The person with a myocardial infarction
CASE AIMS
After examining this case study the reader should be able to:
• Briefly explain the normal anatomy and physiology of blood vessels.
• Describe the pathophysiology of atherosclerosis.
• Outline why the patient’s gender is an important factor in diagnosing cardiovascular disease.
• Explain the significance of being post-menopausal in terms of myocardial infarction.
• Identify the importance of checking cholesterol levels in the diagnosis of myocardial infarction.
• Demonstrate an understanding of the mode of action and side-effects of tenecteplase in the treatment of myocardial infarction.
• Articulate how specific biomarkers such as troponin I relate to the confirmation of myocardial infarction.
CASE
A 59-year-old woman presented to the A&E department with a four-hour history of increased shortness of breath (dyspnoea), retrosternal chest pain and sudden extreme fatigue/weakness. She has a strong family history of heart disease, herself suffering from atherosclerosis, angina and hypertension. She is post-menopausal. She takes Imdur 60mg once per day and 5mg of amlodopine. She recently had fasting cholesterol levels checked by her GP and the results were: LDLs 4.9mmol/L,HDLs <1.3mmol/L and triglycerides 5.6mmol/L. This gave her a total cholesterol of 6.2mmol/L. Her BMI is 29 and she has a history of very little exercise before being diagnosed with her angina four years ago. She is a non-smoker and admits to having an occasional glass of wine.
2 What is meant by atherosclerosis?
3 Why may the patient’s gender be an important factor in diagnosing the problem?
4 What is significant about the patient being post-menopausal?
5 Why has she had her cholesterol levels checked?
The patient is diagnosed via ECG and patient history with an AMI. She is given 300mg of aspirin(stat) tenecteplase (TNK) with IV heparin running alongside as per trust policy. She is also given 2.5mg of diamorphine, an antiemetic and 100% oxygen. Twelve hours after her initial onset of symptoms she is given a troponin I blood test which returns at 16.0ng/ml (which is significant for indication of MI).
6 What is the mechanism of action of thrombolytic drugs such as tenecteplase?
7 What are the main risks with thrombolytic drugs?
8 How do specific biomarkers such as troponin I relate to the confirmation of MI?
ANSWERS
1 Prior to the patient’s CVD, what would have been the normal anatomy and physiology of her blood vessels?
A Most blood vessels have a similar construction (with the exception of the capillaries). The walls of all blood vessels, arteries and veins are composed of three layers of tissue called tunica. The outer layer, tunica externa (adventitia) is composed of connective tissue, collagen and nerve fibres. It surrounds and supports the vessel with sympathetic nerve fibres that transmit nerve impulses to keep the walls of the vessel in a state of tonus which stops the vessel from collapsing in on itself. The infiltration of sympathetic nerve fibres is increased (vasoconstriction) and allows for dilation of the vessel walls when nerve impulses are decreased (vasodilation). Generally there is more fibrous tissue found in arteries than in veins.
The middle layer is called the tunica media and is made up of vascular smooth muscle supported by a layer of collagen and elastin fibres. The smooth muscle cells that make up this layer produce the vasoconstriction/dilation of the blood vessel by releasing the neurotransmitter norepinephrine which diffuses into the tunica media and acts upon the nearby smooth muscle cells.
The innermost layer is called the tunica intima and consists of a single layer of flattened endothelial cells with little sub-endothelial connective tissue. This layer is smooth to prevent turbulent blood flow (Fawcett 2006). Beneath the tissue is an internal elastic lamina (thin layer) that is well developed in muscular arteries. Endothelial cells form a continuous lining throughout the vascular system called the endothelium. The endothelium plays a role in vascular resistance, control of platelet adhesion and clotting. Capillaries are composed only of endothelial cells with few or no elastic fibres; this aids the rapid exchange of water and solutes between the tissue fluid and blood plasma (Barber et al. 2012).
2 What is meant by atherosclerosis?
A Atherosclerosis is a disease process that affects the large and medium arteries, especially the aorta and the arteries that supply the heart (coronary arteries), brain, kidneys and lower limbs (Woods et al. 2012). As a disease process it is described as a thickening or hardening of the arteries. As it is a progressive disease, and evidence suggests that the disease process starts in childhood, but it may be many years before the effects of poor diet, lack of pertinent exercise, smoking, drinking and lifestyle habits finally show themselves as hypertension, diabetes, obesity and smoking-related disorders which all carry an increased risk of developing coronary heart disease (CHD).
It is under the inner layer of the arteries, the tunica intima, where the progressive disease process of atherosclerosis is most prevalent and where plaque formation is accumulated. This build-up of atherosclerotic plaque is the precursor of many forms of angina and ultimately can, and does, lead to the high incidence of MI in both men and women.
In general, atherosclerosis evolves from deposits of lipids, cellular debris, calcium and fibrin (a clotting factor). Together they unite to initiate a progressive inflammatory component. Although not yet completely understood it is hypothesized to be fundamentally initiated by an inflammatory process in the vessel wall in response to retained LDL molecules. Once the molecules are inside the vessel wall they are suspected of becoming susceptible to oxidation by free radicals and in essence become toxic in nature to the cells. Because of this toxicity the molecules trigger a cascade of immune responses which over time produce an atheroma. The body’s immune system responds by sending specialized white blood cells such as macrophages and T-lymphocytes to absorb the oxidized-LDL forming specialized foam cells, along with a proliferation of arterial smooth muscle cells in an attempt to heal the lesion. However, in their endeavour to process the oxidized-LDL they grow and then rupture, depositing an even greater amount of oxidized cholesterol into the artery wall. This ultimately triggers more white blood cells which perpetuates the cycle. Eventually, the artery becomes inflamed, and the cholesterol plaque causes the muscle cells to enlarge and form a hard cover over the affected area.
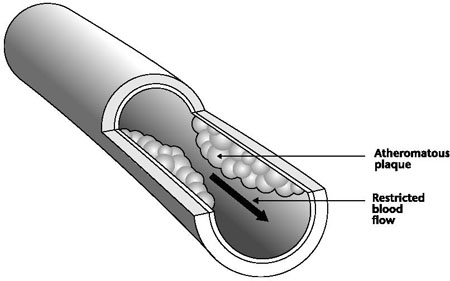
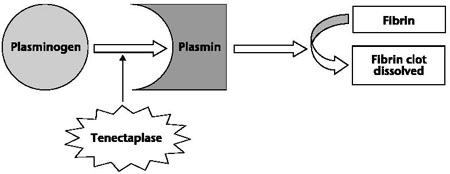
Figure 15.1 The effects of atherosclerosis
This hard cover is what causes a narrowing of the lumen of the artery, reducing the blood flow, which may lead to angina and increases blood pressure. Advanced plaques, which have a fibrous coating and a lipid-rich core, are known to be unstable. Consequently, thrombi form on the plaque surface, which ultimately restricts the lumen of the artery further and is known to produce the symptoms of acute coronary syndrome (Johnson and Rawlings-Anderson 2007).
3 Why may the patient’s gender be an important factor in diagnosing the problem?
A
• Heart disease does not discriminate between the sexes and remains a leading killer of both men and women worldwide. The difference lies in the diagnosis and treatment of women with heart disease which seems to have perpetuated a gender gap.
• According to the British Heart Foundation (2011), CVD is the leading cause of death and disability in women in the UK and accounts for more deaths among women than breast cancer. However, despite these findings, many women still do not identify cardiovascular disease as their greatest health risk.
• Rowlands and Clarke (2007) state that, unlike men, women are less likely to seek medical help and are more likely to present themselves late to A&E with symptoms such as breathlessness, abdominal discomfort and fatigue. This late presentation may well result in delays in diagnosis and receiving effective treatment.
• When a hospital assessment is needed, women are less likely to be treated in coronary care units than men, or even to have ECG and cardiac enzymes measured, and this may be due in part to their ‘atypical’ symptoms.
• In a man, plaque tends to distribute itself in clumps for some reason, whereas women’s plaque is distributed more evenly throughout the artery walls. This can result in women’s angiographic studies as being misinterpreted as ‘normal’. Therefore, women are less likely to receive treatment for their symptoms in line with the evidence-based guidelines for men.
4 What is significant about the patient being post-menopausal?
A
• Up until the menopause a woman is thought to be naturally protected by the presence of the hormone oestrogen, which is responsible for the female secondary sexual characteristics and the development and proper functioning of the female genital organs.
• Oestrogen is known to act on the tunica intima and helps to reduce the disease process of atherosclerosis by minimizing the effects of inflammation on the arteries.
• It is around the time of the menopause that researchers find that many doctors see a clustering of obesity, hypertension and dyslipidaemia in their peri/post-menopausal patients, which also increases the risks for developing CHD (Thompson and Webster 2005).
• Recently there has been further discussion by the British Heart Foundation (2011) to confirm that some researchers worldwide are now not totally convinced that it is solely down to the loss of oestrogen that puts women at greater risk of developing CHD.
• Consideration is also being given to other variables such as ageing, diabetes and psycho-social factors such as depression as significant risk factors. Although this research is in its infancy at present there appear to be far too many unanswered questions to conclude a correlation between these variables and the relationship to CHD in women, and, as such, a reduction in the amount of oestrogen still remains a favourable consideration for the development of CHD.
5 Why has she had her cholesterol levels checked?
A Although elevated cholesterol levels are associated with an increased risk of developing CHD in men and women, total cholesterol levels tend to peak approximately 10 years later in women than in men. Due to this factor a low level of HDL appears to be a better predictor of CHD risk in women, especially older women, compared to LDL levels.
This difference in cholesterol levels may well be attributed to the fact that oestrogen keeps the harmful LDL cholesterol levels lower and HDL levels higher. It also plays a role in keeping the blood vessels dilated. This protective effect is believed to be reduced after the menopause (see above).
6 What is the mechanism of action of thrombolytic drugs such as tenecteplase?
A Thrombolytic drugs such as tenecteplase break down the thrombus so that the blood flow to the heart muscle can be re-established to prevent any further damage; this will also assist in the healing process (NICE 2002).
If heart muscle is compromised or occluded from a rich supply of oxygenated blood then the likelihood of death of the heart muscle (necrosis) becomes increasingly high. For our patient in this scenario her clinical symptoms (typically but not exclusively retrosternal chest pain/discomfort) and characteristic changes in her 12-lead ECG (with ST segment elevation) have provided the most immediate indication of the diagnosis of AMI which, in the absence of contraindications for this patient, requires thrombolysis as per hospital trust policy.
Tenecteplase is a relatively new type of thrombolytic drug introduced in 2001. It is considered a modified form of plasminogen activator and can be given by rapid IV bolus injection rather than by infusion (BNF 2012). Its timing is crucial in determining the extent of beneficial achievement and has a window of opportunity of up to 12 hours from the first onset of symptoms.
Figure 15.2 The mechanism of action of tenectaplase
Although not completely verified it is thought that tenecteplase binds to fibrin (the insoluble matrix on which a blood clot is formed) and converts plasminogen (a precursor of plasmin) to plasmin, which breaks down fibrin clots when healing is complete. In the presence of fibrin, tenecteplase conversion of plasminogen to plasmin is increased relative to its conversion in the absence of fibrin. Ultimately this decreases systemic activation of plasminogen and the resulting degradation of circulating fibrinogen. In essence its action is to break down the clot by interfering with the body’s natural clotting cascade (Khan 2007).
Alongside tenecteplase, heparin (an anticoagulant) is given, usually as an IV bolus injection before thrombolysis, followed by IV infusion. When given alongside tenecteplase the heparin dose is weight-adjusted. It is also recommended that aspirin 300mg (chewable) is given at the same or around the same time as any thrombolytic drug as the benefit of aspirin is that it works on platelet aggregation.
7 What are the main risks with thrombolytic drugs?
A Bleeding complications are the main risk that is associated with thrombolytic drugs. The most important of these is the complication due to haemorrhagic stroke which occurs in 0.5–1.0% of patients and carries an associated risk of high mortality and long-term disability in survivors. The risk of a haemorrhagic stroke following the use of thrombolytic drugs increases with a patient’s age and blood pressure. Strict guidelines and protocols exist which highlight important contraindications to the giving of this drug in patients with a recent history of any type of:
• haemorrhage;
• trauma;
• surgery;
• acute cerebrovascular events.
As with any drug that has the potential to cause haemorrhage, thrombolytic drugs should be stopped immediately if the patient displays any signs or symptoms of severe bleeding or stroke-type symptoms (BNF 2012).
8 How do specific biomarkers such as troponin I relate to the confirmation of MI?
A
• Troponin I and T are structural components of cardiac muscle. They are released directly into the bloodstream with a myocardial injury.
• Troponins will begin to increase following MI within 3 to 12 hours.
• Troponin I, as a diagnostic marker, is taken at its peak time of 12 hours after initial chest pain/discomfort.
• Patients that arrive in hospital after the 12-hour window of opportunity can still be given the test but may very well miss out on being given a clot-busting drug such as tenecteplase as these drugs are shown to be most effective in their management of clot busting within the 12-hour window.
• Troponins will also remain elevated from 5 to 10 days for troponin I and up to two weeks for troponin T. This fact alone makes them a superior marker for diagnosing MI.
• The disadvantage of this continued elevation is that this particular diagnostic marker makes it more difficult to diagnose re-infarction or extension of infarction in a patient who has already suffered an initial MI (Saenger and Jaffe 2007).
KEY POINTS
• Heart disease does not discriminate between the sexes and remains a leading killer of both men and women worldwide.
• CHD accounts for more deaths among women than breast cancer.
• Women are more likely to present themselves late to A&E with ‘atypical’ symptoms of a suspected MI.
• Women are less likely to receive treatment for their symptoms in line with evidence-based guidelines for men.
• Up until the menopause, women are thought to be naturally protected from CHD by the presence of the hormone oestrogen.
• Recently new research looked at the links to variables such as age, diabetes, depression and psychosocial factors in the development of MI in women.
• It is under the inner layer of the tunica intima where the progressive disease process of atherosclerosis is most prevalent and where plaque formation is accumulated.
• In general, atherosclerosis evolves from deposits of lipids, cellular debris, calcium and fibrin.
• Plaque in a man tends to distribute itself in clumps whereas women’s plaque is distributed more evenly throughout the artery walls.
• Although elevated cholesterol levels are associated with an increased risk of developing CHD in men and women, total cholesterol levels tend to peak approximately 10 years later in women than in men.
• Thrombolytic drugs such as tenecteplase break down the thrombus so that the blood flow to heart muscle can be re-established.
• Bleeding complications are the main risk factors that are associated with thrombolytic drugs.
• Troponin I and T are highly specific markers for confirmation of myocardial injury.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree