Chapter 31 Supporting the breastfeeding mother
Learning outcomes for this chapter are:
1. To identify the location and structures of the female breast
2. To explain the function at a cellular level of the lactating breast
3. To differentiate between mammogenesis, lactogenesis and galactopoesis
4. To identify the properties and discuss the benefits of human breast milk
5. To discuss worldwide initiatives that promote breastfeeding and identify the 10 steps to successful breastfeeding
6. To describe recommended practices that assist in the preparation, initiation and maintenance of breastfeeding
7. To recognise the importance of positioning and attachment of an infant at the breast
8. To identify common challenges associated with breastfeeding, and describe recommended interventions and treatments for each identified challenge
9. To critically analyse artificial feeding in relation to breastfeeding.
The chapter establishes an evidence-based framework for understanding, educating and assisting women and their families with breastfeeding. The discussion draws on research to identify benefits of breastfeeding practices and provide guidelines for midwives when working with women who are preparing, initiating and maintaining breastfeeding. Challenges that may arise during breastfeeding are addressed, and evidence-based strategies for their management are discussed. Positioning and attachment are emphasised as crucial to milk production, supply and successful transfer from mother to infant. A critique of artificial feeding is presented against a background of the advantages of breast milk and breastfeeding.
BREAST STRUCTURE AND FUNCTION
Breast structure
The mature female breast is located over the pectoralis major muscle on the anterior chest wall, within the superficial fascia, extending from the 2nd to the 6th rib and from the sternum to the axilla on each side (Stables & Rankin 2005); it is composed of glandular tissue with a branching duct structure surrounded by supportive connective and adipose tissue. Breast size, colour and shape vary from breast to breast and from woman to woman. Breast size is dependent on the amount of adipose tissue present—size is a poor indicator of breast function and breastfeeding success (Riordan & Wambach 2009).
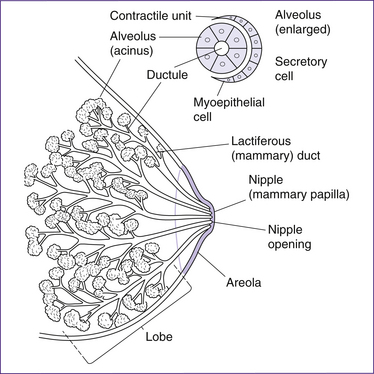
In the mature woman, each breast has 7–10 sections or lobes of glandular tissue separated by connective tissue. The gland epithelial tissue (secretory or acini cells) synthesises the breast milk, which is then stored in small clusters of sac-like spaces called alveoli. Some 10–100 clusters of secretory alveoli cells are present in each lobe, supported by collagen sheaths (Stables & Rankin 2005). Myoepithelial (muscle) cells and capillaries surround the clusters of alveoli. The breast milk passes with the aid of muscle contractions from the alveoli into small and then larger ducts as they get closer to the nipple. Several milk ducts merge close to the areola before the nipple is reached. Some 5–10 small channels or pores emerge through the nipple to the skin surface (Brodribb 2004). A diagram of the breast structure is shown in Figure 31.1.
Ultrasound studies of the lactating breast have enabled the female breast structure and function to be more clearly visualised (Ramsay et al 2005). This research has challenged the once-familiar, well-accepted and longstanding diagrams depicted in textbooks. Visualisations have indicated:
• fewer lobes (7–10, not 15–20)
• an absence of milk sinuses (reservoirs) behind the nipple and areola
• fewer openings of milk ducts at the nipple (5–10, not 15–25)
• smaller number and size of the small and larger ducts
• rapid branching of ducts close to the areola, which continue to branch and intertwine into a disorderly pattern; the assumption that there is an organised pattern of branching ducts is now obsolete
• that the milk duct diameter increases as let-down (milk ejection) occurs
These studies suggest that the ducts transport rather than store breast milk (Geddes 2007).
The nipple is located in the middle of the brown pigmented area called the areola. The size and shape of both nipple and areola can vary between individuals, from large and with flat nipples and reduced or no pigmentation, to raised and small nipples with very distinctive pigmentation. Women can lactate successfully regardless of these wide variations. The nipple, which is composed of smooth muscle, becomes erect when stimulated. There are small swellings located on the areola that secrete an oily fluid which provides lubrication and antimicrobial protection for the nipple and areola surface; these are called Montgomery’s tubercles. The nipple and areola also contain many nerve endings that respond to the infant’s sucking at the breast and trigger the production and release of milk (Blackburn 2003).
The breast is highly vascularised via the internal mammary and lateral thoracic arteries. Arterial blood terminates in capillary networks surrounding the alveoli. Venules drain venous blood into a circular vein behind the nipple, then into the mammary and axillary veins (Stables & Rankin 2005). The lymph vessels are extensive, flowing alongside the ductal tissue and converging towards the nipple, where they form a plexus beneath the areola. Lymph glands drain into axillary nodes. The breast is innervated by the 4th, 5th and 6th intercostals, giving rise to an uneven pattern of sensation, with the areola and nipple being the most sensitive part (Riordan & Wambach 2009).
Breast function
The function of the breast is to synthesise and eject milk—a process called lactation. The components of milk are synthesised in the secretory cells (protein, fat and lactose) of the alveoli or extracted from the maternal plasma (minerals and vitamins) (Blackburn 2003). The secretory cells alternate between a secreting and a resting state. During infant sucking, active secretion occurs.
Breast milk production involves integration of neuronal, endocrine and autocrine processes. There are several main phases involved as breast gland tissue develops and the ability to produce milk occurs over time (Wilson-Clay & Hoover 2008).
Mammogenesis (mammary growth)
Mammary growth (mammogenesis) begins during embryonic and fetal life and accelerates at puberty under the influence of oestrogen and progesterone (Stables & Rankin 2005). Further changes occur during pregnancy and after birth, in order to support lactation. Maturation of tissue begins shortly after conception, when there is a steady increase in breast size and weight, with a proliferation of the ducts and alveoli. Nipples become more erect, the areola pigmentation enhances and the Montgomery’s tubercles enlarge. Blood supply to the breast also increases, making the vessels appear more visible on the skin surface (Riordan & Wambach 2009). These changes occur under the influence of oestrogen, human placental lactogen, glucocorticoids, human chorionic gonadotrophin, insulin, growth hormone, thyroid hormone, progesterone and prolactin.
Lactogenesis (initiation of milk secretion/production)
During the second half of pregnancy, the secretory cells begin milk synthesis (lactogenesis I) under the influence of prolactin and placental lactogen, and colostrum and fat globules distend the alveoli (Blackburn 2003). Following childbirth, progesterone, placental lactogen and oestrogen diminish in the bloodstream. This fall triggers colostrum to change to more mature milk. At about day 2–3 up until day 8 post-birth, milk production is influenced by the hormones prolactin, placental lactogen, cortisol and insulin.
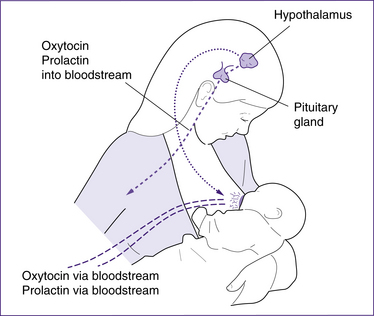
When the infant sucks at the breast, mechanoreceptors (nerve endings) in the nipple stimulate the hypothalamus to suppress the prolactin-inhibiting factor and release prolactin and placental lactogen from the anterior pituitary into the bloodstream. This initiates milk production (lactogenesis II) by the acini cells in the glandular tissue at about 30–40 hours postpartum (Hurst 2007). Increase in sucking and emptying the breasts leads to an increase in prolactin levels, and the prolactin receptors and milk supply increase. The breast function moves from being under initial endocrine or hormone control to autocrine or milk removal control (Riordan & Wambach 2009).
The let-down (milk ejection) reflex
The let-down reflex (or milk ejection reflex) is an important process for moving milk along the system of ducts in the breast and is essential for milk removal and transfer to the infant. Sucking at the breast sends messages from the nipple/areola area to the hypothalamus, which in turn releases oxytocin from the posterior pituitary gland into the bloodstream (see Fig 31.2). Myoepithelial cells around the alveoli are then stimulated to contract and push milk down the ducts towards the nipple. This same hormone stimulates uterine contractions and involution (Riordan & Wambach 2009). The milk ducts increase in diameter during let-down. Multiple let-downs can occur during a breastfeed and affect the amount of milk the infant consumes (Kent et al 2006; Ramsay et al 2004).
The let-down reflex can also be stimulated by the sight of an infant or the sound of an infant’s cry, and inhibited by maternal pain or stress, or low milk supply. Some mothers do not notice any change in sensation during let-down but others report signs of increased thirst, a tingling sensation in the breast, a feeling of breast fullness, leaking of milk from the non-suckled breast or uterine contractions (Brodribb 2004). During let-down, the infant’s sucking and swallowing pattern may change from a fast suck to a slower suck and swallow of larger amounts of breast milk.
Galactopoesis (maintenance of milk secretion)
The maintenance of milk production (galactopoesis—also known as lactogenesis III) depends on active removal or non-removal of milk from the breast on a frequent basis from about day 9 post-birth until breastfeeding ceases (Hurst 2007). Breast function is now under the influence of a local feedback control mechanism. Production of milk depends on adequate stimulation of the breast—the more the infant sucks and the more milk is removed from the breast, the more milk is produced. The less sucking at the breast and the less milk removed, the less milk produced. As long as milk is removed from the breast regularly, the alveolar cells will continue to synthesise milk (Riordan & Wambach 2009).
The storage capacity also depends on the glandular tissue in the breast, not breast size. Storage capacity varies between mothers and between feeds for the same mother. Breastfeeding frequency is related to breast storage—the lower the storage, the higher the frequency of feeding and vice versa. Furthermore, the storage capacity of each breast and the quantity of milk removed at each feed influences milk synthesis between feeds (Ramsay et al 2004). The milk supply is therefore produced and influenced through the supply–demand principle as well as the functional capacity of the breast. Infants therefore regulate their milk intake according to their appetite.
Weaning (involution)
If breastfeeding ceases or reduces in frequency, peptides in the milk begin to inhibit cell production and cells die, and therefore milk production decreases. This reduction or weaning may be infant-led or mother-led. When breastfeeding ceases, involution of breast tissue occurs to the pre-pregnant state. Weaning milk begins to resemble the composition of colostrum, again with an increase in immunoglobulins, protein and sodium and a decrease in lactose (Lawrence & Lawrence 2005).
Benefits of breastfeeding
Although instinctively known, research has clearly established the benefits of breastfeeding and the use of human milk for infants. Concomitantly, mothers, families and society can benefit from an increase in the incidence and prevalence of breastfeeding. These benefits include physiological, nutritional, health, psychological, social, economic and environmental outcomes (Lutter 2000; Oddy 2001; WHO 2000).
Biologically breast milk is the ideal food for infants. Breast milk provides a unique fomulary of proteins, carbohydrates and fats needed for optimal cell function and growth. The breast alters the consistency of these nutrients as the infant’s growth and development change over time. This balance, complexity and enhanced bioavailability of nutrients and other substances in breast milk has recently been recognised (Brodribb 2004).
• gastrointestinal infections (Kramer & Kakuma 2004; Oddy 2008)
• diarrhoeal illness (Bertran et al 2001; Sikorski et al 2004)
• necrotising enterocolitis (Updegrove 2004))
• urinary tract infections (Bick 1999)
• protects infants from sudden infant death syndrome (SIDS) or sudden unexpected infant death (SUDI) (McVea et al 2000)
• reduces the risk of childhood asthma (Oddy 2008)
• reduces the risk of eczema in childhood (Kramer et al 2001b)
• significantly enhances cell-mediated and humoral responses to antigens (Campbell 2000)
• provides immunological protection from insulin-dependent diabetes mellitus (Bick 1999), Crohn’s disease and ulcerative colitis, childhood lymphomas and those of allergic origin (Bener et al 2001; Saarinen et al 2000).
Breastfed infants are less likely to develop obesity (Armstrong & Reilly 2002) and have lower cholesterol levels in later life (Owen et al 2002; Singhal et al 2004). Human milk, containing vital omega-3 and omega-6 fatty acids needed for brain development, also enhances cognitive development (Kramer et al 2008) and visual acuity (Mortensen et al 2002; Odent 2003).
Mothers are also likely to benefit from breastfeeding. Oxytocin, released during infant suckling at the breast, contracts the uterus and hastens involution (Riordan & Wambach 2009). Breastfeeding also prolongs lactation amenorrhoea, thus reducing fertility and increasing child spacing (Kramer & Kakuma 2004). A reduction in rates of ovarian and breast cancer (Zheng et al 2000), heart disease (Owen et al 2002; Singhal et al 2001) and osteoporosis (Jones et al 2000) is revealed in mothers who breastfeed. Prolonged breastfeeding also improves the return to pre-pregnant weight. Psychologically, maternal–infant bonding and empowerment is enhanced by breastfeeding, due to early contact; and maternal oxytocin levels released during a breastfeed decrease maternal anxiety and enhance calmness and social responsiveness (Day 2006; Lawrence & Lawrence 2005).
An increase in the prevalence of breastfeeding may provide overall medical, social and economic benefits to society. This impact may flow through to improved personal health outcomes and the possibility of healthier communities through reduced perinatal morbidity and mortality; cost savings for parents (no need to purchase infant formula articles); fewer hospital admissions; lower healthcare costs; and less absenteeism from school or work attributable to illness (Ball & Bennett 2001; NICE 2006). Further, global enhancements have been suggested related to reduction in world overpopulation (reduced fertility), saving on fuel and energy resources, and elimination of wastes from the production of artificial milk and its leftover containers (Biancuzzo 1999).
There is significant good-quality clinical and public health evidence to support the benefits of breastfeeding and human milk consumption (Oddy 2008). Therefore the World Health Organization (WHO 2003) recommends that all babies be exclusively breastfed for the first six months to promote health and reduce illness. The WHO also recommends continued breastfeeding for a further two years. See Table 31.1 for a summary of the benefits of breastfeeding for mother and infant.
Table 31.1 Summary of the benefits of breastfeeding for mother and infant
IDDM = insulin-dependent diabetes mellitus; NEC = necrotising enterocolitis; SIDS = sudden infant death syndrome; SUDI = sudden unexpected infant death.
(Source: WHO 2001)
Properties of breast milk
Colostrum: the early milk
Colostrum is secreted during the last trimester of pregnancy until 10 days postpartum. It is a viscous, concentrated yellow, white or brown liquid of low volume (varies from 7 mL to 123 mL in 24–48 hours) with an average amount of 37 mL (Riordan & Wambach 2009). The newborn’s kidneys are immature at birth and cannot deal with large volumes of fluid, and therefore a low volume of colostrum is ideal. This early fluid is high in protein, sodium and minerals but low in carbohydrates, fats and vitamins. Colostrum facilitates the growth of gut flora, and aids the excretion of meconium from the gut due to its laxative effect (Brodribb 2004). Colostrum also contains a high concentration of antibodies and immune cells that protect a newborn’s fragile mucuos membranes against microbes and viruses by preventing their entry, transport and/or proliferation (Odent 2003). The milk volumes increase rapidly 3–4 days postpartum (Wilson-Clay & Hoover 2008). Colostrum is therefore the ideal first food for the newborn with its low volume (to protect the kidneys), balanced nutrients for growth and antibodies for protection at this vulnerable time.
Mature breast milk
Mature breast milk is a rich, balanced brew containing 90% water and 10% solids. Bluish in colour, it is slightly alkaline (pH 7.0–7.45), with an average calorie count of 65 kcal/100 mL (272 kJ/100 mL), although this varies depending on fat content. It is not a uniform fluid; it varies from mother to mother and changes composition during a feed, with the time of the day and from one lactation to the next (Blackburn 2003). Breast milk has nutritional, anti-infective, immunological, bioactive and anti-allergenic properties.
Nutritional properties
The constituents of breast milk include the following:
• Fats—fat provides half the calories of an infant’s energy needs. Fats are essential for development of visual acuity, help vitamin function and form cell membranes and prostaglandins (Lauwers & Shinskie 2004). Levels vary during the feed and are higher in hindmilk than foremilk. Fat globules are small and easily absorbed, with triglycerides being broken down to free fatty acids and glycerol (Blackburn 2003).
• Carbohydrates—the carbohydrate contained in human milk is mostly lactose, being broken down slowly to glucose and galactose and providing 40%–45% of an infant’s energy needs. Carbohydrates enhance calcium absorption, promote the growth of lactobacilli in the intestines and reduce the growth of gut pathogens. They are also essential for central nervous system development (Lauwers & Shinskie 2004).
• Protein—human milk protein contains 40% casein (soft curds) and 60% whey (a soluble liquid), and is therefore easily digested and absorbed. The whey contains albumins, enzymes, immunoglobulins and hormones (Blackburn 2003). Infants are able to use the protein constituent efficiently. Proteins are needed for cell growth and stability, all body processes, bile salt conjugation and nerve transmission (Lauwers & Shinskie 2004).
• Vitamins—fat-soluble and water-soluble essential vitamins are available in breast milk in sufficient amounts to aid cell growth and function. Specifically, vitamins are required for blood clotting, central nervous system development and skin integrity, and to protect the retinas and mediate cell function (Riordan & Wambach 2009).
• Minerals—human milk contains all the essential minerals needed for electrolyte balance, and infant cell and organ function. They are highly bioavailable and suited to infant growth and development (Brodribb 2004).
• Water—water is the largest component (90%) of breast milk in which dissolved solids (10%) are carried. Water also contributes to regulation of an infant’s temperature.
Other properties of breast milk
• Anti-infective properties—enzymes, immunoglobulin and leucocytes provide protection from infection and reduce the incidence and severity of acute and chronic illnesses (Bick 1999).
• Immunological properties—immunoglobulins are proteins produced by the plasma that block adhesion of pathogens to the infant’s mucosal surfaces and produce antibodies, which in turn target microbes. B-lymphocytes help destroy antigens; macrophages engulf and absorb pathogens; neutrophils ingest microbes; and T-lymphocytes kill infected cells. Lactoferrin binds iron (preventing pathogens from using it) and aids T and B cell production. The bifidus factor is an intestinal flora that promotes the growth of lactobacilli and maintains the gut pH at an acid level, which inhibits the growth of Escherichia coli. Lactoperoxidase is an enzyme that, when combined with ImmunoglobulinA, increases the ability to kill streptococcus bacteria. Oligosaccharides are simple chains of sugars that intercept bacteria and block their attachment to the gut epithelium and bind to form harmless substances (Lawrence & Lawrence 2005; Lauwers & Shinskie 2004; Odent 2003).
• Bioactive properties—enzymes, lysosomes, lipase, amylase, interferon and fibronectin in breast milk promote growth and development, and infection control (Riordan & Wambach 2009).
• Anti-allergenic properties—breast milk facilitates early maturation of the intestinal mucosa and reduces allergic responses. There is a protective effect against skin conditions and respiratory illnesses (Bertran et al 2001; Saarinen et al 2000).
Hormones and enzymes
Over 70 enzymes have been isolated from human breast milk. An insulin-like factor promotes growth, an epidermal factor aids skin growth, cortisol transports fluids and salts in the gut, thyroxine stimulates the intestine, prostaglandins aid local circulation and mucus secretion, electrolytes balance and protect the gut mucosa, and taurine is a neurotransmitter that aids brain maturation (Riordan & Wambach 2009).
WORLDWIDE INITIATIVES TO PROMOTE BREASTFEEDING
World Health Organization
The World Health Organization (WHO) is a specialised agency of the United Nations with a primary responsibility for public health. Its brief extends to the role of maternity services in promoting breastfeeding (Biancuzzo 1999). A joint WHO/United Nations International Children’s Emergency Fund (UNICEF) statement, launched in 1989, describes the critical role of healthcare services and outlines steps taken to facilitate the initiation and establishment of breastfeeding (WHO/UNICEF 1989).
The WHO Global Data Bank on breastfeeding developed new breastfeeding indicators and definitions to broaden the nomenclature for describing breastfeeding behaviour and to increase the coherence, reliability and comparability of data. The ‘Bank’ pools information drawn from surveys and studies dealing with breastfeeding prevalence and duration. This enables comparison of representative data. National, regional and local information gathered on breastfeeding and complementary feeding practices over time provides a reliable database with which to plan promotional programs (WHO 1996).
The WHO Code
An initiative of the WHO and UNICEF, the International Code of Marketing of Breastmilk Substitutes (the WHO Code), adopted in 1981, emphasises the fact that human milk and breastfeeding provides an unequalled way of providing nutrients and other biological substances necessary for the growth and development of infants. It aims to protect the wellbeing of infants through the protection and promotion of breastfeeding and ensuring that breast milk substitutes are used only when necessary. Support for and adherence to the WHO Code is an ethical choice for countries, governments, industries, healthcare professional organisations, educators and individuals involved in maternity and newborn care (Young 2001).
The Innocenti Declaration
In 1990 the WHO, UNICEF and other key health and global policy-makers met in Innocenti, Italy to set targets for promotion and support of breastfeeding. The Innocenti Declaration was produced and adopted, recognising the uniqueness of breastfeeding, the need to reinforce a breastfeeding culture and to stop the competition of a bottle-feeding culture. The Declaration stated that all women should be enabled to practise exclusive breastfeeding for six months following childbirth. It recommended that all governments implement the WHO Code and develop national breastfeeding targets and policies, and integrate them into overall health and development (WHO 2003).
In response to the recommendations, the National Health and Medical Research Council (NHMRC) in Australia developed guidelines for health workers on infant feeding (Commonwealth Department of Health and Family Services 2001). A national breastfeeding strategy was launched in the same year to provide a multifaceted primary healthcare approach to breastfeeding promotion. This was aimed at healthcare professionals, community agencies and the general public (Commonwealth Department of Health and Aged Care 2001). Similar measures were also implemented by the New Zealand government (Ministry of Health 2009).
International Baby Food Action Network
Growing public and professional concern over commercial and advertising promotion of breast milk substitute foods, feeding bottles and teats encouraged development of the International Baby Food Action Network (IBFAN) (IBFAN 1993). The network is a coalition of voluntary organisations in industrialised and developing countries working for better health through the promotion of breastfeeding and the elimination of the marketing of artificial infant foods. The IBFAN provides a written guide for healthcare workers about the WHO Code (WHO 1993) and also monitors Code compliance. Code-breaking promotional materials and tactics are still used in systematic and blatant ways by companies that continue to undermine health in pursuit of profits (Advisory Panel on the Marketing in Australia of Infant Formula 2000).
World Alliance for Breastfeeding Action
In 1990 the United Nations held a world summit for children, at which heads of state promised to work towards the rights of children, including the right to be breastfed. In 1991 groups working on maternal and child health launched the World Alliance for Breastfeeding Action (WABA) group. IBFAN was one founding member. The WABA group mobilised social support for the Innocenti Declaration and implemented international breastfeeding week activities on an annual basis (IBFAN 1993).
Baby Friendly Health Initiative
Ten steps to successful breastfeeding have been articulated to encompass education and counselling of new mothers, unrestricted mother–infant contact, demand and exclusive breastfeeding and maternal support in the postpartum period. Healthcare services are challenged and motivated to adhere to these 10 steps when working with mothers and their families. The BFHI aims to increase the worldwide prevalence and duration of breastfeeding (Braun et al 2003; Naylor 2001). The BFHI philosophy is applied universally irrespective of whether a country is developed or developing, or has a Western or traditional society (WHO/UNICEF 1992).
In 2006, in Australia, the initiative’s name changed to the Baby Friendly Health Initiative in order to more accurately reflect the work of both hospital and community settings (Australian College of Midwives 2008).
Similarly, the New Zealand Breastfeeding Authority has also developed a Baby Friendly Community Initiative (BFCI) in recognition of the importance of continuing community support for breastfeeding women (New Zealand Breastfeeding Authority 2009).
THE 10 STEPS TO SUCCESSFUL BREASTFEEDING
Healthcare practices are very influential when a new mother and her family are initiating and establishing breastfeeding. Consistent lactation support and encouragement by informed healthcare workers, the reduced influence of artificial feeding practices, keeping mother and infant together and feeding early and frequently by infant-led demand are practices promoted by the BFHI. Successful long-term breastfeeding depends on a successful beginning (Philipp & Merewood 2004). Through compliance with the 10 steps to successful breastfeeding, healthcare agencies give mothers the best chance of establishing and maintaining breastfeeding. The 10 steps are listed in Box 31.1.
Box 31.1 The 10 steps to successful breastfeeding
Every facility providing maternity services and care for newborn infants should:
1. Have a written policy that is routinely communicated to all healthcare staff.
2. Train all healthcare staff in the skills necessary to implement this policy.
3. Inform all pregnant women about the benefits and management of breastfeeding.
4. Help mothers initiate breastfeeding within an hour of birth.∗∗
5. Show mothers how to breastfeed, and how to maintain lactation even if they are separated from their infants.
6. Give newborn infants no food or drink other than breast milk, unless medically indicated.
7. Practise rooming-in—allow mothers and infants to remain together—24 hours a day.
8. Encourage breastfeeding on demand.
9. Give no artificial teats or pacifiers (also called dummies or soothers) to breastfeeding infants.
10. Foster the establishment of breastfeeding support groups and refer mothers to them on discharge from hospital.
(Source: WHO/UNICEF 1989)
A prospective study by Pincombe et al (2008) investigated the relationship between 6 of the 10 steps and duration of breastfeeding in first-time mothers. The study found babies who were not exclusively breastfed and used a pacifier or nipple shield were at risk of weaning early.
PREPARATION FOR BREASTFEEDING
Breastfeeding education
Successful breastfeeding depends on the mother’s acquisition of basic skills and accurate information. This success is strongly influenced by the quality of help and support (both professional and community) provided during pregnancy, childbirth and the postpartum period (Sikorski et al 2004). Despite the evidence of the benefits of breastfeeding, many women may choose to use artificial formula, indicating that their decision not to breastfeed may be unrelated to health factors (Earle 2000; Hodinott & Pill 2000).
The maternal decision to breastfeed is based on multiple factors, including knowledge about breastfeeding, personal attitudes and beliefs about breastfeeding, role models and the support of significant others (Baghurst et al 2006; Hurst 2007
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree