The person with schizophrenia
CASE AIMS
After examining this case study the reader should be able to:
• Discuss why a service user’s past history is important in the diagnosis of schizophrenia.
• Explain why the diagnosis of schizophrenia in immediate family could be significant.
• Describe the pathophysiological changes that are thought to be occurring in the brain of a service user with schizophrenia.
• Demonstrate an understanding of the mode of action and side-effects of haloperidol in the treatment of schizophrenia.
• Articulate what is meant by dystonic symptoms and explain how haloperidol causes these.
• Outline the role of the nurse in monitoring and caring for a person taking olanzapine.
• Discuss the relationship between weight gain, type 2 diabetes and taking olanzapine.
• Discuss the problems of concordance with medication in a service user with schizophrenia.
CASE
John P is a 25-year-old male with the diagnosis of schizophrenia. He was a healthy child, but his parents report that he was a bed-wetter and seemed slower to develop than his brothers and sisters. A maternal uncle has also been diagnosed with schizophrenia.
1 Discuss why John’s past history is important in his diagnosis of schizophrenia
2 Explain why the diagnosis of schizophrenia in John’s uncle could be significant
3 What pathophysiological changes are thought to be occurring in John’s brain?
4 What type of medicine is haloperidol and what is its mode of action?
5 What is meant by dystonic symptoms and why should the haloperidol cause these?
6 Outline the role of the nurse in monitoring and caring for a person taking olanzapine
7 Why should John have put on weight and developed diabetes while on olanzapine?
John’s parents support him financially. His brothers and sisters are angry with, and frightened of, him and have nothing to do with him. They are particularly upset by his lack of interest in the outside world. John lives in a boarding home and works in a sheltered workshop with difficulty. He sees a psychiatrist for 15 minutes every two months but sometimes misses his appointment. He has a social worker who he sees often. The psychiatrist would like to switch John to long-acting injectable antipsychotic treatment, but John is afraid of injections and isn’t sure that he needs this medication. He usually misses his appointments with his primary care physician.
8 Discuss the problems of concordance with medication in a service user with schizophrenia
ANSWERS
1 Discuss why John’s past history is important in his diagnosis of schizophrenia
A
• Information about the medical and psychiatric history of the family, details about pregnancy and early childhood, history of travel, and history of medications and substance abuse are all important. This information is helpful in ruling out other causes of psychotic symptoms. John may have had an unexceptional childhood but began to experience a noticeable change in personality and a decrease in academic, social and interpersonal functioning during mid- to late adolescence.
• In retrospect, family members may describe the person with schizophrenia as a physically clumsy and emotionally aloof child who may have been anxious and preferred to play by himself or herself. The child may also have been late to learn to walk and may have been a bed wetter (Hyde et al. 2008).
• History-taking is especially important as, usually, one or two years pass between the onset of vague symptoms and the first visit to a psychiatrist (Ho and Andreasen 2001).
2 Explain why the diagnosis of schizophrenia in John’s uncle could be significant
A The risk of schizophrenia is elevated in biological relatives of patients but not in adopted relatives. The risk of schizophrenia in first-degree relatives of people suffering from schizophrenia is 10%. If both parents have schizophrenia, the risk of the condition in their child is 40%. Concordance for schizophrenia is about 10% for dizygotic twins and 40–50% for monozygotic twins. The gene variants that have been so far implicated are responsible for only a small fraction of schizophrenia, and these findings have not always been replicated in different studies. The genes that have been found mostly change a gene’s expression or a protein’s function in a small way. Interactions with the rest of the genome and with the environment will doubtless prove to be important (Picchioni and Murray 2007).
3 What pathophysiological changes are thought to be occurring in John’s brain?
A
• Particular attention has been paid to the function of dopamine in the causation of schizophrenia. This focus largely resulted from the accidental finding that phenothiazine drugs, which block dopamine function, could reduce psychotic symptoms. This is also supported by the fact that amphetamines, which trigger the release of dopamine, may exacerbate the psychotic symptoms in schizophrenia.
• The influential dopamine hypothesis of schizophrenia proposed that excessive activation of D2 receptors was the cause of (the positive symptoms of) the condition. However, newer anti-psychotic medication (atypical antipsychotic medication) can be just as effective, but these drugs also affect serotonin function and may have slightly less of a dopamine blocking effect (Jones and Pilowsky 2002).
• Interest has also focused on the neurotransmitter glutamate and the reduced function of the N-methyl-D-aspartate glutamate receptor in schizophrenia (Rang et al. 2011).
4 What type of medicine is haloperidol and what is its mode of action?
A
• Haloperidol is a typical antipsychotic medicine. It is in the butyrophenone class of anti-psychotic medications and has pharmacological effects similar to the phenothiazines (BNF 2012).
• The ability of certain drugs to act on dopaminergic transmission and relieve the symptoms of psychosis was the basis of the dopamine hypothesis of schizophrenia first postulated in the 1960s. Most typical antipsychotics act at D2 receptors (Barber and Robertson 2012).
• It may take several weeks for haloperidol to have its full effect and these drugs are associated with many side-effects.
5 What is meant by dystonic symptoms and why should the haloperidol cause these?
A
• Dystonia is a syndrome of spasms and sustained contractions of the muscles. These muscle movements are not under voluntary control and they result in repetitive abnormal movements of parts of the body or persistently abnormal postures.
• Dystonia can affect virtually any single part of the body or several different areas at once.
• Although the causes of dystonia are not fully known it is currently thought that the con-dition results from a malfunction in a part of the brain called the basal ganglia: structures situated deep in the brain that help to regulate voluntary and involuntary movement by controlling muscle contractions in the body. The problem may mainly lie in an area of the basal ganglia called the globus pallidus. The fault in the basal ganglia may be caused by haloperidol as it affects dopaminergic receptors (BNF 2012).
6 Outline the role of the nurse in monitoring and caring for a person taking olanzapine
A The nurse’s role in monitoring and caring for a person taking olanzapine should involve the following.
MONITORING WHITE BLOOD CELL COUNT
A condition called agranulocytosis (white blood cell count below 3500) can be a life-threatening side-effect of this medication, which may also suppress bone marrow and lower infection-fighting ability (Tolosa-Vilellaa et al. 2002). Therefore the nurse would advise the service user and caregiver to keep appointments for laboratory testing. They would also instruct the service user to immediately report any sore throat, signs of infection or fatigue without apparent cause.
OBSERVING FOR ADVERSE EFFECTS
Olanzapine may affect:
• blood pressure;
• heart rate;
• other autonomic functions.
Therefore the service user should be instructed to report side-effects (Karch 2008) such as:
• drowsiness;
• dizziness;
• depression;
• anxiety;
• tachycardia;
• hypotension;
• nausea/vomiting;
• excessive salivation;
• urinary frequency or urgency;
• incontinence;
• weight gain;
• muscle pain or weakness;
• fever.
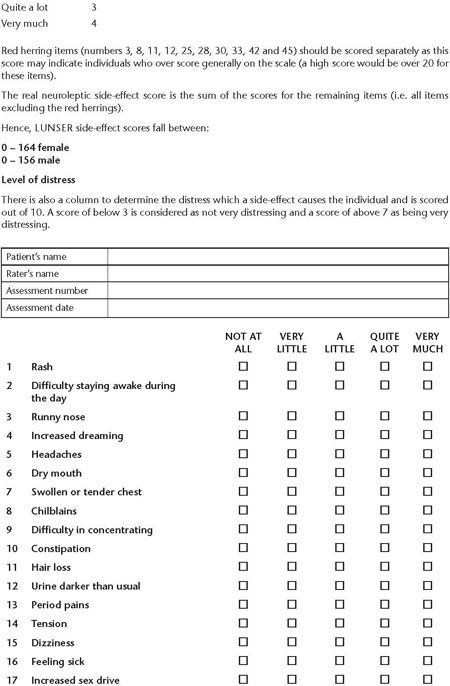
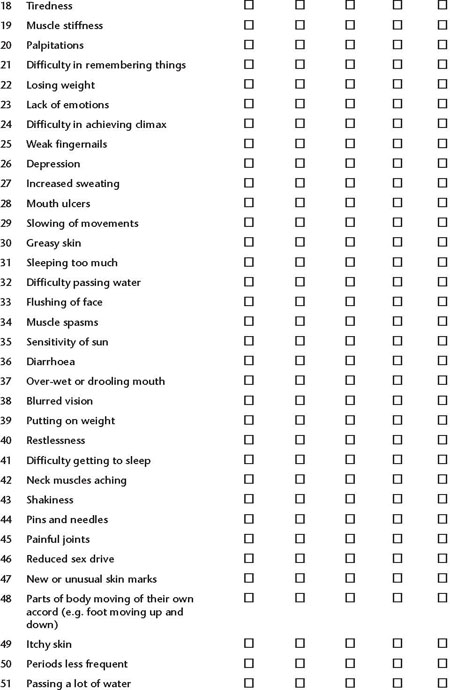
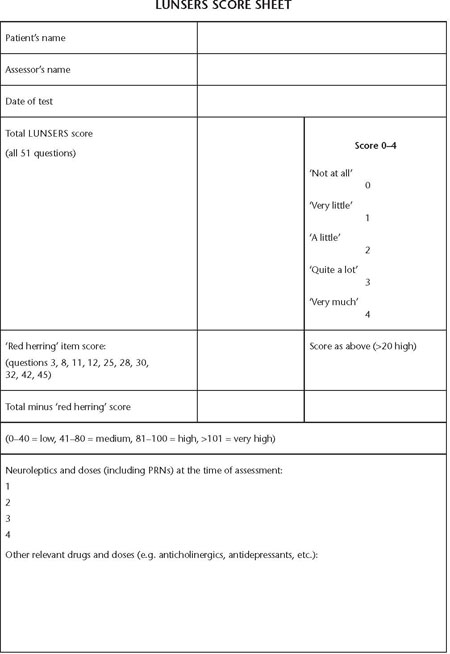
The Liverpool University Neuroleptic Side-effect Rating Scale (LUNSERS) has been developed to enable service users to report their experiences of side-effects: the ‘LUNSERS may be a useful tool for systematically eliciting side-effect information from patients, and as a brief and cost-effective measure of side-effects in research studies’ (Day et al. 1995: 653) (see Figure 20.1).
MONITOR EFFICACY OF THE MEDICATION
The nurse should observe for a decrease of psychotic symptoms. Decreased symptoms indicate an effective dose and type of medication. The nurse should be noticing increases or decreases of symptoms of psychosis, including hallucinations, abnormal sleep patterns, social withdrawal, delusions or paranoia. If symptoms do not decrease over a six-week period then further medical intervention may be considered.
MONITOR ALCOHOL AND ILLEGAL DRUG USE
Used concurrently, these will cause increased CNS depression. The service user may decide to use alcohol or illegal drugs as a means of coping with the symptoms of psychosis, so may stop taking the drug. It may be difficult, but the service user should be encouraged to avoid alcohol or illegal drug use. It might be advantageous to refer the person to a support group as appropriate. The service user should be encouraged to increase dietary fibre, fluids and exercise, to prevent constipation. To relieve the symptoms of a dry mouth it may be useful to suggest sucking sugar-free hard sweets or chewing gum, and taking frequent drinks of water.
The service user should be told to immediately notify the health care provider if urinary retention occurs.
OBSERVE FOR NEUROLEPTIC MALIGNANCY SYNDROME
Neuroleptic malignancy syndrome is a life-threatening neurological disorder most often caused by an adverse reaction to neuroleptic or antipsychotic medication. The nurse should observe for muscle rigidity, fever, autonomic instability and cognitive changes such as delirium, and associated with elevated creatine phosphokinase. Generally, removal of the antipsychotic drug treatment, along with supportive medical management, lead to a positive outcome (Strawn et al. 2007).
Figure 20.1 is set out as follows:
7 Why should John have put on weight and developed diabetes while on olanzapine?
A Service users taking either olanzapine or risperidone show significant weight gain as compared to those taking typical phenothiazines. Several explanations have been proposed for gaining weight while taking atypical antipsychotic drugs. These medications may have an affinity for dopamine, serotonin and histamine receptors that could lead to increased eating and weight gain (Farwell et al. 2004). Weight gain is not the cause of diabetes mellitus among patients taking atypical antipsychotics but suggests that the development of diabetes is due to an independent effect of atypical antipsychotic drugs on metabolism.
In the UK, guidelines published by NICE for the treatment of schizophrenia in secondary and primary care (2009) recommend that primary and secondary care practitioners provide routine physical checks for people with schizophrenia unless the service user does not want contact with or has no GP.
8 Discuss the problems of concordance with medication in a service user with schizophrenia
A One of the major clinical problems in the treatment of people with schizophrenia is partial or complete non-concordance with medication and this limits the clinical effectiveness of the prescribed drugs. Antipsychotic medication can only be effective if it is taken continuously over a sustained period of time (Kikkert et al. 2006).
LACK OF INSIGHT
The problem of non-concordance may be more prevalent among those with schizophrenia due to the nature of the condition – for example, due to a lack of insight. Non-concordance with medication is often linked to the person’s level of insight into their illness and lack of insight is a frequent concomitant of psychosis. In schizophrenia, insight has been defined as an awareness of illness – an ability to recognize the symptoms as part of the illness and the need for treatment. Patients diagnosed with schizophrenia have been shown to be partially or totally lacking insight into the presence of their mental disorder and these individuals are often difficult to engage with treatment (Urquhart 2005).
HEALTH BELIEF SYSTEMS
Some patients may have their own explanations of their illnesses, such as religious or cultural beliefs which may not coincide with the western medical model of mental disorders, and this can be even more complicated if one tries directly to impose the models of insight on patients from non-western cultures. Gamble and Brennan (2006) suggest that different cultures in the UK perceive mental illness in different ways and that this can have an impact on treatment as some cultures prefer to seek help from religious leaders rather than mental health services. Alternatively, religion or spiritual beliefs in western culture can have a positive impact on concordance with medication, as religious individuals with schizophrenia have better social support compared to non-religious individuals.
STIGMA
Patients can have different levels of awareness into their illness and they may consciously or unconsciously avoid acknowledging that they are suffering from mental health problems because of their reluctance to bear the stigma of being mentally ill. The power and influence of the media with respect to mental illness has been a key issue of debate over many years as people with schizophrenia are frequently portrayed as violent and dangerous. Gamble and Brennan (2006) emphasize this point by stating that when the boxing champion Frank Bruno was admitted to hospital in 2003, one of the newspaper headlines was ‘Bonkers Bruno Locked Up’. Stigma has the grave potential to cause reluctance to seek treatment and can be detrimental to the person’s health as a result of stereotyping (DH 1999).
SELF-MEDICATION WITH ALCOHOL AND ILLICIT DRUGS
There is evidence that patients with schizophrenia who misuse illicit drugs and alcohol have an increased rate of re-hospitalization. The higher relapse rate in people with established schizophrenia who use substances may be partially explained by non-concordance to the medication regimen. Evidence suggests that the substance used most frequently by people with schizophrenia is cannabis (Gamble and Brennan 2006).
NEWER MEDICINES LEAD TO GREATER CONCORDANCE
It has been widely assumed that the introduction of atypical (second-generation) anti- psychotics has revolutionized the management of schizophrenia and will lead to improved concordance with medication regimes for patients with this condition. However, there is an argument that despite the introduction of so-called second-generation antipsychotics, there is no significant difference in the rates of concordance.
DOCTOR–SERVICE USER RELATIONSHIP
Concordance with prescribed antipsychotics will be difficult to achieve in people with schizophrenia who are not well engaged with mental health services and who are not experiencing good therapeutic relationships with psychiatric professionals. NICE (2009) recommends that prescribing antipsychotic medications should be a joint decision by the clinician and the service user, and this discussion should be documented in the service user’s notes.
KEY POINTS
• History-taking is especially important as usually one to two years pass between the onset of vague symptoms and the first visit to a psychiatrist.
• The risk of schizophrenia is elevated in biological relatives of patients but not in adopted relatives.
• Particular attention has been paid to the function of dopamine in the causation of schizophrenia.
• Antipsychotic drugs in general interfere with the functioning of several neurotransmitters and receptors, notably dopamine.
• Dystonia is a syndrome of spasms and sustained contractions of the muscles.
• The nurse should monitor for a range of side-effects in a patient taking clozapine and track white blood cell count, blood pressure, heart rate and other autonomic functions along with looking for signs of neuroleptic malignancy syndrome.
• Although it is difficult to know for sure, studies suggest that people taking olanzapine may be at a higher risk of developing diabetes.
• One of the major clinical problems in the treatment of people with schizophrenia is partial or complete non-concordance with medication and this limits the clinical effectiveness of the prescribed medication.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree