The person with pain
CASE AIMS
After examining this case study the reader should be able to:
• Describe the features of the hip joint.
• Highlight the anatomical structures that would aid in the stability of the hip joint.
• Briefly explain how the sensation of pain is brought about at a neuronal level.
• Demonstrate an understanding of the mode of action of paracetamol.
• Discuss the role of the nurse in advising patients taking paracetamol.
• Describe the pathophysiology of osteoarthritis.
• Demonstrate an understanding of the mode of action and side-effects of arthrotec.
• Explain the mode of action of morphine in relieving post-operative pain
• Outline the role of the nurse in monitoring and caring for a patient receiving morphine post-operatively.
CASE
Emma is a 68-year-old woman who lives in a town outside a large urban centre in the north-west of England. She is a single mother of three grown children and still cares for one of her children who has a disability, at home. She is self-employed so that she can maintain an income and care for her child. A few years ago Emma started feeling pain in her hip and found it increasingly difficult to walk. During an appointment with her GP, she complained of the pain and was prescribed paracetamol. At first, the medication appeared to diminish some of the pain.
1 Describe the features of Emma’s synovial hip joints
2 What anatomical structures would aid in the stability of Emma’s hip joint?
3 How is Emma’s sensation of pain brought about at a neuronal level?
4 Describe how giving paracetamol to Emma is thought to bring about analgesia
5 What advice would you give Emma about her paracetamol?
6 Describe briefly how the condition of osteoarthritis would affect Emma’s joints
7 How would arthrotec work in relation to the inflammation caused by Emma’s osteoarthritis and what are the side-effects?
After two years of suffering, Emma urged her GP to refer her to a specialist about her hip pain. She also told her doctor about her concerns regarding the side-effects of the medications she had been taking over the past several years. Her GP agreed to refer her to an orthopaedic surgeon. The surgeon has now carried out a total hip replacement and Emma is now being cared for on an orthopaedic ward. She has just returned from the operating theatre and is receiving morphine via a patient-controlled analgesia device. The device contains morphine 50mg in 50ml; she receives a demand dose of 1mg in 1ml with a lockout period of five minutes.
8 Explain the mode of action of morphine in relieving Emma’s post-operative pain
9 Outline the role of the nurse in monitoring and caring for Emma as she receives morphine
ANSWERS
1 Describe the features of Emma’s synovial hip joints
A Emma’s synovial joints are her most mobile. They possess the following characteristic features (Marieb 2010).
• The articular surfaces are covered with hyaline cartilage. This cartilage is avascular, non-nervous and elastic. Lubricated with synovial fluid, the cartilage forms slippery surfaces for free movements.
• Between the articular surfaces there is a joint cavity filled with synovial fluid. The cavity may be partially or completely subdivided by an articular disc known as the meniscus.
• The joint is surrounded by an articular capsule which is fibrous in nature and lined with synovial membrane. Because of its rich nerve supply the fibrous capsule is sensitive to stretches imposed by movements.
• Varying degrees of movement are always permitted by the synovial joints.
2 What anatomical structures would aid in the stability of Emma’s hip joint?
A There are various factors maintaining the stability at Emma’s hip joint. These are described below in order of their importance (Tortora and Derrickson 2009).
• Muscles – the tone of different groups of muscles acting on the joint is the most important and indispensable factor in maintaining stability. Without muscles, the knee and shoulder would be unstable and the arches of the feet would collapse.
• Ligaments – are important in preventing any over-movement and in guarding against sudden accidental stresses. However, they do not help against a continuous strain because once stretched they tend to remain elongated.
• Bones – help in maintaining stability only in firm-type of joints such as the hips and ankles. Otherwise in most joints their role is negligible.
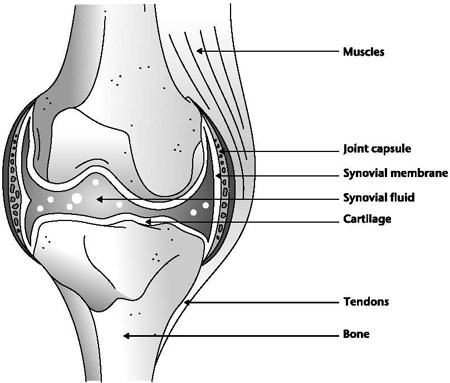
Figure 17.1 Anatomy of a synovial joint
3 How is Emma’s sensation of pain brought about at a neuronal level?
A At rest, the inside of Emma’s nociceptive neuron has a negative charge compared to the outside, which is positive. In order to trigger the sensation of pain in Emma, the inside of the neuron must become positively charged as compared to the outside. Chemicals liberated by damaged tissue bring about a change in the neuronal membrane, allowing sodium to pass into the neuron. This continues until the inside of the neuron is positively charged in relation to the outside. This build-up of positively charged sodium is termed ‘depolarization’ (Tate et al. 2008). At the synapse, where one neuron meets another, neurotransmitters must be released in order to stimulate the next neuron to continue to pass the message onwards. Once the inside of the neuron has converted to a positive environment, calcium channels in the membrane open, so allowing calcium to enter. The influx of calcium attracts small sacs called synaptic vesicles, which are full of neurotransmitters, towards the synapse. When these vesicles reach the synapse they fuse with the neuron membrane and pour their cargo of neurotransmitter into the synapse itself.
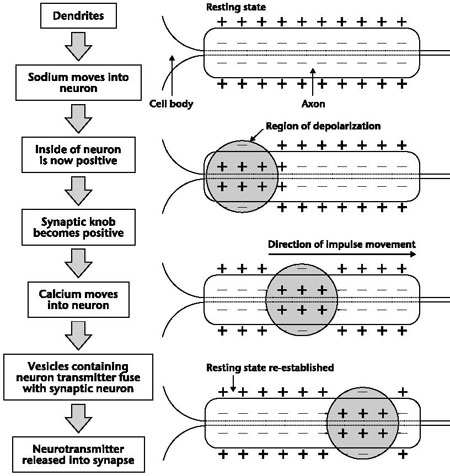
Figure 17.2 Firing of a neuron
4 Describe how giving paracetamol to Emma is thought to bring about analgesia
A Emma’s body is producing prostaglandins in response to injury from her osteoarthritis. One of their actions is to sensitize nerve endings, so that when the injury is stimulated it causes pain (presumably to prevent us from causing further harm to the area). As paracetamol reduces the production of these nerve-sensitizing prostaglandins it is thought it may increase our pain threshold, so that although the injury remains, we can feel it less (Hinz et al. 2008).
5 What advice would you give Emma about her paracetamol?
A
• You should first ascertain whether Emma has an allergy to paracetamol or similar products. According to Jordan (2008), hypersensitivity or allergic responses are possible with almost any drug.
• Paracetamol should be used with caution in people who have renal or liver disease, so again you should check Emma’s medical history. It is possible that regular intake of large doses over a long period may increase the risk of kidney damage (Rang et al. 2011).
• You should inform Emma that she should not take this medicine with any other paracetamol-containing products. This is because other medicines that contain paracetamol in combination with this medicine can easily result in exceeding the maximum recommended daily dose. Many cold and flu remedies and over-the-counter painkillers contain paracetamol so she should be advised to check the ingredients of any other medicines before taking them, or ask the pharmacist for advice (Barber and Robertson 2012).
• Emma should not exceed the dose stated in the information leaflet supplied with her medicine. This is because an overdose of paracetamol is dangerous and capable of causing serious damage to the liver and kidneys. Emma should seek immediate medical advice in the unlikely event of an overdose, even if she feels well, because of the risk of delayed, serious liver damage (Brenner and Stephens 2009).
• If symptoms persist she should consult her doctor, so that more appropriate treatment can be offered.
6 Describe briefly how the condition of osteoarthritis would affect Emma’s joints
A Osteoarthritis is the most common form of joint disease. It causes pain and stiffness in the joints and affects at least 8 million people in the UK. When Emma’s joint becomes affected by osteoarthritis its surfaces become damaged and it doesn’t move as well as it should. The following happens:
• the articular cartilage becomes rough and thin;
• the bone at the edge of the joint grows outwards, forming bony spurs called osteophytes;
• the synovium may swell and produce extra fluid, causing the joint to swell;
• the capsule and ligaments slowly thicken and contract.
In severe osteoarthritis the cartilage can become so thin that the bones may start to rub against each other and wear away. The loss of cartilage, the wearing of bone and the osteophyte formation can alter the shape of the joint, forcing the bones out of their normal position (Arthritis Research in the United Kingdom 2011).
7 How would arthrotec work in relation to the inflammation caused by Emma’s osteoarthritis and what are the side-effects?
A MODE OF ACTION
• Prostaglandins are very important in triggering the inflammatory response and are formed when a fatty acid called arachidonic acid is liberated from a damaged cell membrane by action of an enzyme known as phospholipase.
• The arachidonic acid acts by triggering the cyclo-oxygenase pathway. Cyclo-oxygenase pathways in most pharmacological texts are denoted by the prefix COX followed by the number of the pathway (e.g. COX1).
• The prostaglandins derived from COX1 assist in the smooth running of body systems; in particular they help to maintain the protective mucous lining of the stomach and intestine.
• COX2 in comparison produces prostaglandins that facilitate pain and inflammation.
• Arthrotec works by inhibiting the formation of prostaglandins by blocking the cyclo-oxygenase pathways (BNF 2012).
SIDE-EFFECTS
The vast number of current NSAIDs (including diclofenac) blocks both pathways. This is problematic as the drugs reduce the pain and inflammation associated with COX2 but also reduce the homeostatic function of COX1. This leads to a number of GI problems, the most significant of which is peptic ulceration. Often, oral administration of a prostaglandin substitute, such as misoprostol, may be used. This helps to ensure limited damage to the stomach mucosa. Arthrotec is such a drug as it combines in one tablet diclofenac and misoprostol (BNF 2012).
8 Explain the mode of action of morphine in relieving Emma’s post-operative pain
A
• All opioids exert their effect through binding with specific receptors called opioid receptors, located in the CNS (brain and spinal cord) or peripherally in the GI tract. There are four types of opioid receptor and they are designated by the Greek letters μ (mu), κ (kappa), σ (sigma) and δ (delta).
• Opioid drugs mimic our own endorphins, bringing about a similar analgesic reaction. There are numerous opioid analgesic preparations, some natural (e.g. morphine and codeine) and some synthetic (e.g. diamorphine, methadone, fentanyl and meperidine).
ANALGESIA
This term refers to the loss or relief of pain but without the loss of consciousness. Morphine is useful in both acute and chronic types of pain. It not only raises the level at which pain is initiated (higher threshold) but it also alters the brain’s perception of pain. The patient is still aware of the pain but does not recognize it as an unpleasant sensation.
9 Outline the role of the nurse in monitoring and caring for Emma as she receives morphine
A
• As part of your post-operative care you will be taking Emma’s blood pressure. This is an important parameter to monitor when someone is receiving morphine as the drug can cause a drop in blood pressure, as it produces vasodilatation and can increase the release of histamine in an individual (Adams et al. 2008).
• You should monitor Emma’s respiratory rate and depth. Respiratory depression is caused by the respiratory centre in the brain stem becoming less sensitive to the respiratory drive of carbon dioxide. It is one of the more troublesome side-effects that you need to be aware of, particularly as it can occur with therapeutic doses. It is also the commonest cause of death in acute opioid poisoning. Medication may be withheld for any difficulty in breathing or respirations below 12 breaths per minute.
• Opioid effects (adverse or otherwise) can be reversed with an opioid antagonist such as naloxone. The elimination half-life of naloxone can be shorter than that of the opioid itself, so repeat dosing or continuous infusion may be required.
• Emma should be assessed regarding the location, quality, intensity and frequency or duration of her pain. Use a nominal scale to determine intensity. Often a numerical score is used and these scales range from a low number usually indicating a low level of pain to a high number indicating worsening or more intense pain (Seers 1988).
• Morphine also affects the smooth muscle of the urinary tract. Therefore it is important that you monitor renal status and urinary output. Morphine may cause urinary retention due to muscle relaxation in the urinary tract.
• Opiates are excreted through the kidneys. Impaired kidney function may result in reduced medication clearance and increased serum drug levels (Aschenbrenner and Venable 2008).
• Nausea and vomiting occurs in up to 40% of people who are prescribed morphine when they first start to take the drug. You should first of all prepare for this by making sure a vomit bowl and tissues are available. You should chart the frequency of the vomiting and often there is an assessment scale for this purpose. Mouth care is important to consider. Emma will have been prescribed an antiemetic. It is probably easier to prevent than to treat established nausea and vomiting, so any patient with a risk score for post-operative nausea and vomiting (PONV) of 2 and above should receive prophylactic antiemetic agents according to that trust’s protocol (Gan et al. 2003).
• Monitor Emma for constipation. Opioids have an antispasmodic effect on the GI tract, which decreases peristaltic activity. Therefore you may need to increase dietary fibre or administer laxatives (Brunner et al. 2009).
• Immediately report effects such as untoward or rebound pain, restlessness, anxiety, depression, hallucination, nausea, dizziness and itching. Emma’s respiratory rate should be maintained at least at 12 breaths per minute.
KEY POINTS
• Synovial joints possess the following characteristic features: articular surfaces covered with hyaline cartilage; a joint cavity filled with synovial fluid; the joint is surrounded by an articular capsule which is fibrous in nature and is lined with synovial membrane; synovial fluid lubricates the joint and nourishes the articular cartilage.
• There are various elements maintaining stability at the hip joint: muscles, ligaments and bones.
• In order to trigger the sensation of pain, the inside of a neuron must become positively charged as compared to the outside.
• Paracetamol reduces the production of nerve-sensitizing prostaglandins and it is thought it may increase our pain threshold, so that although the injury remains, we can feel it less.
• If other medicines containing paracetamol are taken in combination with paracetamol, this can easily result in overdose.
• Osteoarthritis is the most common form of joint disease. It causes pain and stiffness in the joints and affects at least 8 million people in the UK.
• The vast numbers of current NSAIDs block both cyclo-oxygenase pathways. This is problematic because these drugs reduce the pain and inflammation associated with COX2 but also reduce the homeostatic function of COX1. This leads to a number of GI problems such as peptic ulceration.
• All opioids exert their effect through binding with specific receptors called opioid receptors located in the cCNS (brain and spinal cord) or peripherally in the GI tract.
• Different opioid analgesics bind in different ways with a variety of receptors, so explaining why a range of effects and side-effects can occur.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


