CHAPTER 8 Diabetes* is often complicated by structural and functional abnormalities in the blood vessels and nerves. The atherosclerotic changes that frequently occur in the large vessels (macroangiopathy) affect the cardiac, cerebral, and peripheral circulation. Thickening of the basement membrane of the capillaries (microangiopathy) can also occur and is especially significant when it involves the vessels in the eyes and kidneys. The neurological involvement can be manifested in a wide variety of ways and is referred to as diabetic neuropathy. Several different mechanisms are thought to contribute to the development of diabetic neuropathy. These include reduced blood flow to the nerves as a result of angiopathies and a metabolic defect in the polyol pathway resulting in accumulation of sorbitol in the nerves, which subsequently alters nerve function. The most common neuropathy is peripheral sensorimotor polyneuropathy, which has a gradual onset of sensory manifestations such as numbness and tingling, burning or shooting pain sensations, and/or hyperesthesia. Neuropathy of the autonomic nervous system is also common. 1. Have blood glucose stabilized within a desired range 2. Have signs and symptoms of vascular and neurological complications at a manageable level 3. Verbalize a basic understanding of diabetes mellitus 4. Verbalize an understanding of medications ordered and demonstrate the ability to correctly draw up and administer insulin if prescribed 5. Verbalize an understanding of the principles of dietary management and be able to calculate and plan meals within the prescribed caloric distribution 6. Demonstrate the ability to perform blood glucose and urine tests correctly and interpret results accurately 7. Verbalize an understanding of the role of exercise in the management of diabetes 8. Identify health care and hygiene practices that should be integrated into lifestyle 9. Identify appropriate safety measures to follow because of the diagnosis of diabetes 10. State signs and symptoms of hypoglycemia and ketoacidosis and appropriate actions for prevention and treatment 11. State signs and symptoms to report to the health care provider 12. Share feelings and concerns about diabetes and its effect on lifestyle 13. Identify resources that can assist in the adjustment to and management of diabetes 14. Verbalize an understanding of and a plan for adhering to recommended follow-up care including future appointments with health care provider and for laboratory studies. Definition: Risk for variation of blood glucose/sugar levels from the normal range • Inadequate insulin production • Insulin resistance that may lead to generalized vascular disease and neuropathy • Inability of the client to adhere to the diabetic regimen • Lack of knowledge of diabetes management • Inappropriate dietary intake • Inadequate medication management DESIRED OUTCOMES: The client will experience normal or near-normal blood glucose levels as evidenced by: NOC OUTCOMES: Tissue perfusion: cardiac; tissue perfusion: cerebral; tissue perfusion: abdominal organs; tissue perfusion: peripheral tissue integrity; skin and mucous membranes • Osmotic swelling of the lens associated with hyperglycemia • Changes in the retinal vessels (retinopathy) • Presence of cataracts (there is an increased incidence of cataract formation in persons with diabetes) DESIRED OUTCOMES: The client will not experience ketoacidosis as evidenced by: • Lack of understanding of the implications of not following the prescribed treatment plan • Feeling of lack of control over disease progression despite efforts to follow prescribed treatment plan • Difficulty modifying personal habits and integrating necessary treatments and dietary regimen into lifestyle DESIRED OUTCOMES: The client will demonstrate the probability of effective therapeutic regimen management as evidenced by: NOC OUTCOMES: Compliance behavior; diabetes self-management; treatment behavior: illness or injury; knowledge: treatment regimen; health beliefs: perceived resources; health beliefs: perceived ability to perform NOC OUTCOMES: Knowledge: treatment regimen; knowledge: health behavior; knowledge: health resources; knowledge: treatment procedure(s)
The Client with Alterations in Metabolic Function
DIABETES MELLITUS
OUTCOME/DISCHARGE CRITERIA
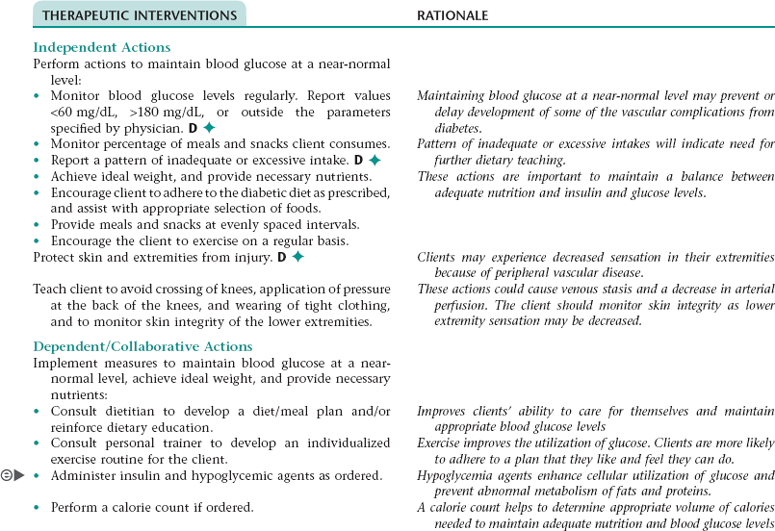
Collaborative Diagnosis RISK FOR UNSTABLE BLOOD GLUCOSE LEVEL NDx
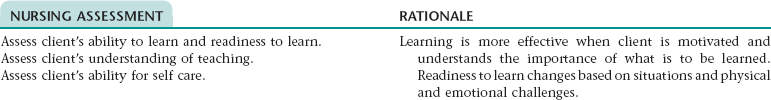
NURSING ASSESSMENT
RATIONALE
Assess blood glucose levels before meals and at bedtime.
Monitoring the client’s blood glucose levels determines effectiveness of glucose control and allows for prompt treatment as needed.
Assess for increased blood pressure (B/P).
Hypertension is frequently associated with diabetes. Control of B/P is associated with decreased incidence of or limited development of heart disease, stroke, retinopathy, and nephropathy.
Assess for capillary refill, temperature, peripheral pulses, and color.
Monitors adequate peripheral vascular perfusion and aids in detection of peripheral vascular disease
Assess for increased or decreased urine output and excessive complaints of thirst and hunger.
Indicators that the individual may be experiencing increased blood glucose levels
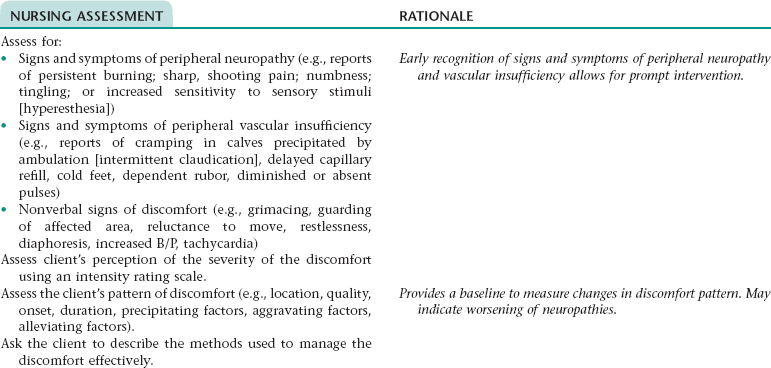
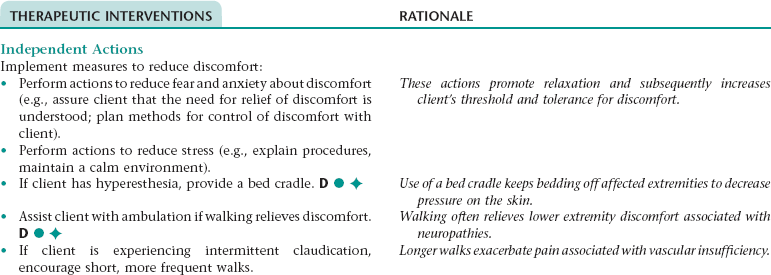
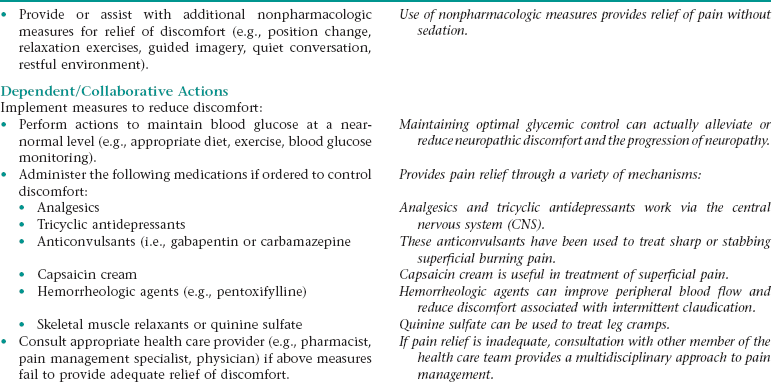
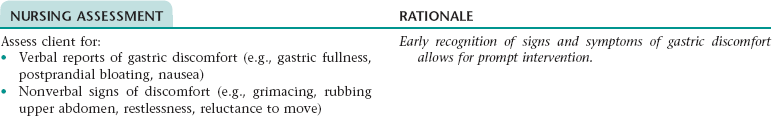
Nursing Diagnosis IMPAIRED COMFORT NDx (BURNING, ACHING, CRAMPING, HYPERESTHESIA, NUMBNESS, AND/OR TINGLING [PARTICULARLY IN LOWER EXTREMITIES])
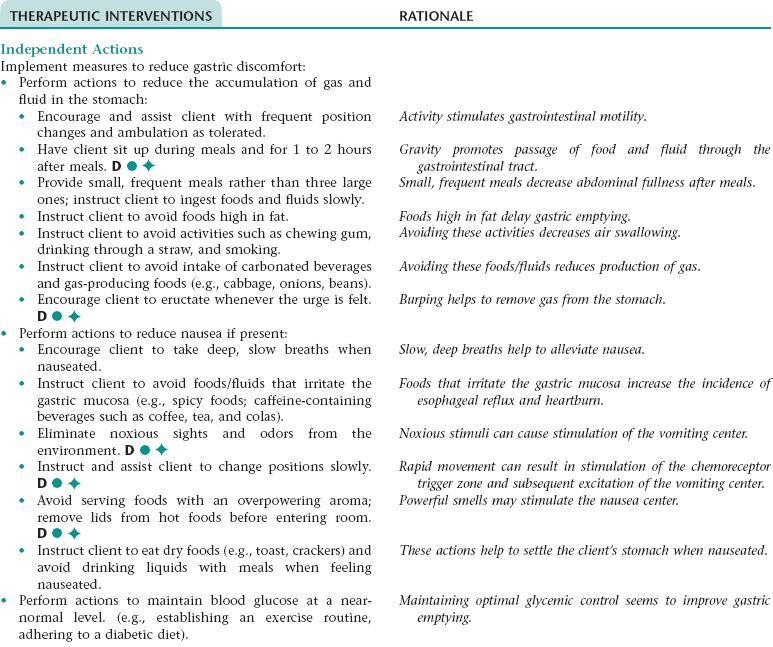
Nursing Diagnosis RISK FOR DYSFUNCTIONAL GASTROINTESTINAL MOTILITY NDx
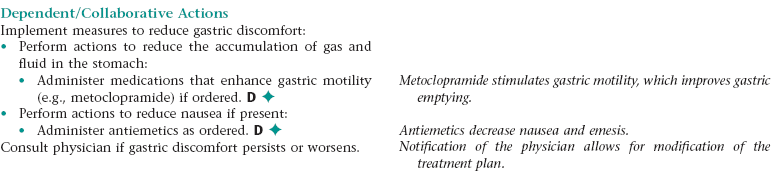
Nursing Diagnosis DISTURBED SENSORY PERCEPTION NDx (VISUAL)
NURSING ASSESSMENT
RATIONALE
Assess for visual disturbances (e.g., reports of blurred vision; partial or total loss of vision; the presence of “floaters,” spots, or flashing lights).
Diabetes is the number one cause of blindness in the United States. Early recognition and treatment may prevent or delay visual changes from occurring.
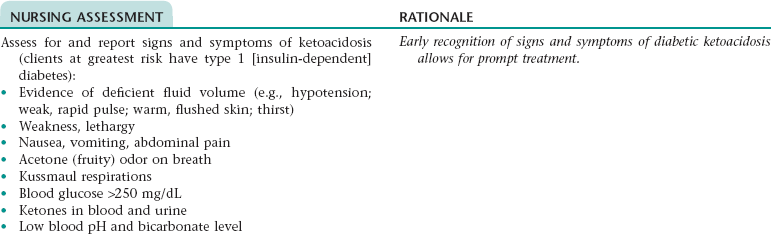
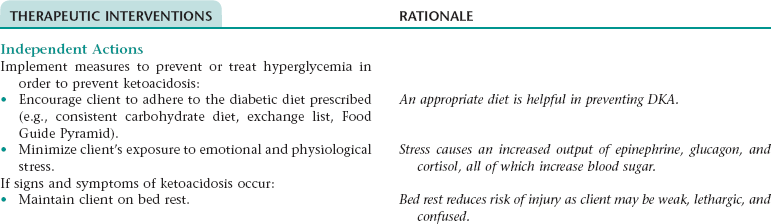
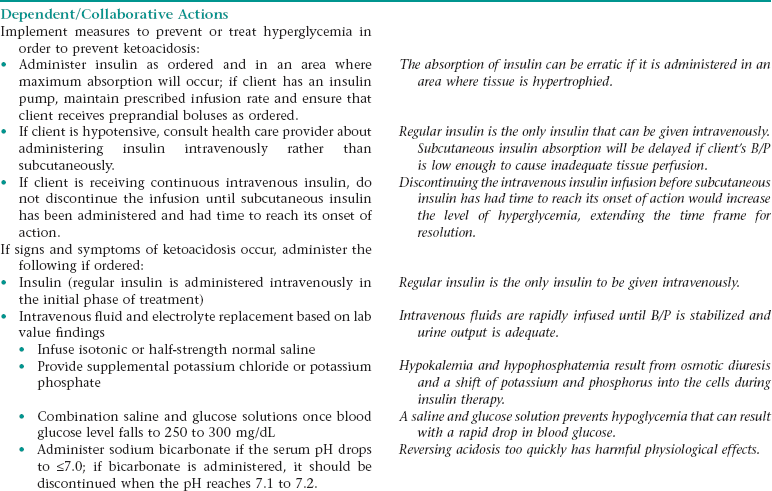
Collaborative Diagnosis RISK FOR DIABETIC KETOACIDOSIS (DKA)
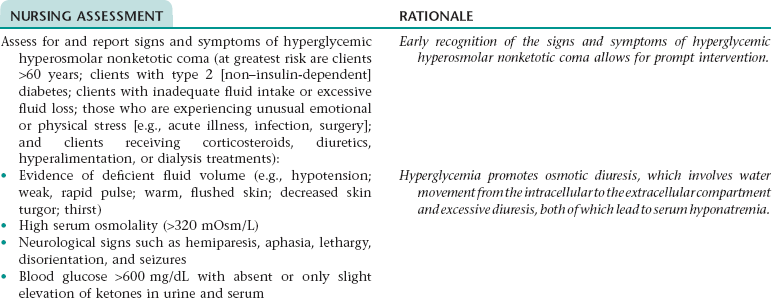
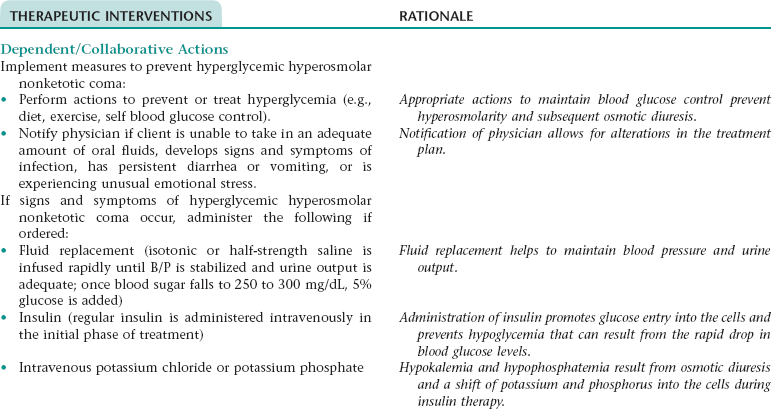
Collaborative Diagnosis RISK FOR HYPERGLYCEMIC HYPEROSMOLAR NONKETOTIC COMA (SYNDROME)
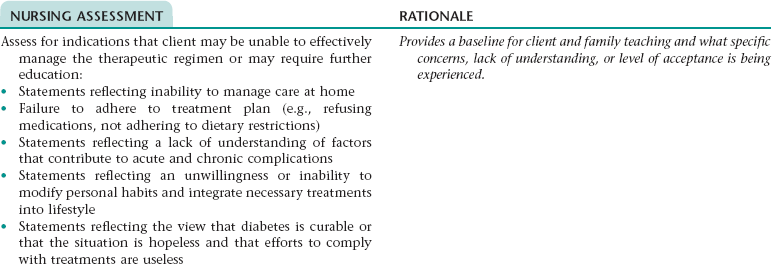
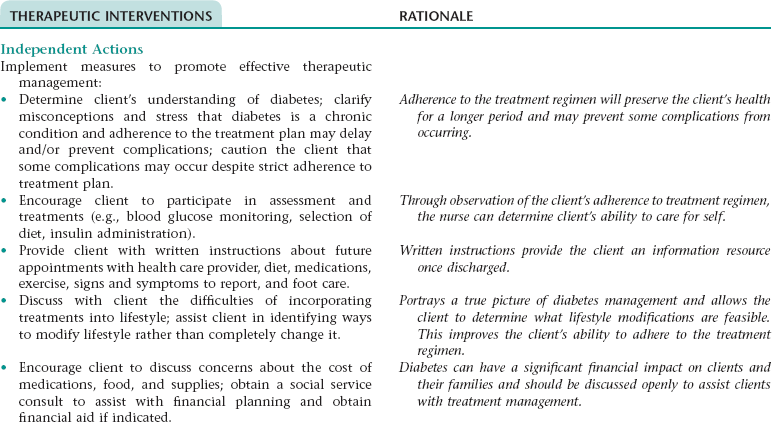
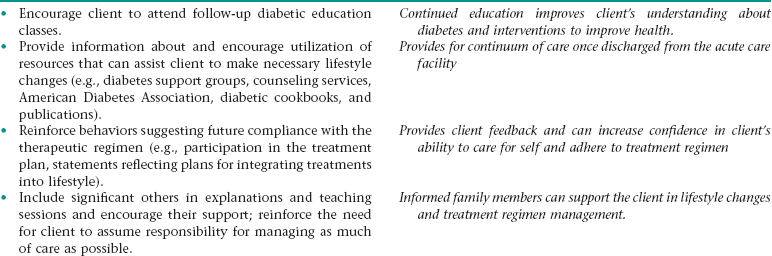
Nursing Diagnosis INEFFECTIVE FAMILY THERAPEUTIC REGIMEN MANAGEMENT NDx
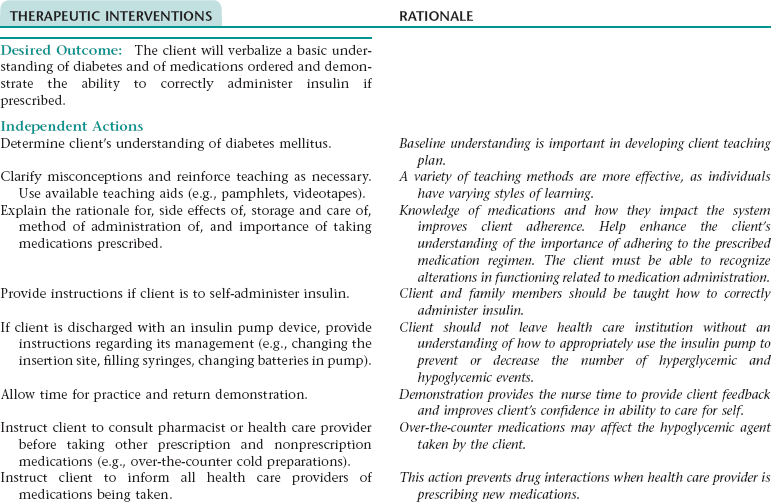
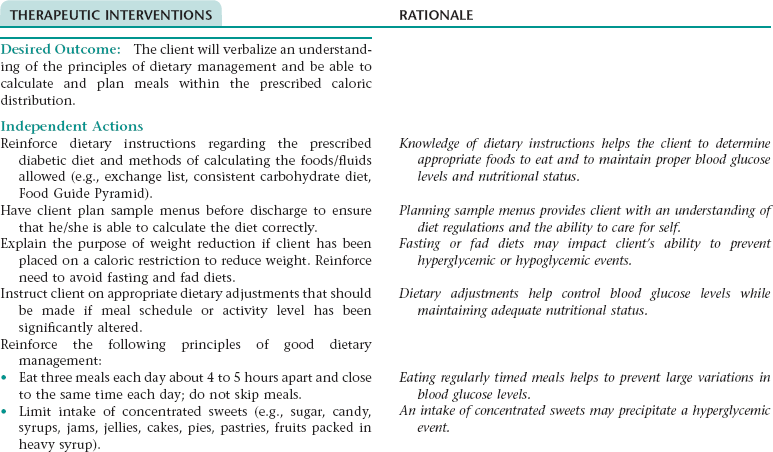
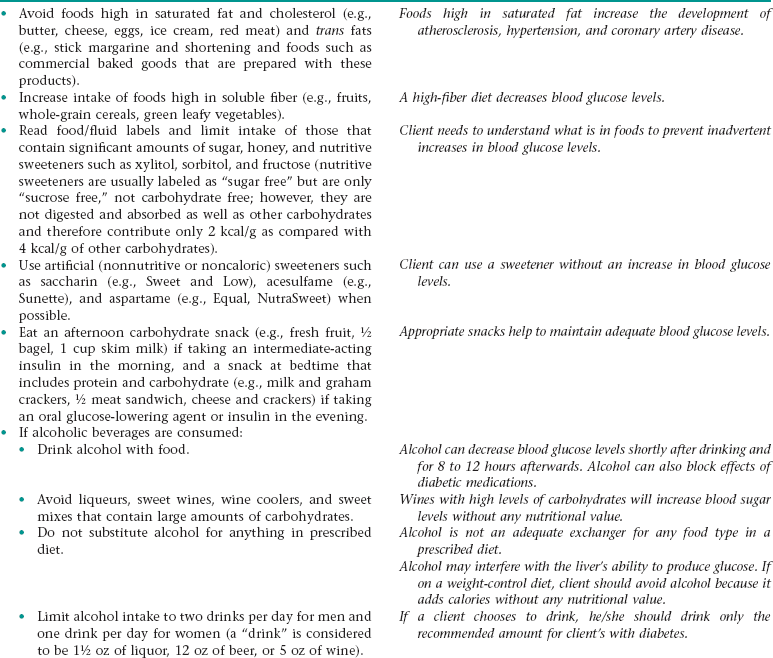
Nursing Diagnosis DEFICIENT KNOWLEDGE NDx OR INEFFECTIVE SELF HEALTH MANAGEMENT* NDx
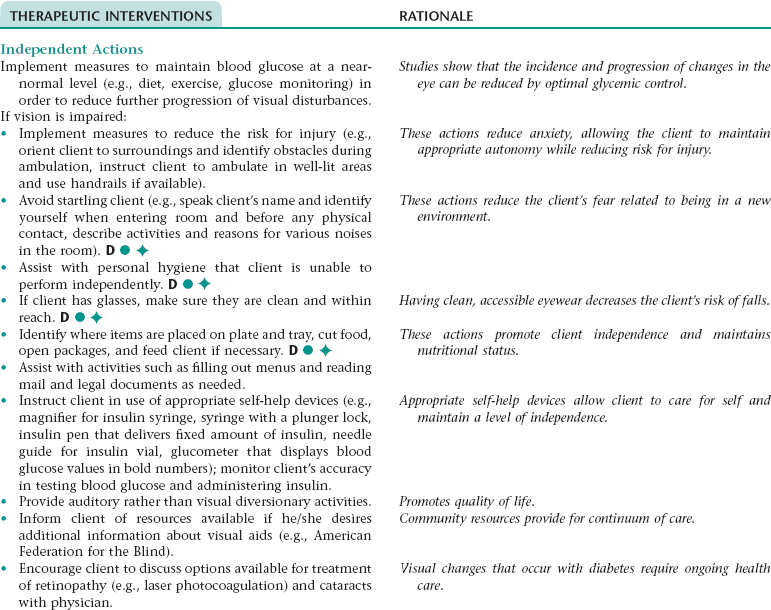
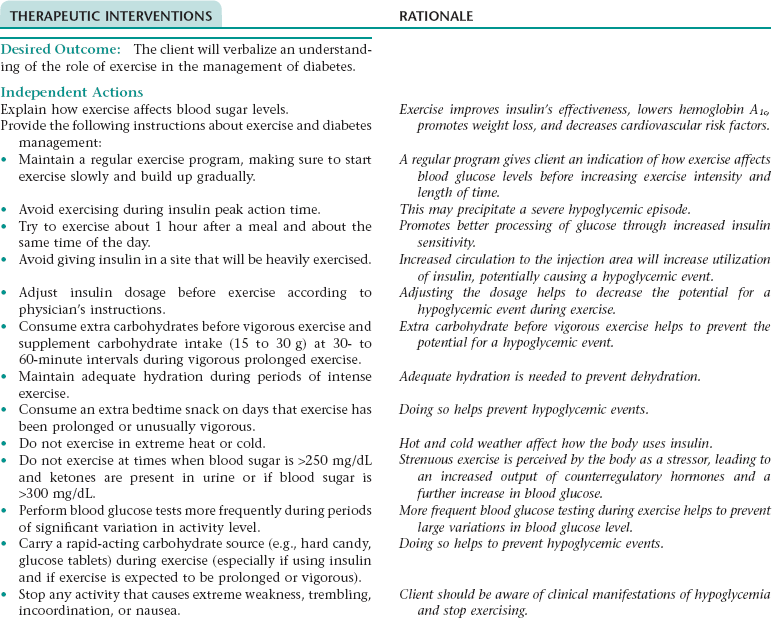
THERAPEUTIC INTERVENTIONS
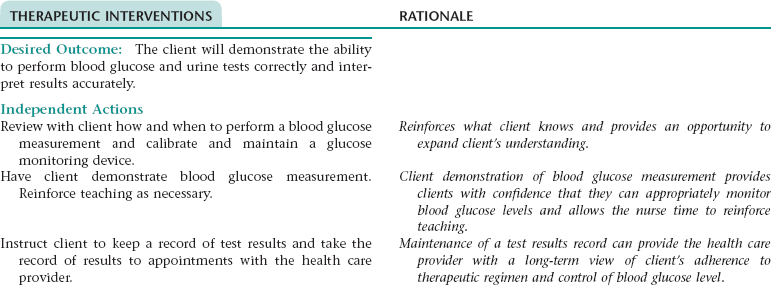
RATIONALE
Provide instructions on actions client should take when test results are abnormal (some clients are instructed to adjust insulin dose and dietary intake; others are instructed to notify appropriate health care provider)
Written instructions provide an ongoing resource for client to use in controlling blood glucose level.
The Client with Alterations in Metabolic Function
Get Clinical Tree app for offline access