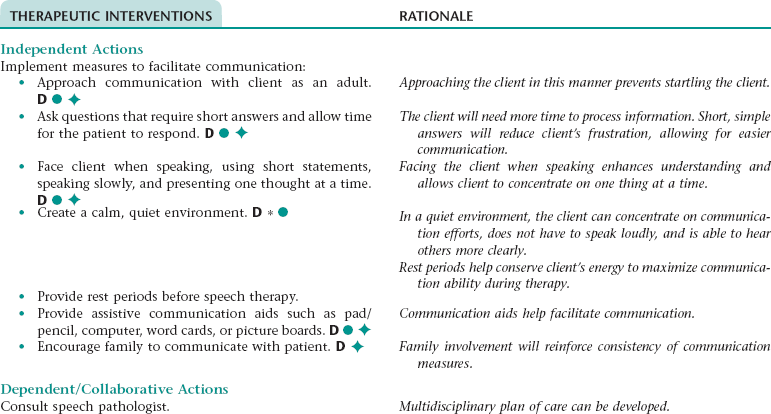
Nursing Diagnosis SELF-CARE DEFICIT NDx (BATHING, FEEDING, DRESSING, TOILETING)
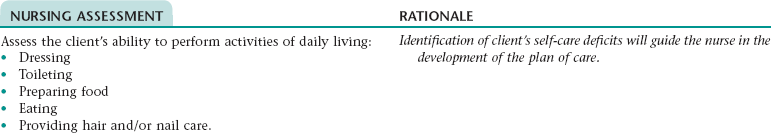
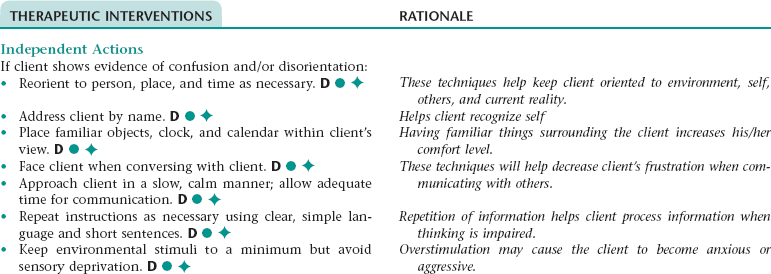
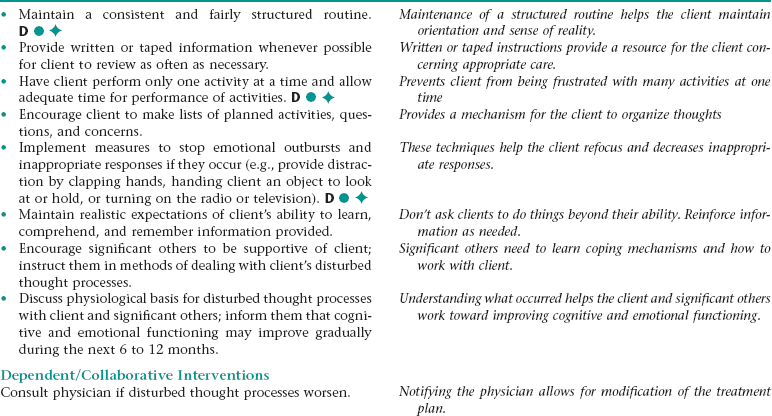
Collaborative/Nursing Diagnosis ACUTE AND CHRONIC CONFUSION NDx
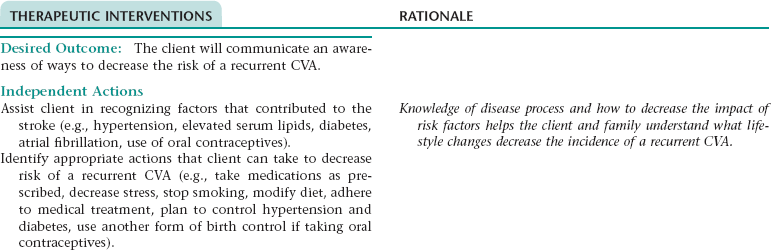
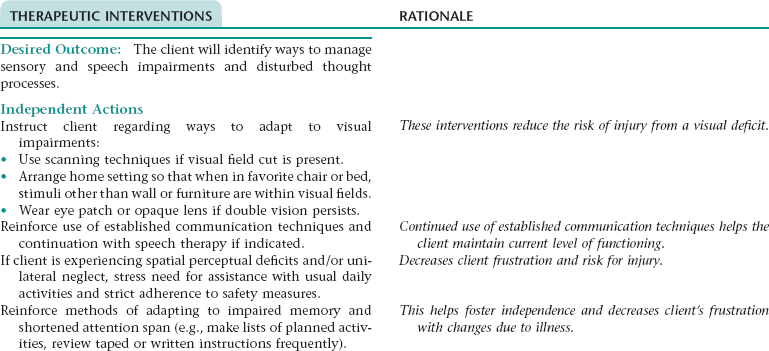
Nursing Diagnosis DEFICIENT KNOWLEDGE NDx; INEFFECTIVE FAMILY THERAPEUTIC REGIMEN MANAGEMENT NDx; OR INEFFECTIVE HEALTH MAINTENANCE* NDx
NURSING ASSESSMENT
RATIONALE
Assess for stroke-related factors that may impede the learning process.
Client may not be emotionally or physically able to learn.
Assess client/family understanding of disease process.
The nurse’s understanding of the client’s and significant other’s knowledge based aids in formulating an educational plan.
ADDITIONAL NURSING DIAGNOSES
IMBALANCED NUTRITION: LESS THAN BODY REQUIREMENTS NDx
RISK FOR CONSTIPATION NDx
POTENTIAL COMPLICATIONS OF CVA
IMPAIRED PHYSICAL MOBILITY NDx
IMPAIRED URINARY ELIMINATION: INCONTINENCE NDx
DISTURBED SELF-CONCEPT NDx
CRANIOCEREBRAL TRAUMA/CRANIOTOMY
 The leading causes of craniocerebral trauma (head injury, traumatic brain injury) are motor vehicle accidents, falls, sports/recreational injuries, and assaults. Examples of skull and brain injury that can occur include skull fracture; dural tear; cerebral contusion, concussion, and laceration; diffuse axonal injury (DAI); brainstem damage; and intracranial hemorrhage. Brain damage can occur during the initial injury and as a result of subsequent cerebral damage resulting from factors such as cerebral hematoma, infection, and edema; seizure activity; and/or obstruction of the flow of cerebrospinal fluid (CSF).
The leading causes of craniocerebral trauma (head injury, traumatic brain injury) are motor vehicle accidents, falls, sports/recreational injuries, and assaults. Examples of skull and brain injury that can occur include skull fracture; dural tear; cerebral contusion, concussion, and laceration; diffuse axonal injury (DAI); brainstem damage; and intracranial hemorrhage. Brain damage can occur during the initial injury and as a result of subsequent cerebral damage resulting from factors such as cerebral hematoma, infection, and edema; seizure activity; and/or obstruction of the flow of cerebrospinal fluid (CSF).
OUTCOME/DISCHARGE CRITERIA
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Nurse Key
Fastest Nurse Insight Engine
Get Clinical Tree app for offline access