The person with acute left ventricular failure following myocardial infarction
CASE AIMS
After examining this case study the reader should be able to:
• Outline how the heart normally works as a pump.
• Briefly explain why a patient who has had an anterior MI could have left ventricular failure.
• Outline left ventricular ejection fraction and its significance.
• Demonstrate an understanding of the mode of action and contraindications of cardiac nitrates.
• Demonstrate an understanding of the mode of action and the benefits of giving frusemide in left ventricular failure.
• Demonstrate an understanding of the mode of action and significance of using opiates in left ventricular failure.
• Discuss the role of the nurse in anticipating the side-effects of using opiates in left ventricular failure.
CASE
Mr D is a 70-year-old man who was admitted to the coronary care unit (CCU) with acute shortness of breath, chest pain, nausea and vomiting. He was diagnosed, with his current history and significant ECG changes, with an acute anterior myocardial infarction (AMI). Previous medical history is of hypertension and angina, and he is a current smoker. He was thrombolyzed according to the CCU protocol for thrombolysis, and appeared to respond well to treatment. Later an echocardiogram was performed which showed he had a poor left ventricular ejection fraction (LVEF) of 40% which showed as left ventricular systolic dysfunction (LVSD) by non-contracting (akinetic) or poorly contracting (hypokinetic) areas of the left ventricular wall.
1 Prior to Mr D’s acute AMI, how would his heart have worked as a pump?
2 Why has Mr D gone into LVEF following his AMI?
3 What is an LVEF?
4 What is the significance of determining LVEF following an echocardiogram and potential future events?
Twenty-four hours post-lysis Mr D developed sudden breathlessness (dyspnoea), tachycardia and confusion, and appeared pale, cold and clammy. His saturations on air were recorded as <80%, blood pressure 126/85mmHg, pulse 120bpm, respirations 25 breaths per minute. He was diagnosed with acute pulmonary oedema with crepitations as a consequence of left ventricular failure upon completion of examination and a portable chest X-ray. He was treated with IV nitrates for the pulmonary oedema, IV frusemide for his left ventricular failure and IV diamorphine.
5 Describe the mode of action of IV nitrates
6 Explain the contraindications of giving IV nitrates to a person with acute left ventricular failure
7 What is the mode of action of frusemide?
8 What are the benefits of giving IV frusemide in left ventricular failure?
9 What are opioids?
10 What is the significance of using IV diamorphine in acute left ventricular failure?
11 What likely side-effects should the nurse anticipate?
ANSWERS
1 Prior to Mr D’s acute AMI, how would his heart have worked as a pump?
A Normal cardiac output (CO) is the product of heart rate (HR) and stroke volume (SV). HR is determined by the rate of spontaneous firing at the sinoatrial node but can be modified by the autonomic nervous system. The vagus nerve acts on muscarinic receptors to slow the heart, whereas the cardiac sympathetic fibres stimulate beta adrenergic receptors and increase HR. Stroke volume is determined by three main factors:
• preload;
• afterload;
• contractility.
PRELOAD
Preload is the stretching of the muscle fibres in the ventricles (both right and left). This stretching results from blood volume in the ventricles at end diastole (the relaxation filling period of the cardiac cycle). According to Starling’s Law, the more the heart muscle stretches during diastole, the more forcefully it contracts during systole (the contraction phase of the cardiac cycle). Think of preload as being like a balloon stretching as air is blown into it – the more air blown into the balloon the greater the stretch.
AFTERLOAD
This is the resistance to ventricular ejection and is caused by resistance to flow in the systemic circulation, referred to as systemic vascular resistance. This is determined by the diameter of the arterioles and pre-capillary sphincters – the narrower or more constricted, the higher the resistance. The level of systemic vascular resistance is controlled by the sympathetic system which, in turn, controls the tone of the muscle in the wall of the arterioles, and hence the diameter.
CONTRACTILITY
Contractility refers to the inherent ability of the myocardium to contract normally. Contractility is the amount of stretch present in the myocardium muscle fibres at the end of diastole. This is also influenced by preload. So in effect if returned blood flow to the right side of the heart is compromised in any way then ultimately this will have an effect on the amount of blood returning to the left side of the heart. This can affect afterload (Barrett et al. 2009).
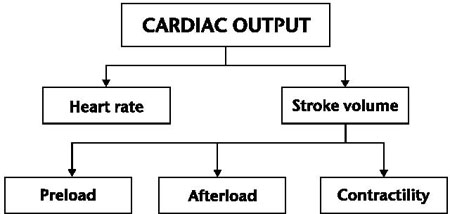
Figure 6.1 Factors affecting cardiac output
BLOOD PRESSURE AND CARDIAC OUTPUT
Blood leaving the left side of the heart (systemic system) is at a greater pressure than blood returning to the right side. This is because the left side of the heart is responsible for delivering oxygenated blood via the aorta into the body and ultimately perfusing all the cells of the body with nutrients and oxygen (a mean arterial pressure of 90–100mmHg is initiated from the left ventricle on systole).
The left ventricle has a thicker myocardium (muscle wall) and consequently has the largest coronary artery that feeds this muscular wall (left ascending coronary artery). The right ventricle has a thinner myocardium and the right side of the heart (pulmonary) is the smaller of the two chambers and functions at a much lower pressure than the left (mean arterial pressure of 12mmHg). This lower pulmonary pressure allows blood to move through the lungs more slowly which is vitally important for gaseous exchange.
As the heart is a closed system it needs to function effectively and requires that both sides pump the same amount of blood over time. If the output of the left heart ventricle were to fall below that of the right, blood would accumulate in the pulmonary circulation. Likewise if the right side were to pump less efficiently than the left then blood would accumulate in the systemic system (Porth 2011).
2 Why has Mr D gone into LVEF following his AMI?
A Mr D has been diagnosed and treated for an AMI. Any occlusion of the anterior descending branch of the left coronary artery can lead to an anterior wall infarction (death of muscle tissue). This occurs if the heart muscle is starved of rich oxygenated blood and as a result the portion of the muscle that has been occluded dies (necrosis). This is affecting Mr D’s heart’s pumping ability.
Because the left ventricle has the largest coronary blood supply, it is the most likely to be involved in MI. Any damage to the left ventricular myocardium through infarction leads to reduced contractility and abnormal movements of the walls of the ventricle (akinetic and hypokinetic contraction); this has had a greater significance as Mr D also has a history of hypertension.
The result is reduced cardiac output or a need for the ventricle to increase its workload to maintain the same cardiac output. This in turn can lead to an increase in muscle bulk (hypertrophy) or an enlargement of the chamber itself (dilation). These physical changes are known as ‘remodelling’ and although they are a compensatory mechanism the result can be a negative effect as the ventricle becomes overstretched and the fibres lose their elasticity. Further, a dilated heart can also change the shape of the atrioventricular valves, which can in turn lead to regurgitation (Nicholson 2007).
Left-sided heart failure associated with elevated pulmonary venous pressure and decreased cardiac output explain Mr D’s situation – he is presenting with breathlessness, weakness, pulmonary congestion and associated confusion (Woods et al. 2010).
3 What is an LVEF?
A As Mr D has a diagnosis of left ventricular systolic dysfunction (LVSD) the pumping action of his heart is reduced, weakened and/or compromised. This can be quite common following an AMI. A common clinical measurement of the left ventricle, via an echocardiogram, is LVEF.
• The LVEF is a calculation of how much blood is ejected out of the left ventricle (stroke volume), divided by the maximum volume remaining in the left ventricle at the end of diastole (when the heart relaxes).
• A normal LVEF in a healthy person is around 55–75%. Left ventricular systolic heart failure shows as a decreased fraction of <50%.
• Mr D has been diagnosed as having an LVEF of 40%. At anything less than 50% his heart can start to have serious problems with its pumping ability, as a direct consequence of his MI (NICE 2010).
Table 6.1 Ejection fraction measurements
| Ejection fraction measurement | What it means |
| 55–70% | Normal |
| 40–55% | Below normal |
| Less than 40% | May confirm diagnosis of heart failure |
| <35% | Patient may be at risk of life-threatening irregular heartbeat |
4 What is the significance of determining LVEF following an echocardiogram and potential future events?
A The significance of establishing ejection fraction is that it estimates the percentage of blood pumped out of the heart each time it contracts. When the heart contracts it ejects blood from the left and right ventricles, and as it relaxes the ventricles refill with blood.
As we have already established, the left ventricle is the heart’s main pumping chamber and, as such, ejection fraction is usually only measured in the left ventricle, as it is responsible for sending oxygenated blood via the aorta into the systemic system. A damaged left ventricle has a direct effect on cardiac output, which it compromises (i.e. makes low). This can lead to hypoperfusion of the body’s tissues. It also has an effect on the lungs, with an increased pressure in the pulmonary veins. The rise in pressure is due to more and more blood being pumped to the left side of the heart to compensate for its reduced efficiency. The left and right side of the heart must pump the same volume of blood. When this is not possible due to muscle damage, fluid is forced out of the blood vessels in the lungs and into lung tissue, leading to pulmonary oedema (Nicholson 2007).
5 Describe the mode of action of IV nitrates
A Nitrates (vasodilators) are recommended as an initial therapy, and are a common choice of drug used in the relief of angina and acute left ventricular failure; they also work by reducing breathlessness in patients with heart failure (BNF 2012). These drugs include isosorbide mononitrate and isosorbide dinitrate, which can be taken orally, sublingually (beneath the tongue) and by IV administration.
They exert their effects in a dose-dependent fashion by a mode of action which sees the release of nitric oxide (an important signalling chemical) into vascular smooth muscle and improves myocardial oxygen supply while reducing the demand of oxygen consumption. In small doses they dilate veins to a greater degree than arteries and this in turn affects preload (left ventricular end diastolic pressure) and right-sided heart filling pressure and volume (Thompson and Webster 2005). At higher doses nitrates can also act as arterial dilators, which lower peripheral resistance, left ventricular pressures, myocardial work and oxygen demands.
The final action of these drugs is that they dilate the coronary arteries, thereby increasing blood and oxygen supply to the myocardium (Nicholson 2007). For IV administration the starting dose should be low and increased gradually until relief of symptoms is achieved or blood pressure is adversely affected. As IV nitrates are vasodilators it is an important part of nursing care that blood pressure is monitored closely and that IV nitrates are adjusted accordingly. The systolic blood pressure should not drop by >20mmHg and if it does then the dose should be reduced if the systolic blood pressure is <100mmHg. A diastolic blood pressure of >60mmHg is necessary for adequate coronary artery perfusion.
Gardner et al. (2008) clarify that there is evidence that the combination of IV nitrates and frusemide is superior to high-dose diuretic treatment alone in the management of pulmonary oedema.
6 Explain the contraindications of giving IV nitrates to a person with acute left ventricular failure
A The contraindications of giving IV nitrates to a person with acute left ventricular failure are that they can cause hypotension (low blood pressure) as a consequence of vasodilation. The supply of blood to the heart is dependent on blood pressure remaining above a critical level; this means that a sufficient pressure to force blood into the coronary arteries is maintained. If it falls below the critical level the heart becomes short of oxygen and this can lead to chest pain. As a person ages a low blood pressure can reduce cerebral blood flow which can ultimately lead to impaired functioning of the brain and confusion (Jordan 2009).
7 What is the mode of action of frusemide?
A Frusemide belongs to a group of drugs called diuretics. Their mechanism of action is to work on the kidneys to increase urine volume by reducing salt and water reabsorption from the tubules (BNF 2012). There are several different sodium channels that exist in the renal tubules and, because of this, different diuretic drugs act at different sites along the tubule, providing different molecular actions and clinical side-effects (Dawson et al. 2005). Frusemide is a loop diuretic which acts at the thick ascending segment of the Loop of Henle, which eventually leads into the distal tubule.
Frusemide can cause the excretion of 15–25% of filtered sodium as opposed to the normal 1% or less. This action alone can result in profound diuresis (remember that where sodium goes, water will follow it). The mechanism of action of loop diuretics is that they inhibit the sodium/potassium/chloride co-transporter in the luminal membrane which inevitably increases the amount of sodium reaching the collecting duct. Because of this there is an increase in potassium and proton secretion. Loop diuretics have a venodilatory action which is renowned for bringing relief of clinical symptoms such as acute pulmonary oedema and heart failure in as little as 30 minutes by the IV route (NICE 2010).
8 What are the benefits of giving IV frusemide in left ventricular failure?
A The benefit of giving IV frusemide to a patient like Mr D with acute left ventricular failure is that if the patient is showing signs of fluid retention (pulmonary oedema) and is acutely unwell the dose of diuretic can be titrated up quickly to achieve the desired effect (DH 2000). Another benefit is that by removing excess water and by causing vasodilation, the pressure on the heart (preload) is inevitably reduced and consequently the heart is not put under as much strain. This can lead to a marked reduction in breathlessness (Nicholson 2007).
As with any drug there are always some side-effects and the main ones for frusemide are:
• hypotension;
• hypokalaemia;
• hyponatraemia;
• hypovolaemia;
• hyperuricaemia.
9 What are opioids?
A
• Opioids are drugs that are either naturally occurring (e.g. morphine) or chemically synthesized. They work by interacting with specific opioid receptors to produce the pharmacological effect of analgesia.
• They are also considered to be anxiolytic (reduce anxiety) and are likened to endorphins and encephalins, which are the body’s mood changers and analgesics in time of great stress.
• Sometimes, sedation, mental detachment or euphoria are the predominant effects of a dose of diamorphine (BNF 2012).
10 What is the significance of using IV diamorphine in acute left ventricular failure?
A As Mr D has gone into acute heart failure, the left ventricle fails and afterload increases. Pressure then rises in the left atrium and left ventricle, while hydrostatic pressure rises and fluid is forced out into the lung tissues, leading to pulmonary oedema. Opioids have a venodilatory effect, and because of this they can be used to reduce afterload. They also have the effect of making the patient feel calmer and dissociated from their body.
When a patient goes into acute MI like Mr D they appear very distressed due to their breathlessness, which can make them feel totally out of control. At this time their ‘fight and flight’ response becomes activated, which makes them feel worse. Administering IV diamorphine calms the patient, allowing time for the nitrates and diuretics to take effect (Nicholson 2007).
11 What likely side-effects should the nurse anticipate?
A Some of the adverse side effects of diamorphine include:
• drowsiness and sedation;
• reduction in sensitivity of the respiratory centre to CO2, which can lead to shallow and slow respirations and should be monitored carefully;
• hypotension and reduced cardiac output;
• activation of the vomiting centre due to stimulation of the chemoreceptor trigger zone (CTZ) – an antiemetic such as cyclizine should also be administered (Dawson et al. 2005).
KEY POINTS
• MI constitutes a mixture of symptoms and signs that are ultimately due to cardiac dysfunction.
• The heart’s pumping ability is reliant upon three factors: preload, contractility and afterload.
• Following an acute AMI the left ventricle can become severely damaged.
• LVEF is a common clinical measurement of the left ventricle, via an echocardiogram.
• Ejection fraction is normally around 55–75% in patients without cardiac damage.
• IV nitrates are a common choice of drugs used in the relief of angina and acute left ventricular failure. Their mode of action allows the release of nitric oxide into vascular smooth muscle which improves oxygen supply while reducing the demand for oxygen consumption.
• Frusemide belongs to a group of drugs called diuretics. Their mechanism of action is to work on the kidneys to increase urine volume by reducing salt and water reabsorption from the renal tubules.
• Administering diamorphine to calm the patient allows time for nitrates and diuretics to take effect.
• Some of the adverse side-effects of diamorphine include drowsiness and sedation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


