The young person with meningitis
CASE AIMS
After examining this case study the reader should be able to:
• Briefly explain the presenting symptoms of meningitis.
• List the possible causes of meningitis.
• Demonstrate an understanding of the mode of action and reasons for giving penicillin in meningitis.
• With reference to pathophysiology, explain the signs and symptoms of meningococcal meningitis and septicaemia.
• Argue the pros and cons of carrying out a lumbar puncture as an aid to diagnosis.
• Outline the focus of treatment in meningococcal septicaemia in a young person.
• Explain the implications of using intravenous fluids and antibiotics to treat septicaemic shock.
• Explain why meningitis and meningococcal meningitis are notifiable diseases.
• Demonstrate an understanding of why rifampacin would be given to the family of a patient diagnosed as having meningococcal meningitis.
CASE
Fifteen-year-old Mohammed visited his GP at 9 a.m. accompanied by his mother. Mohammed reported that he had been ill since last night; he had vomited his breakfast, but was now drinking water. He felt hot, his head was pounding and he was tired. The GP’s observations were: temperature 38°C, pulse 75, blood pressure 110/80, respiratory rate 20 and oxygen saturations of 97% in air. The GP could not find a cause for the febrile illness and advised Mohammed to take ibuprofen every four hours. He arranged to call him at home after surgery. He also advised Mohammed’s mother to contact the surgery if Mohammed appeared to get any more agitated or drowsy, or if a rash appeared.
Later that afternoon Mohammed’s mother phoned the GP as she was concerned that her son had continued to vomit and was becoming more irritable and had a rash that was spreading. The GP visited and noted his temperature 39°C, pulse 80, blood pressure 100/60 and respiratory rate 20. The patient’s oxygen saturation was 95% in air and there was a capillary refill <2 seconds. Mohammed was becoming drowsier, had a petechial rash, but showed no signs of neck stiffness or photophobia. Bacterial meningitis was suspected. Benzyl penicillin was administered prior to Mohammed being taken to hospital.
1 What presenting symptoms have prompted the GP’s advice?
2 What causes meningitis?
3 Why was penicillin administered and how does it work?
On admission to A&E Mohammed had a non-blanching rash. Meningococcal meningitis was suspected. His observations had deteriorated (temperature 39°C, pulse 85, blood pressure 100/80, respiratory rate 25). His oxygen saturation was 93% in air and capillary refill was sluggish, but still <2 seconds. He was becoming drowsier with no signs of neck stiffness or photophobia. He was complaining that his legs hurt and he felt cold. A lumbar puncture was not performed. Antibiotics and an IV infusion of 0.9% sodium chloride were commenced. Mohammed’s close family were given rifampicin.
4 With reference to pathophysiology, explain the signs and symptoms of meningococcal meningitis and septicaemia
5 How could a lumbar puncture have aided diagnosis?
6 Why was a lumbar puncture not performed?
7 What is the focus of treatment in meningococcal septicaemia in a young person?
8 Explain the implications of using IV fluids and antibiotics to treat septicaemic shock
9 Why are meningitis and meningococcal meningitis notifiable diseases?
10 Why was rifampicin given and how does it work?
ANSWERS
1 What presenting symptoms have prompted the GP’s advice?
A Mohammed presents with a non-specific febrile illness which may indicate the early stage (prodromal phase) of meningitis or septicaemia. Young people with bacterial meningitis commonly present with non-specific symptoms and signs such as:
• vomiting;
• irritability;
• upper respiratory tract symptoms.
It is often impossible to distinguish a milder self-limiting illness from meningococcal meningitis in the prodromal phase (NICE 2010).
Meningitis is a rapidly evolving illness, requiring urgent treatment. A study found that 50% of young people who presented with early signs can then go on to develop later neurological symptoms of meningitis (neck stiffness and photophobia) 12 to 15 hours from onset (Thompson et al. 2006).
Those with more fulminant illness will be critically ill within the first 24 hours, leaving a very narrow window of opportunity to deliver life-saving treatment. Early intervention is indicated. Signs of deterioration such as becoming more agitated (meningeal irritation) and a rash that does not blanch when pressed using a glass (petechiae indicating intradermal haemorrhage) can be indications of meningococcal meningitis and/or septicaemia.
2 What causes meningitis?
A Meningitis can be caused by infection of bacteria, fungus or virus and is classified according to the causative agents. Bacterial meningitis can be caused by:
• pneumococcal species;
• Haemophilus influenzae;
• staphylococcal species;
• meningococcal species.
Meningococcal infection is the most common cause of bacterial meningitis in the UK and Ireland. There are several strains of meningococcal bacteria, but with the development of the MenC vaccine, 85% of cases are caused by MenB infection. Meningococcal bacteria (Neisseria meningitidis) can cause meningitis or septicaemia (blood poisoning), or a combination of these diseases, known as meningococcal disease.
3 Why was penicillin administered and how does it work?
A The NICE guidelines (2010) recommend the administration of benzyl penicillin pre-hospital (or ceftriaxone if allergic to penicillin) in the presence of signs of meningococcal septicaemia. Penicillin is the drug of choice to treat meningococcal meningitis. Although it does not normally pass the blood–brain barrier, it can readily penetrate when the meninges are acutely inflamed. There is no clear evidence to indicate that early penicillin treatment improves outcomes, but it is the best current advice. However, early diagnosis and intervention are necessary to reduce mortality (Todar 2006).
Penicillin is bactericidal and has its effect by damaging and penetrating the cell wall of bacteria, thus killing the bacteria cells. A large component of all bacterial walls is a substance known as peptidoglycan. Bacteria are constantly rebuilding their cell walls (peptidoglycan synthesis), which is how they protect themselves and maintain their structure.
Peptidoglycan is principally made from two sugar molecules; N-acetylglucosamine (NAG) and N-acetylemuramic acid (NAM). Bacteria synthesize long, linear chains of these two sugars, alternating between a NAG and a NAM. Attached to each NAM, however, is a chain of a few amino acids (oligopeptide). To complete the structure of peptidoglycan, these oligopeptides are cross-linked to a neighbouring chain’s oligopeptides to form a strong mesh.
Penicillins irreversibly bind to the bacterial enzyme transpeptidase (penicillin-binding protein) that cross-links these chains. This binding deactivates the enzyme, and so no cross-linking of the ‘amino sugar’ chains can take place, thus weakening the cell wall mesh and bacteria structure. Bacteria can build a resistance to the antibiotic by making β-lactamase, which defends the bacterial walls. This defence can be counteracted by combining the penicillin with β-lactamase inhibitors (BNF 2012).
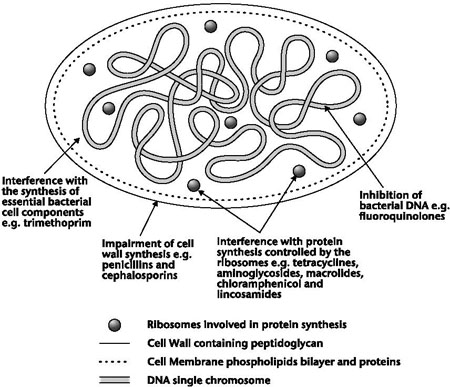
Figure 14.1 Simplified diagram of a bacterial cell and actions of antibiotic drugs
4 With reference to pathophysiology, explain the signs and symptoms of meningococcal meningitis and septicaemia
A SYSTEMIC PRESENTATION
The clinical features of meningitis are a reflection of the underlying pathophysiology. Early clinical features of bacterial meningitis are non-specific and include:
• fever;
• malaise;
• headache.
The major pathophysiological event in meningococcal septicaemia relates to a change in the functions of the microvasculature. The vascular endothelial surface is a highly specialized organ, regulating vascular permeability and presenting a thrombo-resistant, non-reactive surface to circulating blood cells. The highly specialized properties affected during the inflammatory process result in:
• increased vascular permeability;
• pathological vasoconstriction and vasodilatation;
• loss of intravascular coagulation;
• myocardial dysfunction leading to shock and multi-organ failure as a result of the vascular permeability;
• hypovolemia and shock.
The permeability is caused by bacterial components, such as endotoxins released from the bacterial cell wall, and is indirectly caused by the activation of inflammatory cells and stimulation of the immune system by proinflammatory cytokines. The capillary leak is the most important clinical event, but the underlying pathophysiology is unclear. Some evidence suggests that meningococci and neutrophils cause the loss of negatively charged glycosaminoglycans that are normally present on the endothelium. Albumin is normally confined to the vasculature because of its large size and negative charge, which repels the endothelial negative charge. The repulsive effect of albumin may be reduced in meningococcal infection, which allows the protein leak. The inflammatory process induced by meningococci results in a change in the permeability properties of the endothelium in all vascular beds.
From presentation until two to four days after the onset of illness:
• vascular permeability massively increases;
• albumin and other plasma proteins leak into the intravascular space and urine (proteinuria), causing severe hypovolemia;
• loss of proteins is followed by loss of fluid and electrolytes that leads to hypovolemia;
• loss of circulating plasma is initially compensated for by homoeostatic mechanisms, including vasoconstriction of both arterial and venous vascular beds.
However, as the capillary leak progresses, venous return to the heart is impaired and the cardiac output (heart rate) falls notably.
As compensatory vasoconstriction is an early protective mechanism to maintain tissue and organ perfusion in the face of diminished cardiac output, most patients with meningococcal septic shock have evidence of intense vasoconstriction. This presents as cold peripheries and sluggish blood flows to the tissues.
Although vasoconstriction is primarily protective, the constriction may persist even after resuscitation and measures to improve cardiac output. This can lead to patients developing cold, pale, and ischemic limbs due to disordered coagulation (Pathan et al. 2003).
Examination of the skin may reveal petechiae indicating haemorrhage and increased vascular permeability that are suggestive of, but not exclusive to, meningococcal infection (Hoffman and Webber 2009). One of the most dramatic features of severe meningococcal sepsis is the occurrence of widespread purpura fulminans, a cutaneous thrombotic disorder usually caused by autoimmune-mediated protein deficiency. This disorder typically presents with petechiae that eventually slowly or rapidly coalesce into extensive, necrotic eschars on the extremities. This severe intravascular thrombosis occurs in the presence of thrombocytopenia and prolonged coagulation as meningococcal infection affects the pathways of coagulation. Also, due to endothelial injury, there are platelet-release reactions which, together with the stagnant circulation due to vasoconstriction, cause platelet plugs to form and start the process of intravascular thrombosis.
CENTRAL NERVOUS PRESENTATION
Later on, the following symptoms develop as signs of meningeal irritation (Van de Beek et al. 2004):
• meningismus (neck stiffness);
• photophobia;
• vomiting.
Once the blood–brain barrier is breached, an inflammatory response within the cerebrospinal fluid occurs as follows.
• The inflammation of the meninges causes an activation of the trigeminal sensory nerve fibres and can also elicit a protective reflex to prevent stretching of the inflamed and hypersensitive nerve roots, which is seen clinically as neck stiffness.
• If the inflammatory process progresses to cerebral vasculitis or causes cerebral oedema and elevated intracranial pressure, then alterations in mental status, vomiting, seizures and cranial nerve palsies may be observed. The nerve palsies affect the ability of the pupil of the eye to respond to changes in environmental light and create weakness in the extremities.
• Patients who present with the clinical features of raised intracranial pressure, caused by meningitis, are at risk of cerebral infarction if perfusion is not improved.
5 How could a lumbar puncture have aided diagnosis?
A A lumbar puncture (or spinal tap) is a way to collect CSF and bacteria in the CSF is usually the way to diagnose meningitis. The CSF in bacterial meningitis is characterized by a strongly elevated white blood cell count (<500 cells/μl) with predominant neutrophils and a strongly elevated protein (<1g/L), indicating severe blood-CSF barrier disruption, increased lactate (<0.3g/L) and decreased glucose CSF/blood ratio (>0.4).
6 Why was a lumbar puncture not performed?
A
• A lumbar puncture remains controversial where there are contraindications (Pollard et al. 1999). The procedure is contraindicated in the face of widespread purpura, severe coagulopathy, cerebral herniation or cardiovascular shock.
• A lumbar puncture is not usually performed where it will add little to the diagnosis, such as in clear-cut cases with fever and generalized purpura, or where it may lead to significant deterioration in those already seriously ill, or may delay treatment.
• Symptoms and signs of cerebral herniation (signs of fluctuating or impaired levels of consciousness) occur in 4–6% of children with bacterial meningitis and this complication accounts for 30% of deaths from the condition (Riordan and Cant 2002). Cerebral herniation can occur when a lumbar puncture has not been performed, but a there is a temporal association between lumbar puncture and herniation. Thus, delaying a lumbar puncture when there are signs and symptoms of herniation may be lifesaving.
Mohammed had no obvious signs of meningeal irritation (neck stiffness or photophobia), but this is not a good indicator of meningitis in young people as they can remain alert and the signs may be non-specific and absent. What was more important was that Mohammed had signs of shock – a sluggish capillary refill time even though it was above the threshold of >2 seconds; cold hands and feet and falling oxygen saturation. He also had some early signs of raised intracranial pressure as he was drowsy, indicating a decreasing conscious level. The purpuric-type rash was also a sign of coagulopathy.
7 What is the focus of treatment in meningococcal septicaemia in a young person?
A The focus of treatment is to identify signs of raised intracranial pressure or shock and treat the young person based on those findings. Meningococcal meningitis generally has a better prognosis than septicaemia; however, death can occur due to the severity of the inflammatory process within the brain. It is crucial to remember that the underlying meningitis and septicaemia may be very advanced by the time a rash appears. The rapidly evolving haemorrhagic rash can be a very late sign and in some cases it may be too late to save the child’s life by the time this rash is seen. Although some of the causes of petechial rashes are self-limiting conditions, many others, including meningococcal disease, are fulminant purpura and life-threatening. So a non-blanching rash should therefore be treated as an emergency.
8 Explain the implications of using IV fluids and antibiotics to treat septicaemic shock
A Restoration of circulation volume is the most important component of resuscitation for shock and early treatment with an IV antibiotic such as ceftriaxone, a bactericidal cephalosporin, is essential. Cephalosporins are structurally similar and work in similar ways to penicillins by blocking the construction of the bacterial cell wall (Han et al. 2003). After being absorbed, cephalosporins are widely distributed in the tissues of the body. Some can actually cross over the blood–brain barrier – for example, ceftriaxone. This drug is therefore useful for infections in the CNS, such as bacterial meningitis.
Circulation volume is improved through IV fluids. Mohammed is prescribed isotonic fluids initially. The properties of an IV solution are created by the specific materials it contains. Crystalloid solutions are the primary fluids used to correct dehydration and contain electrolytes (e.g. sodium, potassium, calcium, chloride) but lack the large proteins and molecules found in colloids such as plasma albumin. Isotonic crystalloids (iso – same; tonic – concentration) have an electrolyte tonicity equal to the body plasma. When administered to a normally hydrated patient, isotonic crystalloids do not facilitate osmosis so there is no significant shift of water between the cells and the intravascular space (circulation). However, fluid replacement has to be managed carefully in meningococcal septicaemia due to vascular permeability. There is also a risk of increasing oedema within all tissues and organs as a result of persistent capillary leak. Pulmonary oedema and respiratory failure are direct consequences of the gross increase in vascular permeability.
To improve circulating volumes in shock, colloid solutions may also be prescribed. A colloid solution contains solutes as large proteins or other similarly sized molecules. The proteins and molecules are so large that they cannot pass through the cell walls of the capillaries and can significantly increase the intravascular volume (volume of blood). Colloid solutions facilitate movement of water into the circulation which may be beneficial in the short term, but continual movement can cause dehydration (Corbett and Brodie 2007).
9 Why are meningitis and meningococcal meningitis notifiable diseases?
A Meningococcal disease is contracted through association with infected individuals, as evidenced by the 500- to 800-fold greater attack rate among household contacts than among the general population. Notification to the Health Protection Agency (HPA) is a legal requirement and acts as a trigger for public health actions to be put into place to protect other people from that disease (HPA 2010).
10 Why was rifampicin given and how does it work?
A The risk to contacts is low. Although meningococcal disease is infectious, 97% of cases are isolated, with no links to any other cases. However, people who live in the same household as someone with meningococcal disease, along with intimate kissing contacts (boy/girlfriends) are more at risk than others. For this reason, such people are given rifampicin tablets or syrup. Usually, family members who accompany the patient to hospital will receive antibiotics there. The local public health doctor then has the job of making sure that any other household or intimate contacts receive antibiotics, and usually also tells the nursery or school the patient attends that there has been a case. There is no need to give antibiotics to a wider range of contacts, such as classmates, unless there has been more than one case within a short period of time. The public health doctor follows national guidelines when deciding what needs to be done to protect the community.
Rifampicin works by targeting and inactivating a bacterial enzyme called RNA-polymerase. The bacteria use RNA-polymerase to make essential proteins and to copy their own genetic information (DNA). Without this enzyme the bacteria cannot reproduce. It is important to remember that rifampicin kills the bacteria that live in the nose and throat, but cannot prevent illness in someone who is already incubating the germs. So even if a person is given anti-biotics, it is still important they look out for the signs and symptoms of septicaemia and meningitis.
KEY POINTS
• It is often impossible to distinguish someone who has a milder self-limiting illness from someone with the early stages of meningococcal meningitis (prodromal phase).
• Bacterial meningitis is an infection of the surface of the brain (meninges). In young people the most frequent cause is Neisseria meningitidis (meningococcus) bacteria.
• Once the blood–brain barrier is breached, the inflammatory response of the meninges causes an activation of the trigeminal sensory nerve fibres, eliciting a protective reflex to prevent stretching of the inflamed and hypersensitive nerve roots. This is seen clinically as neck stiffness.
• Progressive inflammatory processes can lead to cerebral vasculitis, cerebral oedema and elevated intracranial pressure. This presents as alterations in mental status, vomiting and seizures, and causes cranial nerve palsies.
• A raised white cell count in the CSF is usually the way to diagnose bacterial meningitis, but a lumbar puncture is contraindicated when the individual exhibits signs of shock.
• Restoration of circulation volume is the most important component of resuscitation for septicaemic shock.
• Meningitis is a communicable disease so all who have a high risk of contracting it are offered a preventative antibiotic (chemoprophylactic agent).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


