Targeting the right population with the right services
The ICM model is designed to provide specialized care management services to two larger groups of individuals that fall into complementary subdivisions of the Medicaid population: (1) complex, high-risk members; and (2) members that require various levels of episodic supportive care management services. A key feature of the ICM model is the strategic identification of a small subset of individuals with the most complex needs and fragmented care patterns for Intensive Care Management. Care management for these members is characterized by a longer-term relationship with a single clinical care manager who maintains a lower caseload solely dedicated to managing complex, high-risk members. Intensive Care Management services provided to complex, high-risk members, are frequent, high-touch (face-to-face), and sustained for long periods of time (typically several months) to ensure that members reach optimal stabilization and are moved into a lower risk stratification. Members in this group have most of their care management services coordinated by a clinical care manager, but as a member progresses toward stabilization and self-management, coordination needs can be met by non-clinical staff to ensure clinicians on the care team focus on clinical care management activities.
The Supportive Care Management category consists of individuals that have a single complex care issue or several less intensive care issues that will stabilize or resolve within a shorter period of time and require fairly straightforward problem-solving. Supportive Care Management services focus on standard, targeted interventions for specific health or other care issues that may require varied intensity but services are typically more limited in scope and frequency. For example, an individual whose overall health is relatively stable except for an acute disease exacerbation (such as asthma) that may require a shorter term intervention. Individuals in this category might receive regular follow-up for a limited period, including education and regular assessments to ensure medication adherence and engagement with their primary care provider. The focus for members in this category is finding the safest and most appropriate and cost-effective resolution. Care and support for these individuals may require higher-level clinician involvement and oversight for limited periods, but the sustained, longer-term interactions can be primarily supported with non-clinical staff.
Table 18.1 Intensive Care Management Versus Supportive Care Management
The key components of ICM that shape both Intensive Care Management and Supportive Care Management are described in more detail below. The primary driver for the ICM model revolves around the quick identification of high-risk members and their movement into Intensive Care Management.
ICM foundational care components
The Integrated Care Management model is designed around the following eight key components: Focusing on the Right Members; Right People, Right Skills; Individualized Relationship-Based Care; Bio-Psycho-Social Care Planning; Multi-disciplinary Case Rounds; Progression of Care; Outcomes Accountability; and Standardized Electronic Health Information Platform.
Focusing on the right members
ICM considers each member’s complete needs as they relate to their current and future health. Success in correctly aligning needs with the proper level of care is achieved by employing evidence-based member identification and stratification. Aetna uses predictive modeling and self-report tools to fully integrate physical and behavioral health conditions along with psychosocial risks and protective factors to identify members who would benefit from care management and also to properly stratify members into intensive and supportive levels of service.
While all members might benefit from participation in care management, a subset of the Medicaid population can benefit most from targeted, intensive care management activities. Aetna has developed a proprietary system to identify those members who are at highest risk for having poor health outcomes and who are the best candidates for intensive care management. Aetna’s proprietary predictive model is a specialized tool that harvests data from multiple sources, including claims data and medication profiles to predict utilization trends over a 12 month period. In addition to our standard predictive model, Aetna developed a companion risk-stratification model, the Consolidated Outreach and Risk Evaluation Analysis™ (CORE), that identifies those members who will most benefit from intensive care management services.
CORE is a powerful tool that groups members according to their risk of future health care utilization, as well as identifying members where the most impact can be made. CORE integrates the predictive model built primarily on cost of care with two other risk models that measure risk of inpatient and emergency department (ED) utilization. In addition, the tool identifies specific subsets of members that are at higher risk for ED utilization and inpatient admission. The CORE identifies the top 1% of individuals who have the highest cost, highest ED utilization, and highest inpatient utilization. This group also has the highest prevalence of mental illness and substance use disorders. The output of the monthly CORE analysis regularly informs each health plan about which of their members is at highest risk over the next 12 months and whom should receive Intensive Care Management.
In addition to the CORE, each member is outreached and provided a general intake utilizing Aetna’s proprietary Health Risk Questionnaire (HRQ). The HRQ is designed to detect physical, behavioral, and psychosocial factors associated with significant health risks that can be influenced. The HRQ measures key indicators such as presence of a primary care practitioner or medical home, health literacy, medication adherence, alcohol or substance abuse, mental illness or cognitive impairment, housing stability, available support systems, mobility challenges, increased hospitalizations and health perception.
Once candidates are properly triaged, they are placed in the Intensive or Supportive Care Management track, or in Population Health. Each plan will also reconcile the identification of complex members with any contractually-obligated state mandates requiring care management. Members who are not identified as requiring Intensive Care Management through the above methods, but who are required to be care managed, are placed in Supportive Care Management until the screening can be completed.
Right people, right skills
Engaging complex members to achieve successful outcomes requires a qualified staff of clinical intensive care managers and non-clinicians that have the requisite knowledge, expertise, and skills. Under the ICM model, licensed independent clinicians, such as registered nurses and licensed clinical social workers, direct and lead the care plan and care coordination strategies for members. All staff on the ICM team receive education on specific principles and care strategies such as motivational interviewing and patient activation techniques, with special considerations for advanced disease and behavioral health care strategies.
Individuals in Intensive Care Management receive individualized care from a single intensive care manager that consists of primarily “high-touch,” sustained interventions. As previously discussed, a goal of ICM is to have one clinical team member coordinate all care management activities for a high-risk, complex individual for as long as necessary for the member to progress to the Population Health level. Caseloads for ICM care managers are envisioned to be smaller with an average of 30 to 70 members, but may vary based on each plan’s contractual requirement and expectations for outreach activities.
Additional staff support is provided by non-clinical staff who work in tandem with a clinical care manager to ensure all aspects of care coordination are covered. As members progress in their care and as a member becomes more proficient in self-management, the need for intensive clinical oversight will diminish. In this stabilization phase of care management, non-clinicians are in a better position to provide care coordination activities that will allow care managers to stay focused on practicing at the full scope of their license regarding important clinical matters.
Individualized relationship-based care
Member motivation and activation to change and manage their health can only come about through positive, supportive relationships. This requires a collaborative relationship between the member and their assigned care manager that continues throughout the duration of a member’s care management. The ICM model is centered on the expertise of two individuals – the member and the care manager. In the ICM system, each complex, high-risk member is assigned an intensive care manager who serves as the point person for coordinating all aspects of the member’s care management. While the intensive care manager is expected to have an on-going, highly interactive relationship with each assigned member, other members of the team may also assist with care management. For example, care management associates will assist with non-clinical activities, and other team members with additional subject matter expertise relevant to a particular member’s needs will collaborate with the assigned care manager to assure the member’s needs are met.
Additionally, the care management team supports the relationships of health care providers, human services providers, and community support systems important to the member’s recovery and resiliency. Ensuring the member has access to the range of resources they need, and coordination among those resources, are essential steps. This includes working with family and other care givers, engaging the member with a primary care provider in a medical home, and connecting them with essential social and housing supports that match their preferences and needs.
Bio-psycho-social care planning
Care planning that aligns the member’s highest priority issues with goals and interventions that make sense from the member’s perspective is critical to successful care management. Given that complex, high-risk members have multiple physical and behavioral health and psychosocial challenges, addressing these issues with a concise clinical assessment that concentrates on the full range of a member’s needs is the first step to understanding what is truly important to the member. The assessment process advances the dialogue to uncover areas of agreement that will set the foundation on how to address barriers that prevents the member’s effective management of their own health.
The ICM care planning process begins with the Care Plan Interview (CPI). The CPI provides a systemic method for evaluating all current and relevant aspects of a member’s care and support systems. The information obtained during the CPI gives rise to the care plan which is viewed as a dynamic “document” that is developed through reaching consensus with the member on goals and action items that are most significant for them. The care plan becomes a tool that is implemented under the guidance of a skilled care manager who is continually tracking and revising the plan to reflect goal attainment or when necessary, to re-align goals that reinforce changes in the member’s individual needs, abilities, and desires. The care plan creates the central touch point from which the care manager can base coaching and mentoring strategies, as well as guiding the member toward self-reliance.
The care planning process, however, is not restricted to only the care manager and the member. The care plan is a centralized tool with shared access by all providers of care or services with a mutual commitment to positively impact the member. The care planning process identifies the member’s strengths and critical barriers to drive a care plan that is actionable and effective. The care plan identifies all the critical people who are responsible for specific activities intended to help the member achieve their goals. Finally, the care plan enables the care manager and member to track and trend progress toward the member’s goals by focusing on long-term outcomes to assure the benefits are sustained into the future.
Multi-disciplinary case rounds
In order to promote effective care management, each health plan engages in frequent multi-disciplinary case rounds that allow for the intensive examination of individual cases and discussion of evidence-based care management strategies. Multi-disciplinary case rounds offer the opportunity to leverage the collective strengths of the medical management team to produce the best possible outcomes for members. Regular case rounds serve many functions by encouraging a plan’s clinical leadership to provide staff supervision, coaching and mentoring opportunities, and ensuring sound clinical judgment.
Other important aspects of case rounds include the following: each plan is encouraged to have, at minimum, bi-weekly case rounds; case rounds concentrate on care management strategies, recommendations, and strategic problem-solving; risk identification and risk mitigation are emphasized as part of a comprehensive review; collaboration with other health plans to exchange ideas and examine emerging best practices; and all care managers are expected to present cases on a regular basis highlighting successes, lessons learned, and challenges that require consultation.
Progression of care
Successful care management ensures that members are receiving the requisite level of care required to help them achieve optimal health and self-management. It is critical to match the intensity of care management services to the member’s needs as the member moves through recovery toward self-management and autonomy. Throughout the care management process care managers must adapt the intensity of care management to the member’s willingness and ability to effectively use that intensity of service. Achieving positive results will only take place when the members take greater accountability over their own health care needs, with the intensity of care management services they receive decreasing and responsibility shifting to each member, accordingly.
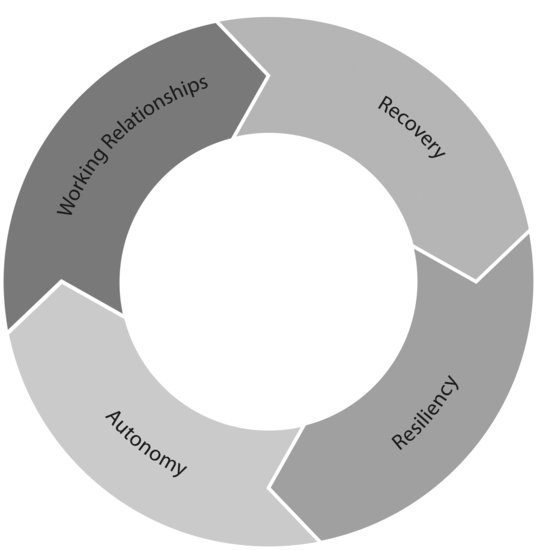
Complex, high-risk members should be viewed as moving through four “phases” of care management:
- Working Relationship – The member is engaged in an effective working relationship with a primary care manager.
- Recovery – The member shows a sustained decrease in their current, avoidable utilization and problematic symptoms, as well as sustained progression towards optimal quality of life and reduction/moderation of risk factors.
- Resiliency – The member decreases their risk of future utilization by decreasing current risk factors and enhancing current protective factors.
- Autonomy – The member takes responsibility for their own health and well-being, which includes managing their own health conditions effectively.
Figure 18.2 Autonomy Wheel Diagram
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


