The person with osteoporosis
CASE AIMS
After examining this case study the reader should be able to:
• Describe the process of normal bone remodelling.
• Briefly explain how bone density changes through a person’s lifespan.
• Define osteoporosis and discuss how it affects bone fragility.
• Identify the risk factors for the development of osteoporosis.
• Demonstrate an understanding of the mode of action and side-effects of bisphosphonates.
• Discuss the role of the nurse in advising patients regarding taking bisphosphonates.
• Discuss the role of the nurse in giving lifestyle advice to a patient with osteoporosis.
CASE
Mrs H, a 57-year-old, presented in A&E with a painful right wrist following a fall. She reported slipping on wet grass while walking her dog. Mrs H’s wrist was manipulated and immobilized in a below-elbow back slab and she was discharged from the department with plaster instructions and an appointment for a review at the fracture clinic.
Mrs H is a teacher and she works full time at the local high school. She is married with two children and four grandchildren. She has no significant medical or surgical history apart from having had a total hysterectomy and bilateral salpingo-oophorectomy at the age of 39 years. She does not take any regular medication. Mrs H was prescribed hormone replacement therapy (HRT) following her hysterectomy but stopped taking it about 10 years ago after media publicity regarding the increased risks associated with the long-term use of HRT. Mrs H does not smoke; she enjoys an occasional glass of wine when eating out and regularly takes her grandchildren swimming. She is 167cm tall and weighs 64kg.
Mrs H returned to the fracture clinic a few days later and was reviewed by the orthopaedic consultant. She had sustained a fragility fracture and the consultant suspected she might have osteoporosis. He advised her to see her GP for further investigation. The GP referred Mrs H for a dual-energy X-ray absorptiometry (DXA) scan to measure her bone mineral density (BMD).
1 Describe the process of normal bone remodelling in Mrs H
2 How does bone density change through a person’s lifespan?
3 Define osteoporosis and discuss how it affects bone fragility
4 Identify the risk factors for the development of osteoporosis
Some weeks later the DXA scan was performed and Mrs H returned to her GP for the results. BMD is measured at the hip and the lower spine and the results are recorded as a standard deviation compared against the normal reference range for healthy young adults (T-score) and the normal reference range for a person of the same age (Z-score). NICE (2008) defines osteoporosis as a T-score of –2.5 standard deviations or below on DXA scanning. Mrs H has a T-score of –2.9 at the hip and the diagnosis of osteoporosis was confirmed. The GP outlined the treatment options and, following discussion, Mrs H was prescribed alendronate 70mg once a week.
5 What effect do bisphosphonates have on bone turnover?
6 What advice would you give to Mrs H in relation to taking her medication?
7 What additional advice would you give to Mrs H?
ANSWERS
1 Describe the process of normal bone remodelling in Mrs H
A The main cells in bone homeostasis are osteoblasts, osteocytes and osteoclasts:
• osteoblasts are bone-building cells that synthesize and secrete collagen and other components that constitute the extracellular matrix of bone tissue;
• osteocytes are mature bone cells that monitor and maintain bone tissue;
• osteoclasts are responsible for the resorption of the extracellular matrix of bone (Rang et al. 2012).
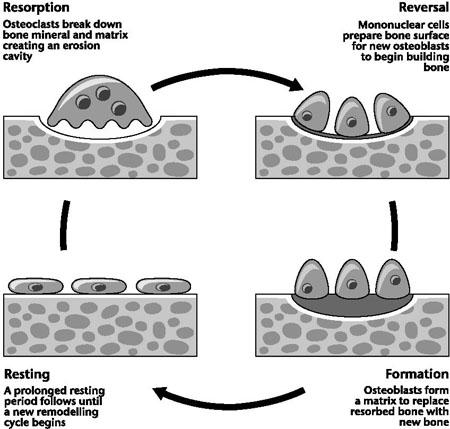
Bone is a complex and dynamic living tissue that is constantly being remodelled. Bone remodelling is a process of bone resorption and bone formation, whereby older, weaker bone is replaced by newer, stronger bone, in response to a variety of factors including exercise, diet, drugs and injury (Tortora and Nielson 2009). The process involves the activity of osteoblasts and osteoclasts, the actions of cytokines, the turnover of the main bone minerals, calcium and phosphate, and the actions of several hormones including, among others, parathyroid hormone (PTH), the vitamin D family and oestrogens.
The cycle begins with osteoclast precursor cells, called into action by cytokines and hormones, which are activated by osteoblasts to develop into osteoclasts. Once released, these cytokines activate osteoblasts which take over the freshly dug resorption pit. The osteoblasts synthesize and secrete osteoid to refill the pit and, having completed their job, the cytokines are embedded in it again to await their next call to action. The osteoid is then mineralized as calcium phosphate crystals (hydroxyapatite) are laid down. Some of the osteoblasts become trapped in the osteoid and become terminal osteocytes and others go on to activate osteoclast precursors and the cycle begins again (Rang et al. 2012).
2 How does bone density change through a person’s lifespan?
A
• In childhood, osteoblast activity is greater than osteoclast activity to enable skeletal development – i.e. growth. At this stage it takes around two years to renew the entire skeleton (compared to 7–10 years in adults).
• Bone stops growing in length at around 16–18 years of age but continues to increase in density until the mid-twenties. At this stage, bone formation and bone resorption are intimately balanced.
• In both men and women, peak bone mass is achieved at around age 35 and after this there is a gradual bone loss of approximately 0.5–1% per year.
• Once this has settled down, bone loss associated with advancing age is seen in both men and women, is due more to decreased osteoblast numbers and affects mainly cortical bone (Tortora and Nielson 2009).
3 Define osteoporosis and discuss how it affects bone fragility
A Osteoporosis is a skeletal disorder characterized by a reduction in bone density and quality as a result of increased bone resorption in relation to bone formation. Bones become progressively porous, brittle and fragile and are at increased risk of fracture. It is often called the ‘silent disease’ because there are no warning signs or symptoms prior to fracture (see www.iofbonehealth.org).
Osteoporotic fractures are called ‘fragility fractures’ because they occur in the course of normal daily activity or as a result of minimal trauma such as a fall from standing height or less. The most common sites of fracture are the vertebrae (spine), hip and distal radius (wrist); however, individuals with osteoporosis have an increased risk of all types of skeletal fractures (see www.nos.org.uk).
The incidence of fractures increases with age for both men and women; one in two women and one in five men over the age of 50 in the UK will suffer a fracture.
Vertebral fractures can result in height loss, intense pain and deformity, however it is hip fractures that are associated with the greatest morbidity and mortality. These latter almost always require surgery, which carries an increased risk of complications and long-term disability, resulting in loss of independence or death (see www.nos.org.uk).
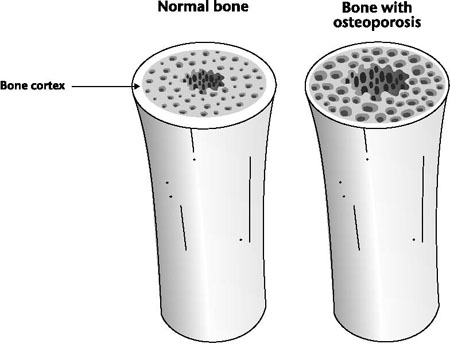
Figure 16.2 Osteoporosis in a bone
Based on current trends, it is predicted that hip fracture rates in the UK will increase from 46,000 in 1985 to 117,000 in 2016. Secondary prevention through early identification and treatment of people at risk of osteoporosis should lead to a reduction in the incidence of major fractures in later life (Dennison et al. 2005; BOA 2007).
4 Identify the risk factors for the development of osteoporosis
A The risk factors in the development of osteoporosis can be broadly divided into two categories (see Table 16.1). Although fixed risks are predetermined and cannot be controlled, there are strategies that can minimize their effect and individuals can take action to reduce the modifiable risks through healthy lifestyle choices.
Table 16.1 Risk factors for the development of osteoporosis (www.iofbonehealth.org)
| Fixed risks | Modifiable risks |
| • Age | • Alcohol |
| • Female gender | • Smoking |
| • Family history of osteoporosis | • Low BMI |
| • Previous fracture | • Poor nutrition |
| • Ethnicity | • Vitamin D deficiency |
| • Menopause/hysterectomy | • Eating disorders |
| • Long-term glucocorticoid therapy | • Insufficient exercise |
| • Rheumatoid arthritis | • Low dietary calcium intake |
| • Primary/secondary hypogonadism in men | • Frequent falls |
In considering the risks in relation to Mrs H, it is evident that her total hysterectomy with bilateral salpingo-oophorectomy resulted in an early menopause (before the age of 45). She was initially prescribed HRT and this would have provided protection for her bones as well as managing the menopausal symptoms, but she stopped taking the HRT after considering the associated risks too great. The recent fragility fracture is also an indicator that she is more likely to sustain another fracture in the future.
5 What effect do bisphosphonates have on bone turnover?
A The treatment of osteoporosis aims to reduce the risk of fracture occurring and can be broadly divided into two categories of drug:
• anti-resorptive agents, which reduce bone resorption;
• anabolic agents, which stimulate bone formation.
Anti-resorptive agents, such as alendronate, inhibit osteoclast activity, slowing down the rate of bone loss. They do this by preventing the osteoclast precursor cells from attaching to the bone and also affect their ability to resorb bone by reducing their metabolic activity. Initially, bone resorption is reduced without affecting bone formation and this results in significant increases in BMD, but this rapid gain slows down over a period of 12–18 months as the resorption-formation coupling mechanisms catch up. The newly formed bone is of normal quality (McDermott et al. 2004; eMC 2012).
Current guidance on the secondary prevention of fragility fractures in post-menopausal women who have osteoporosis and have sustained an osteoporotic fragility fracture recommends treatment with alendronate as it has been shown to reduce the risk of vertebral and hip fractures (NICE 2008). Alendronate can be taken as 10mg tablets daily or 70mg tablets once weekly. The active ingredient is alendronic acid trihydrate and it is available in generic preparations as alendronic acid or branded as ‘Fosamax’. NICE (2008) recommends that the cheapest preparation should be prescribed.
Oral bisphosphonates are very poorly absorbed: less than 5% of the drug is absorbed when taken on an empty stomach and this is further reduced by food, other drugs and liquids (other than water). Of this 5%, about half is deposited in bone and the remainder is rapidly excreted in the urine (Brenner and Stephens 2006).
6 What advice would you give to Mrs H in relation to taking her medication?
A
• Alendronate must be taken at least 30 minutes before the first food or drink of the day. It is important to emphasize this because alendronate will only be effective if taken on an empty stomach. The tablet should be taken with a full glass of plain water, as other fluids (including mineral water), food and some medicines reduce the absorption of the drug (Brenner and Stephens 2006).
• It is necessary to stay upright (sitting, standing or walking) and patients should not take any food or other medications, vitamins or calcium supplements for at least 30 minutes after taking the tablet. These measures will help to minimize the possibility of oesophageal irritation and maximize intestinal absorption of the medication (Greenstein 2009; eMC 2012).
• The most common side-effect associated with oral preparations is GI upset; however, this is reduced with weekly treatment. Mrs H should be advised to report any symptoms of oesophageal irritation such as dysphagia, pain on swallowing, retrosternal pain or new or worsening heartburn to her GP. She should be given the patient information leaflet for osteoporosis and it should be emphasized that failure to follow the instructions may increase the risk of oesophageal problems. Other side-effects include bone, muscle or joint pain. Stress fractures of the femoral shaft have been reported in patients receiving long-term therapy (eMC 2012).
• Bisphosphonates have been linked with reports of osteonecrosis of the jaw (ONJ); however, these cases were generally associated with high-dose IV administration for neoplastic bone disease and were rarely linked with benign bone disease. Mrs H should be advised about the importance of good oral and dental hygiene, be encouraged to visit her dentist for routine checkups and to report any oral symptoms (BNF 2012; eMC 2012).
• More recently there have been links reported with atypical fractures, predominantly occurring in the subtrochanteric region of the femur. Mrs H should be encouraged to report any pain in her hip, thigh or groin to her GP who may consider discontinuing the medication pending further investigation (Rizzoli et al. 2011; BNF 2012; eMC 2012).
• Calcium preparations and antacids should not be taken within two hours of bisphosphonates, as they are known to decrease the bioavailability (Brenner and Stephens 2006). Absorption is also reduced by oral iron preparations (BNF 2012).
• It is common for people with long-term conditions such as osteoporosis to find taking the medication challenging, and consequently only half of these patients will still be taking their medication after one year (see www.iofbonehealth.org). To ensure maximum compliance, adherence and concordance, treatment should have a minimal impact on a patient’s lifestyle and routine, and patients should be empowered and fully involved in the management of their condition (Barber and Robertson 2012). Mrs H’s GP outlined the treatment options and provided her with information on the dosing regimen, the contraindications and the side-effects. Mrs H is an active lady who works full time and following the discussion she opted to take alendronate as a once-weekly tablet. This would allow her to take the tablet at weekends and would not affect her busy morning schedule during the week.
7 What additional advice would you give to Mrs H?
A
• The National Osteoporosis Society is a charity dedicated to the prevention, diagnosis and treatment of osteoporosis and has a network of over 100 support groups across the UK. It runs a helpline staffed by a team of nurses who have specialist knowledge of osteo-porosis and bone health. The charity also produces a wide range of booklets and leaflets for both the general public and health professionals (see www.nos.org.uk). Mrs H may find it useful to contact her local patient support group.
• Mrs H should be encouraged to eat a healthy, balanced calcium-rich diet. The recommended daily requirement for most adults is 700mg of calcium, although people with osteoporosis who are taking drug treatments might benefit from 1000 to 1200mg. Excellent sources of calcium include dairy products, tinned fish and green leafy vegetables (National Osteoporosis Society 2011).
• Vitamin D is vital in the role of calcium absorption and 90% of our requirements are produced through exposure of the skin to sunlight. Mrs H should be advised that she needs about 15 to 20 minutes of sun exposure to the face and arms without sunscreen, three or four times a week, between April and October. This should provide enough vitamin D for the year. Dietary sources of vitamin D include margarine, egg yolks, cod liver oil and oily fish (National Osteoporosis Society 2011).
• Mrs H takes her grandchildren swimming and while this is a healthy exercise choice, it is not weight-bearing and this is a key factor in the maintenance of bone density. Weight-bearing exercise, such as walking, dancing, jogging and tennis, stimulates the thickening of bone, strengthening it and reducing the risk of fracture. Lack of exercise reverses these changes leading to lighter, weaker bones (Waugh and Grant 2006). Mrs H should be advised to engage in weight-bearing exercise at least three times a week for a minimum of 20 minutes. However, her swimming will help to strengthen muscle tone which in turn will improve balance and reduce the risk of falls.
KEY POINTS
• Bone is constantly being remodelled in response to a variety of factors.
• Osteoporosis is a skeletal disorder associated with a reduction in bone density and quality.
• The main cells in bone homeostasis are osteoblasts (bone-building cells), osteocytes (mature bone cells) and osteoclasts (bone-resorbing cells).
• Peak bone mass is achieved at around 35 years of age.
• In women there is a dramatic acceleration of bone loss for several years following the menopause.
• One in two women and one in five men over the age of 50 will suffer a fracture.
• Risk factors in the development of osteoporosis include age, gender, smoking, alcohol intake, diet and exercise.
• Bisphosphonates act by reducing bone resorption, preserving bone mineral density.
• People with osteoporosis should be encouraged to eat a healthy, balanced, calcium-rich diet, take regular weight-bearing exercise, give up smoking and drink alcohol in moderation.
• The National Osteoporosis Society is a charity dedicated to the prevention, diagnosis and treatment of osteoporosis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree