CHAPTER 7 The antiretroviral agents used to control viral replication of HIV include nucleoside reverse transcriptase inhibitors (e.g., zidovudine, lamivudine, zalcitabine, abacavir, didanosine, stavudine), protease inhibitors (e.g., saquinavir, ritonavir, indinavir, amprenavir, nelfinavir), nonnucleoside reverse transcriptase inhibitors (e.g., nevirapine, delavirdine, efavirenz), and fusion inhibitors (e.g., enfuvirtide). Chemoprophylactic therapy to prevent AIDS-defining opportunistic infections has also led to a significant decline in the incidence of certain diseases such as PCP, MAC, tuberculosis, and toxoplasmosis. 1. Have an adequate respiratory status 2. Have an adequate or improved nutritional status 3. Be able to perform activities of daily living without undue fatigue or dyspnea 4. Demonstrate evidence that opportunistic infection is resolving 5. Be effectively managing the signs and symptoms of neurological dysfunction 6. Have discomfort at a manageable level 7. Show evidence that skin and oral mucous membranes are intact or healing appropriately 8. Have fewer episodes of diarrhea 9. Identify ways to prevent the spread of HIV 10. Identify ways to decrease the risk for developing opportunistic infections 11. Verbalize ways to maintain an optimal nutritional status 12. State signs and symptoms to report to the health care provider 13. Share feelings about changes in mental and physical functioning and the social isolation and loneliness that may result from having AIDS 14. Identify resources that can assist with financial needs and adjustment to changes resulting from the diagnosis of AIDS 15. Verbalize an understanding of and a plan for adhering to recommended follow-up care including regular laboratory studies, future appointments with health care providers, and medications prescribed. Ineffective breathing pattern NDx related to: • Decreased depth of respirations associated with fear, anxiety, weakness, fatigue, and chest pain if present • Increased rate of respirations associated with fear, anxiety, and the increase in metabolic rate that occurs with infection Ineffective airway clearance NDx related to: • Increased production of secretions associated with some opportunistic infections of the lungs • Stasis of secretions associated with decreased activity and poor cough effort resulting from fatigue and pain Impaired gas exchange NDx related to a decrease in effective lung surface associated with: • The presence of infiltrates and/or cavities in the lung tissue resulting from opportunistic infection of the lungs (e.g., PCP, pneumococcal pneumonia, tuberculosis, histoplasmosis) • Compression and/or replacement of lung tissue if an AIDS-related cancer such as Kaposi’s sarcoma or non-Hodgkin’s lymphoma is present NOC OUTCOMES: Respiratory status: airway patency; respiratory status: ventilation; respiratory status: gas exchange • Cranial inflammation/pressure associated with an opportunistic infection involving the sinuses or brain or the presence of a cerebral neoplasm • Inflammation of the parietal pleura associated with an opportunistic infection of the lungs • Muscle strain associated with excessive coughing if present Skin and local tissue pain related to: Definition: Intake of nutrients insufficient to meet metabolic demands • Decreased oral intake associated with: • Anorexia resulting from malaise, fatigue, fear, anxiety, pain, depression, increased levels of certain cytokines that depress appetite (e.g., tumor necrosis factor [TNF]), and some antiretroviral agents • Nausea, dyspnea, and cognitive impairment if present • Oral pain and/or dysphagia resulting from opportunistic lesions in the mouth, pharynx, and esophagus • Impaired utilization of nutrients associated with: • Accelerated and inefficient metabolism of nutrients resulting from an increased resting energy expenditure that occurs with infection and increased levels of certain cytokines (e.g., TNF, interleukin-1) • Decreased absorption of nutrients if HIV and/or opportunistic infection involve the intestine • Loss of nutrients associated with persistent diarrhea and vomiting if present • Deficient fluid volume NDx related to: • Excessive loss of fluid associated with diarrhea, diaphoresis, and vomiting if present • Decreased oral intake associated with anorexia, weakness, nausea, and oropharyngeal pain • Excessive loss of sodium associated with diarrhea, profuse diaphoresis, and vomiting if present • Excessive loss of sodium associated with diarrhea, profuse diaphoresis, and vomiting if present • Water retention associated with increased antidiuretic hormone (ADH) output resulting from opportunistic disease involvement of the lungs or central nervous system DESIRED OUTCOMES: The client will maintain fluid and electrolyte balance as evidenced by: d. B/P and pulse within normal range for client and stable with position change e. Capillary refill time less than 2 to 3 seconds i. Soft, nondistended abdomen with normal bowel sounds j. Absence of nausea, vomiting, abdominal cramps, and seizure activity k. BUN, Hct, and serum potassium and sodium levels within normal range Definition: Body temperature elevated above normal range • Difficulty resting and sleeping • Increased energy utilization associated with the elevated metabolic rate that is present with infection • Tissue hypoxia associated with: • Impaired alveolar gas exchange if respiratory infection is present • HIV or opportunistic disease involvement of erythroid precursors in the bone marrow • Treatment with medications that can cause bone marrow depression or red blood cell (RBC) hemolysis (e.g., zidovudine, antineoplastic agents, trimethoprim-sulfamethoxazole [TMP-SMX]) • Vitamin B12 or folate deficiency (a result of malabsorption if intestinal involvement is present) • Overwhelming emotional demands associated with the diagnosis of AIDS • Side effects of some medications client may be receiving (e.g., narcotic [opioid] analgesics, antiemetics, antianxiety or antipsychotic agents)
The Client with Alterations in Hematologic and Immune Function
HUMAN IMMUNODEFICIENCY VIRUS (HIV) INFECTION AND ACQUIRED IMMUNE DEFICIENCY SYNDROME (AIDS)
 Acquired immune deficiency syndrome (AIDS) is an infectious disease of the immune system and is considered to be the last phase of the clinical spectrum of infection by the human immunodeficiency virus (HIV). HIV is a retrovirus that affects the cells in the body that have a CD4 receptor on their surface. The types of cells that have the CD4 receptor and can be infected by the virus include lymphocytes, monocytes, macrophages, glial cells, bone marrow progenitors, and gut-associated lymphoid tissue. The CD4+ T lymphocytes (also called T4 or T-helper cells) have the greatest number of CD4 receptors and are consequently the major target of HIV. These lymphocytes are ultimately destroyed by HIV, which results in severely impaired cell-mediated immunity in the host. Humoral immune function is also impaired because the B lymphocytes are unable to respond appropriately to the presence of a new antigen without the help of normal CD4+ T lymphocytes. The effect of HIV on the monocyte and macrophage further depresses immune system function.
Acquired immune deficiency syndrome (AIDS) is an infectious disease of the immune system and is considered to be the last phase of the clinical spectrum of infection by the human immunodeficiency virus (HIV). HIV is a retrovirus that affects the cells in the body that have a CD4 receptor on their surface. The types of cells that have the CD4 receptor and can be infected by the virus include lymphocytes, monocytes, macrophages, glial cells, bone marrow progenitors, and gut-associated lymphoid tissue. The CD4+ T lymphocytes (also called T4 or T-helper cells) have the greatest number of CD4 receptors and are consequently the major target of HIV. These lymphocytes are ultimately destroyed by HIV, which results in severely impaired cell-mediated immunity in the host. Humoral immune function is also impaired because the B lymphocytes are unable to respond appropriately to the presence of a new antigen without the help of normal CD4+ T lymphocytes. The effect of HIV on the monocyte and macrophage further depresses immune system function.
OUTCOME/DISCHARGE CRITERIA
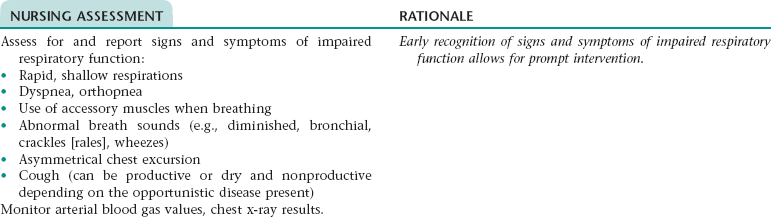
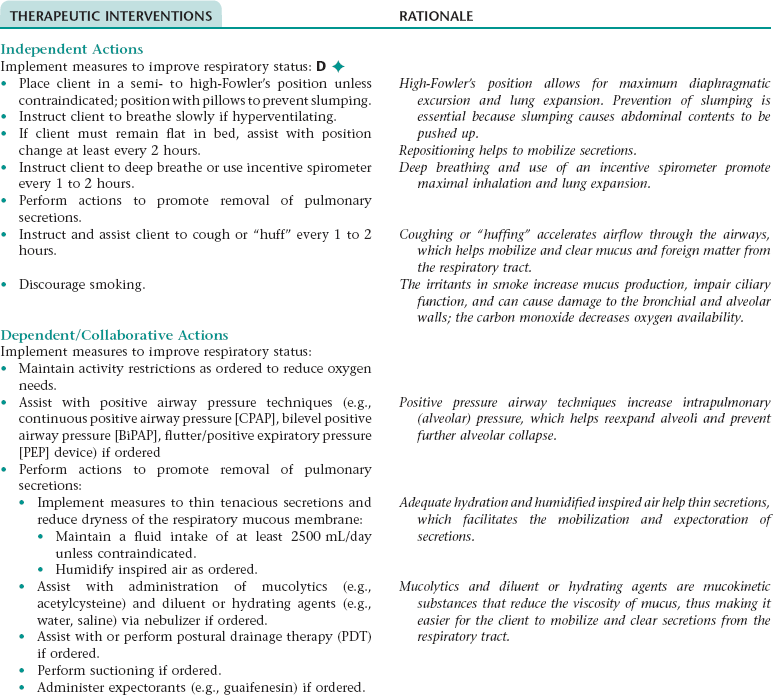
Nursing Diagnosis IMPAIRED RESPIRATORY FUNCTION*
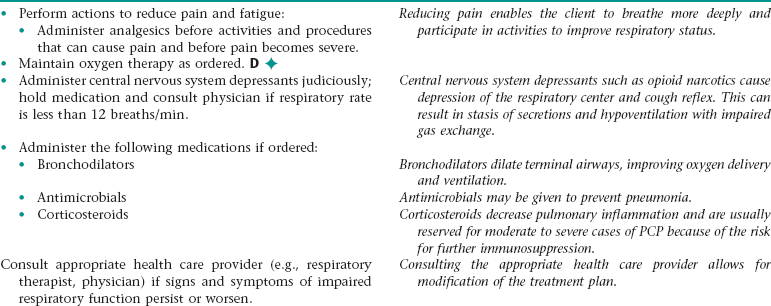
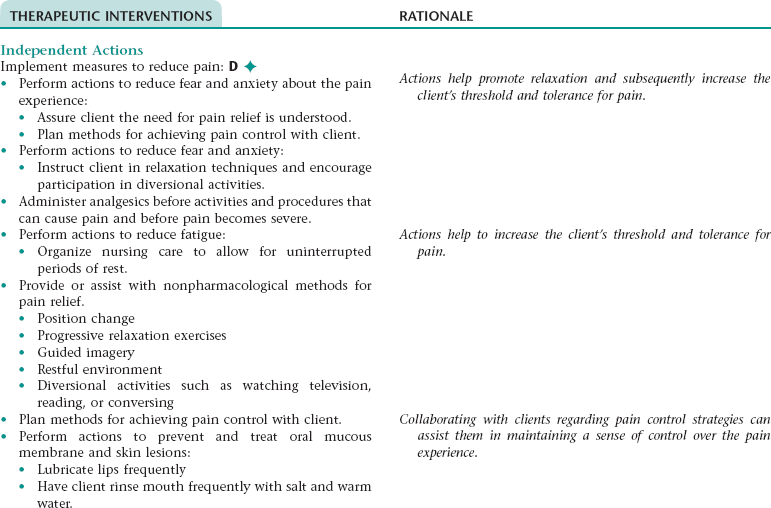
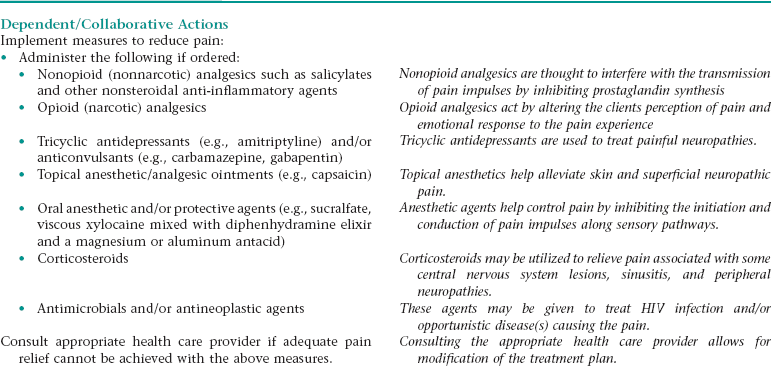
Nursing Diagnosis ACUTE/CHRONIC PAIN NDx
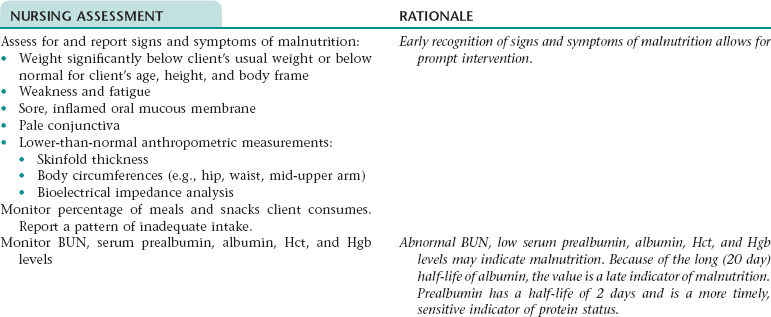
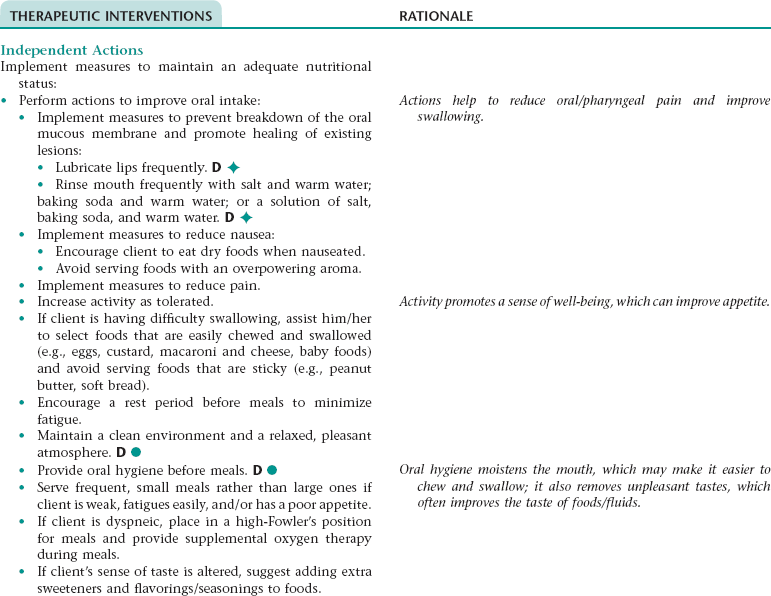
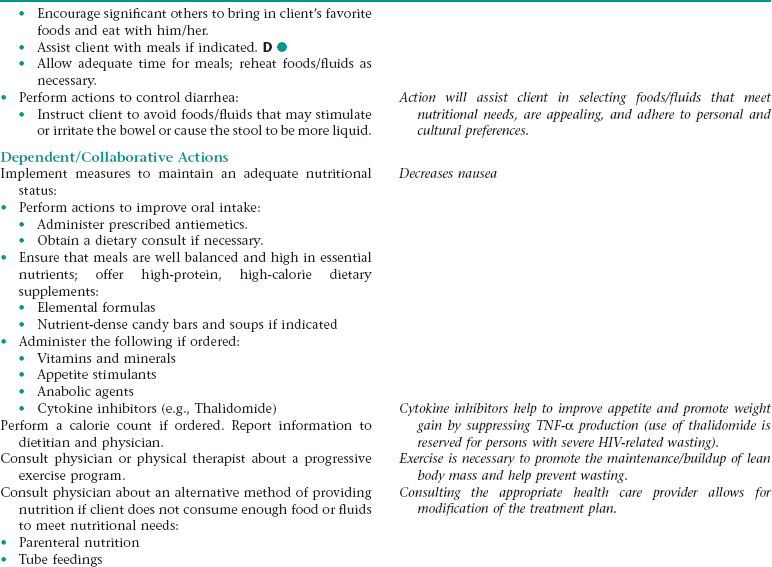
Nursing Diagnosis IMBALANCED NUTRITION: LESS THAN BODY REQUIREMENTS NDx
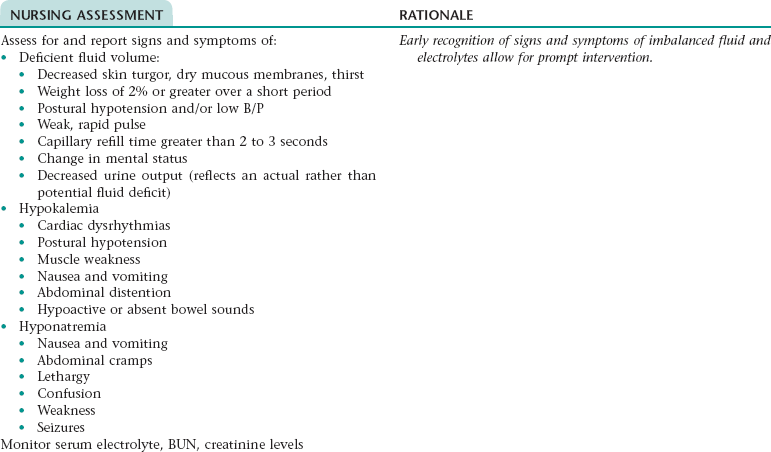
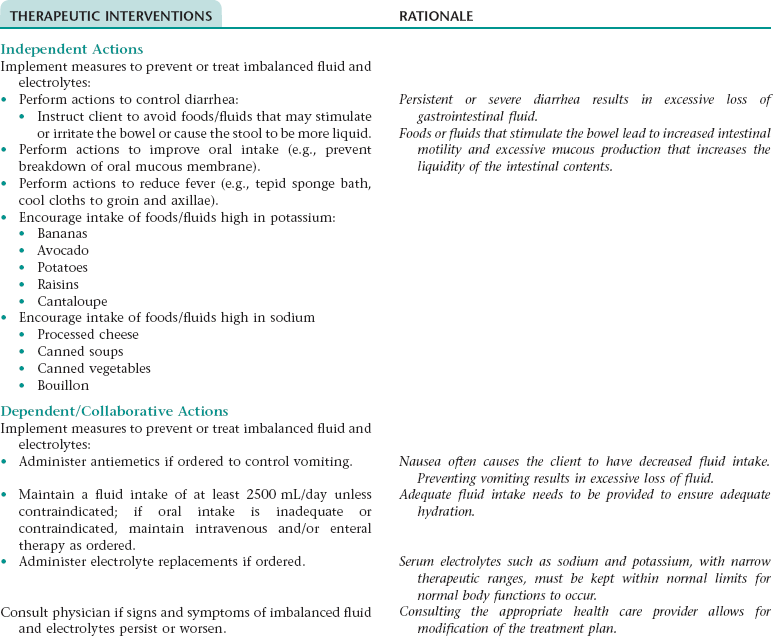
Nursing Diagnosis RISK FOR IMBALANCED FLUID VOLUME NDx AND RISK FOR ELECTROLYTE IMBALANCE NDx
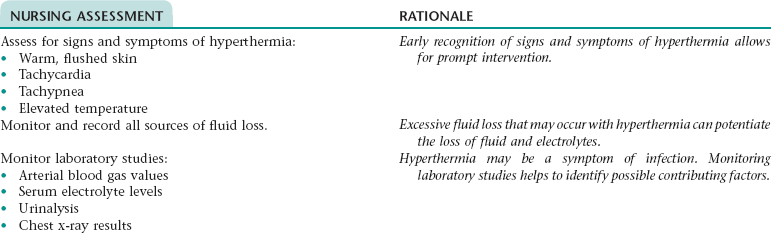
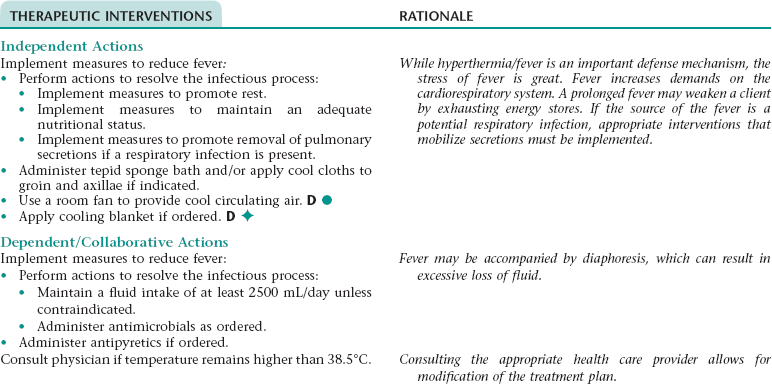
Nursing Diagnosis HYPERTHERMIA NDx
Nursing Diagnosis FATIGUE NDx
Subjective
Objective
Verbalization of overwhelming lack of energy; tired; increase in physical complaints; compromised libido; inability to restore energy even after sleep
Lethargic or listless; drowsy; compromised concentration; disinterest in surroundings; decreased performance ![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree