Chapter 27 The Baby at Birth
Adaptation to extrauterine life
Respiratory and cardiovascular changes are interdependent and concurrent.
Pulmonary adaptation
 During birth, this fluid leaves the alveoli, either by being squeezed up the airway and out of the mouth and nose, or by moving across the alveolar walls into the pulmonary lymphatic vessels and into the thoracic duct, or to the lung capillaries.
During birth, this fluid leaves the alveoli, either by being squeezed up the airway and out of the mouth and nose, or by moving across the alveolar walls into the pulmonary lymphatic vessels and into the thoracic duct, or to the lung capillaries.
 Stimuli to respiration include the mild hypercapnia, hypoxia and acidosis that result from normal labour, due partially to the intermittent cessation of maternal–placental perfusion with contractions. The rhythm of respiration changes from episodic shallow fetal respiration to regular deeper breathing, as a result of a combination of chemical and neural stimuli: notably, a fall in pH and PaO2 and a rise in PaCO2. Other stimuli include cold, light, noise, touch and pain.
Stimuli to respiration include the mild hypercapnia, hypoxia and acidosis that result from normal labour, due partially to the intermittent cessation of maternal–placental perfusion with contractions. The rhythm of respiration changes from episodic shallow fetal respiration to regular deeper breathing, as a result of a combination of chemical and neural stimuli: notably, a fall in pH and PaO2 and a rise in PaCO2. Other stimuli include cold, light, noise, touch and pain.
 Considerable negative intrathoracic pressure of up to 9.8 kPa (100 cm water) is exerted as the first breath is taken. Pressure exerted to effect inhalation diminishes with each breath taken until only 5 cm water pressure is required to inflate the lungs. This is an effect of surfactant, which lines the alveoli, lowering surface tension thus permitting residual air to remain in the alveoli between breaths. Surfactant is a complex of lipoproteins and proteins produced by the alveolar type 2 cells in the lungs; it is primarily concerned with the reduction in surface tension at the alveolar surface, thus reducing the work of breathing.
Considerable negative intrathoracic pressure of up to 9.8 kPa (100 cm water) is exerted as the first breath is taken. Pressure exerted to effect inhalation diminishes with each breath taken until only 5 cm water pressure is required to inflate the lungs. This is an effect of surfactant, which lines the alveoli, lowering surface tension thus permitting residual air to remain in the alveoli between breaths. Surfactant is a complex of lipoproteins and proteins produced by the alveolar type 2 cells in the lungs; it is primarily concerned with the reduction in surface tension at the alveolar surface, thus reducing the work of breathing.
Cardiovascular adaptation
 With the expansion of the lungs and lowered pulmonary vascular resistance, virtually all of the cardiac output is sent to the lungs.
With the expansion of the lungs and lowered pulmonary vascular resistance, virtually all of the cardiac output is sent to the lungs.
 Oxygenated blood returning to the heart from the lungs increases the pressure within the left atrium.
Oxygenated blood returning to the heart from the lungs increases the pressure within the left atrium.
 Pressure in the right atrium is lowered because blood ceases to flow through the cord.
Pressure in the right atrium is lowered because blood ceases to flow through the cord.
 A functional closure of the foramen ovale takes place. During the first days of life this closure is reversible and reopening may occur if pulmonary vascular resistance is high – e.g. when crying – resulting in transient cyanotic episodes in the baby.
A functional closure of the foramen ovale takes place. During the first days of life this closure is reversible and reopening may occur if pulmonary vascular resistance is high – e.g. when crying – resulting in transient cyanotic episodes in the baby.
 The septa usually fuse within the first year of life to form the interatrial septum, though in some individuals perfect anatomical closure may never be achieved.
The septa usually fuse within the first year of life to form the interatrial septum, though in some individuals perfect anatomical closure may never be achieved.
 Contraction of the muscular walls of the ductus arteriosus takes place; this is thought to occur because of sensitivity of the muscle of the ductus arteriosus to increased oxygen tension and reduction in circulating prostaglandin. As a result of altered pressure gradients between the aorta and pulmonary artery, a temporary reverse left-to-right shunt through the ductus may persist for a few hours, though there is usually functional closure of the ductus within 8–10 hours of birth.
Contraction of the muscular walls of the ductus arteriosus takes place; this is thought to occur because of sensitivity of the muscle of the ductus arteriosus to increased oxygen tension and reduction in circulating prostaglandin. As a result of altered pressure gradients between the aorta and pulmonary artery, a temporary reverse left-to-right shunt through the ductus may persist for a few hours, though there is usually functional closure of the ductus within 8–10 hours of birth.
 The remaining temporary structures of the fetal circulation – the umbilical vein, ductus venosus and hypogastric arteries – close functionally within a few minutes after birth and constriction of the cord. Anatomical closure by fibrous tissue occurs within 2–3 months, resulting in the formation of the ligamentum teres, ligamentum venosum and the obliterated hypogastric arteries. The proximal portions of the hypogastric arteries persist as the superior vesical arteries.
The remaining temporary structures of the fetal circulation – the umbilical vein, ductus venosus and hypogastric arteries – close functionally within a few minutes after birth and constriction of the cord. Anatomical closure by fibrous tissue occurs within 2–3 months, resulting in the formation of the ligamentum teres, ligamentum venosum and the obliterated hypogastric arteries. The proximal portions of the hypogastric arteries persist as the superior vesical arteries.
Thermal adaptation
The baby enters a much cooler atmosphere, the birthing room temperature of 21°C contrasting sharply with an intrauterine temperature of 37.7°C. Heat loss can be rapid, and takes place through the mechanisms listed in Box 27.1.
Immediate care of the baby at birth
Cutting the cord
 if a preterm baby is held above the placenta, blood can drain from the baby to the placenta, resulting in anaemia
if a preterm baby is held above the placenta, blood can drain from the baby to the placenta, resulting in anaemia
 if the baby is held below the placenta, it can cause him or her to receive a blood transfusion.
if the baby is held below the placenta, it can cause him or her to receive a blood transfusion.
Early clamping and cutting of the cord is advocated in preterm babies.
Assessment of the baby’s condition
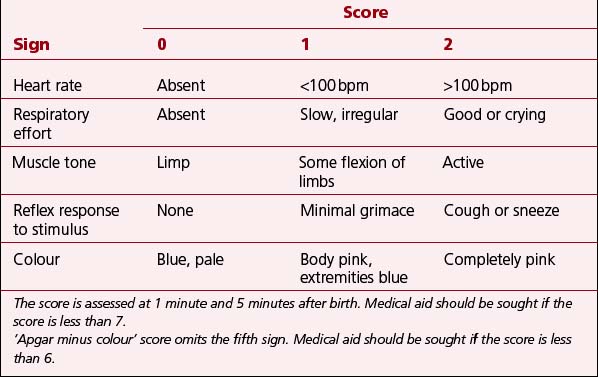
At 1 minute and 5 minutes after the birth, an assessment is made of the baby’s general condition using the Apgar score (Table 27.1).
 The assessment at 1 minute is important for the further management of resuscitation.
The assessment at 1 minute is important for the further management of resuscitation.
 An assessment at 5 minutes provides a record of response to resuscitation and immediate care needs.
An assessment at 5 minutes provides a record of response to resuscitation and immediate care needs.
 The higher the score, the better the outcome for the baby. A mnemonic – APGAR – for the Apgar score is given in Box 27.2.
The higher the score, the better the outcome for the baby. A mnemonic – APGAR – for the Apgar score is given in Box 27.2.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree