The person with chronic obstructive pulmonary disease
CASE AIMS
After examining this case study the reader should be able to:
• Briefly explain the causes of chronic obstructive pulmonary disease.
• Outline the pathophysiology associated with chronic obstructive pulmonary disease.
• Discuss the role of the nurse in caring and managing a patient with chronic obstructive pulmonary disease.
• Demonstrate an understanding of the mode of action and side-effects of salbutamol and tiotropium.
CASE
John Smith is 60 years old, married and has two grown-up children. Both of them are married but they all live in the same locality. Mr Smith, who works at the local engineering firm, likes going out to his local pub, and enjoys a night out and a beer with his friends. He has been complaining of a cough with ‘phlegm’ both during the winter and summer. However, these symptoms became worse during the winter after he had suffered a chest infection. His cough has become generally worse in the morning, on waking. John says that cigarettes help him to expectorate. He also claims that the cough is a ‘smoker’s cough’, and not something to worry about. He continues to smoke because he finds that he missed socializing with his friends at work and at the pub when he tried quitting. John has been smoking approximately two packs of cigarettes per day since the age of 17. His wife persuaded him to visit his GP as his cough and daily phlegm production were not going away. He has also recently complained of a sense of increased effort to breathe. After lung function tests, he was diagnosed as suffering from chronic obstructive pulmonary disease (COPD).
One morning, John was having difficulty breathing, and felt hot. He started to have prolonged bouts of coughing which caused him to faint. His wife, who was at home, called the ambulance which took him to the accident & emergency (A&E) department. Following assessment, the doctor explained to Mrs Smith that her husband had experienced an acute exacerbation of his COPD and needed to be admitted to hospital for stabilization.
1 What could have caused John’s COPD?
2 What changes have taken place in John’s respiratory system?
3 How would you care for and manage John’s condition?
To manage and treat the exacerbation of the COPD, the doctor prescribes nebulized salbutamol to dilate his bronchioles and establish normal ventilation. The doctor also prescribes controlled oxygen therapy, oral corticosteroids for the inflammation and antibiotics for the infection.
4 Why has salbutamol been prescribed?
5 What is the normal dose and route of salbutamol?
6 What side-effects might John anticipate from salbutamol and what can you do to mitigate these effects?
After three days, John is much improved. He is apyrexial and he is able to breathe more easily. His vital capacity and peak flow readings are being recorded and show irreversible lung disease. John’s progress is maintained and the possibility of his discharge is being discussed. The doctor decides to prescribe tiotropium once daily to simplify John’s medication regime. He is also on salbutamol to be used as required.
7 How does tiotropium work?
8 What side-effects might John anticipate from tiotropium and what can you do to mitigate these?
ANSWERS
1 What could have caused john’s COPD?
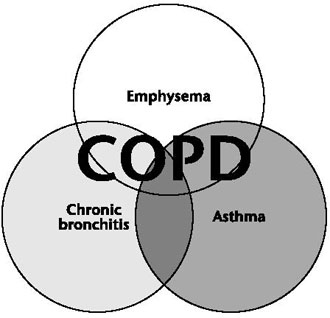
A In COPD there are pathological changes in the main bronchi, the bronchioles, the alveolar ducts, alveolar sacs and the alveoli. The causes of these changes are due to, mainly, cigarette smoke, but not exclusively. So be wary when you encounter patients with COPD, and do not make the assumption that it is self-inflicted by smoking (NICE 2010).
The other causes of COPD are biomass fuel oxidants, industrial pollution, motor exhaust emissions, mineral dusts and particulates, and genetic factors. There are some patients with COPD who have a severe hereditary deficiency of the alpha 1 anti-trypsin, which is a circulating inhibitor of proteases. People who are deficient of alpha 1 anti-trypsin are at increased risk of developing COPD even if they do not smoke (Stoller and Aboussouan 2005).
2 What changes have taken place in John’s respiratory system?
A Following chronic exposure to oxidants in cigarette smoke and other inhaled noxious agents, the respiratory system of a patient with COPD responds to these triggers by unleashing the inflammatory system in a very aggressive way. This aggressive response causes tissue destruction and disables the defence and immune system of the body to limit the tissue destruction as compared to a healthy individual. Furthermore, the inflammatory response disrupts the repair system of the body. Consequently, we see massive structural changes in the airways. These changes continue with disease severity, even after a patient stops smoking (Cosio et al. 2009).
In patients with COPD, the pathological changes to the structure of the airways happen because of two main processes. Firstly, there is an imbalance between proteases and anti-proteases, and secondly there is an imbalance between oxidants and antioxidants in the lungs (MacNee 2007).
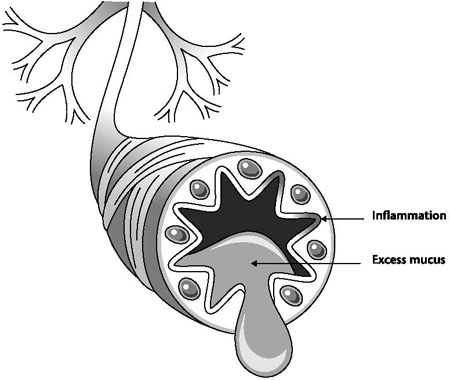
Proteases break down connective tissue component and anti-proteases protect the tissue. Proteases are found in inflammatory cells and epithelial cells, and the level is increased in patients with COPD. When the epithelial cells are damaged by cigarette smoke, many inflammatory mediators are released. Macrophages, neutrophils and T lymphocytes (CD8) in the lungs release proteases which break down connective tissue in the airways, bronchioles and alveoli.
Figure 5.2 Structural changes in bronchial tubes
In emphysema, it is believed that proteases play a major role in its causative factors. Elastin, which is a major connective tissue component of the alveoli, is destroyed by proteases (Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease 2011). Oxidants are generated by cigarette smoke and other noxious gases, and are also released by macrophages and neutrophils. Antioxidants neutralize the effect of oxidants. There is a reduction in endogenous antioxidant in patients with COPD (Rahman 2005).
3 How would you care for and manage John’s condition?
A
• You should sit John upright, supported with an adequate number of pillows and provide a bed table for him to lean forward on and rest in the orthopnoeic position. Oxygen and a bronchodilator should be administered as prescribed. The bronchodilator acts on the peripheral airways, reduces air and traps and reduces lung volume, which will improve John’s breathing and exercise capacity.
• Because there is a potential risk for John to develop respiratory failure, you must be vigilant to the early warning signs. You must monitor the respiration rate, depth and rhythm and observe whether John is having difficulty breathing, showing signs of confusion or disorientation, or of drowsiness, which may indicate cerebral anoxia (Rodriguez-Roisin et al. 2009).
• Pulmonary hypertension and right ventricular hypertrophy are due to the destruction of the pulmonary capillary bed and inflammation of pulmonary arterial vessels. The loss of the pulmonary capillary bed contributes to the increased pressure in the pulmonary circulation. You need to monitor John’s blood pressure closely and administer the prescribed medication. The fluid balance has to be recorded diligently to maintain hydration and electrolyte balance so as to prevent any potential dehydration or circulatory overload.
• Systemic disease and extrapulmonary inflammatory disease occurs in advanced COPD, causing cachexia and loss of fat-free mass, with respiratory and peripheral muscle weakness (Barnes and Celli 2009). This would have implications for John’s ability to carry on with activities of daily living. People with COPD have a higher energy requirement than average. Increased calorie intake is needed to help John to breathe adequately, which means good nutrition is important. You should liaise with the dietician for advice and support to ensure John has adequate nutrition. You should encourage John to take extra-high calorie drinks and added vitamins. If John is unable to tolerate a normal diet due to his breathlessness, you should offer small, easily digestible meals.
4 Why has salbutamol been prescribed?
A Salbutamol is a selective beta2 adrenoceptor agonist that produces broncho-dilation. It acts on the beta2 (B2) receptors in the airway smooth muscle by causing an increase in cyclic adenosine monophosphate (cAMP) levels in the cells. An increase in cAMP concentrations prevents the inflammatory and immunomodulatory cells from carrying out their harmful effect. The smooth muscles in both the large and small airways to relax, enabling them to dilate. This dilation facilitates easier breathing. It also decreases the airway smooth muscle tone and reduces hyperinflation, thus causing rapid relief of symptoms and improving exercise tolerance.
5 What is the normal dose and route of salbutamol?
A Salbutamol has a relatively rapid onset of action, achieving measurable bronchodilation within five minutes and maximal effect in 30 minutes. The effect of the B2 agonist diminishes after two hours and it has a duration of about four to six hours. For regular use, salbutamol must be administered four times daily. It is available in a variety of formulations: pMDIs, nebulized solution, oral and parenteral. Nebulized salbutamol may be appropriate for patients with extremely limited airflows, or in patients who cannot coordinate the use of a pMDI. The actual dose will depend on the route of administration (BNF 2012).
Table 5.1 Dosage of salbutamol according to route of administration (BNF 2012)
| Route | Dose |
| By mouth (but use by inhalation preferred) | 4mg 3–4 times daily |
| By subcutaneous or intramuscular injection | 500mcg 4 times daily if necessary |
| By slow IV injection | Dilute to a concentration of 50mcg per ml Then give 250mcg and repeat if necessary |
| By intravenous infusion | Initially 5mcg per minute, adjusted to a range of 3–20mcg per minute |
| By aerosol inhalation | 100–200mcg (1–2 puffs) 4 times daily |
| By inhalation of powder | 200–400mcg 4 times daily |
| By inhalation of nebulized solution | 2.5–5mg repeated up to 4 times daily 40mg daily is the maximum dose |
Salbutamol is usually given by the inhaled route for direct effect on bronchial smooth muscle. This is usually achieved through an MDI, nebulizer or other proprietary delivery device (e.g. Rotahaler or Autohaler). In these forms of delivery, the maximal effect of salbutamol can take place within 5 to 20 minutes of dosing, though some relief is immediately seen. It can also be given orally as an inhalant or intravenously.
6 What side-effects might John anticipate from salbutamol and what can you do to mitigate these effects?
A
• You should ensure that John is not allergic to any of the constituents of salbutamol (Jordan 2008) before administration. John should be educated to read all labels on medications, whether prescribed or bought over the counter, to ensure there are no drug interactions.
• Salbutamol has positive inotropic effects on the heart, so extra care should be taken with patients with myocardial ischaemia and hypokalaemia. The side-effects, within the cardiovascular system are sinus tachycardia, palpitations, susceptibility to prolonged QT interval and vasodilation. It is very rare for a patient to suffer from cardiac arrhythmias, unless there is some susceptibility. The mechanism may be caused by a direct effect on atrial B2 receptors, combined with a reflex effect from increased peripheral vasodilation via B2 receptors. Short-acting inhaled B2 agonists, such as salbutamol, do not increase the risk of acute MI in patients with COPD.
• You must assess John’s vital signs, such as blood pressure, pulse, temperature and respiration to ensure they are within the normal parameters. If the side-effects outweigh the benefits, the doctor may have to consider an alternative bronchodilator (Hansel and Barnes 2004).
• The side-effects of salbutamol on the central nervous system are headache, restlessness, tension, dizziness and nervousness, and disturbances of sleep and behaviour. John should be told about these possible side-effects and given ways to mitigate them. You should monitor blood pressure lying and standing, and dizziness on standing, and record any difference and advise John accordingly. He should be educated about what strategies he can use to manage his sleep, dizziness and postural hypotension. He should also be advised what medication he should take if he suffers from headache.
• The metabolic side-effects are hypokalaemia, which is caused by a direct effect on the skeletal muscle uptake of potassium via B2 receptors, and is usually a small effect, but can be serious. Hypokalaemia can occur especially when treatment is combined with thiazide diuretics, and this may be the case in patients diagnosed with hypertension. John’s blood potassium levels should be monitored closely. You should also do a 12-lead electrocardiogram (ECG) to have a baseline, and regularly monitor John’s heart rhythm to detect any early signs of hypokalaemia (BNF 2012).
• In patients diagnosed with diabetes mellitus, vigilant monitoring of blood glucose is recommended because salbutamol has a hyperglycaemic effect. There have also been reports of high insulin levels, (hyperinsulinaemia). If John suffers from diabetes mellitus he should be encouraged to check his blood glucose levels regularly and to have an action plan to deal with hyperglycaemia.
• The possible side-effects on the skeletal muscle are fine tremor, particularly in the hands, and muscle cramps However, in some elderly patients treated with high doses of B2 agonists, due to a direct effect on skeletal muscle B2-receptors, the tremors and cramps may be more pronounced. John should be advised to contact a doctor or respiratory specialist nurse if the tremors and muscle cramps appear to be getting worse.
7 How does tiotropium work?
A In patients with COPD, the cholinergic pathways may be activated by inflammatory mediators and inhaled irritants such as cigarette smoke. When this happens, vagal cholinergic tone provokes an increase bronchoconstriction and mucus production. This sequence of events causes the patient to become breathless and start coughing up sputum. When the patient is administered an anticholinergic drug, such as tiotropium, the bronchioles become dilated and the patient feels an improvement in breathing. There is also a reduction in the amount of sputum produced.
Tiotropium is a long-acting anticholinergic drug. Its long duration of action makes it appropriate for use once a day, which helps compliance and concordance. It is inhaled once a day from the ‘HandiHaler’, a specialized dry powder inhalation system (Chen et al. 2008).
8 What side-effects might John anticipate from tiotropium and what can you do to mitigate these?
A
• The British National Formulary (BNF) reports the following side-effects: constipation, cough, stomatitis, gastro-oesophageal reflux disease, pharyngitis, dysphonia, dysphagia, dysuria, epistaxis and oropharyngeal candidiasis. John should be educated about these side-effects and the strategies to mitigate them.
• The extensive use of the drug in its inhaled form, in a variety of doses and settings, has shown it to be safe. Side-effects include dry mouth and metallic taste. You should advise John to have boiled sweets and drinks readily available, and ice chips to take if his mouth becomes dry.
• Men with prostate disease should be monitored closely for urinary tract effects, because some prostatic symptoms have been reported, however there is no evidence of any causal link. You should monitor John’s urine output, by the use of a fluid balance. John should be educated as to the signs and symptoms of urine retention and asked to tell a nurse if he is concerned about his urine output.
• John should be educated and assessed on the right technique for using the inhaler device correctly.
• Tiotropium should be used with caution in patients with glaucoma, since the tiotropium solution with a facemask may precipitate glaucoma, probably due the direct effect of the solution to the eye. Any patients who may be vulnerable to potential systemic anticholinergic side-effects should not be given tiotropium. If John requires tiotropium by the nebulized route, you should stay with him and ensure that a tight-fitting facemask is used to prevent any solution from splashing into his eyes.
KEY POINTS
• COPD is a chronic and progressive disorder which is characterized by inflammation, airflow obstruction and alveolar damage.
• Some response to pharmacological and other therapies can be achieved but they may have limited or no impact on the airflow obstruction.
• Salbutamol causes the smooth muscles in both the large and small airways to relax, enabling them to dilate.
• The side-effects of salbutamol are fine tremor in the hands, muscle cramps, restlessness, tension and dizziness.
• Tiotropium prevents bronchoconstriction and lessens mucus secretion.
• The side-effects of tiotropium include dry mouth, metallic taste, constipation, cough, stomatitis and gastro-oesophageal reflux disease.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree