The person with hypertension
CASE AIMS
After examining this case study the reader should be able to:
• Explain why blood pressure is important in the normal circulation of blood.
• Outline how the body normally regulates blood pressure.
• Identify the risk factors involved in the development of hypertension.
• Discuss the importance of waist/hip ratio and lipid profile in the diagnosis of hypertension.
• Demonstrate an understanding of the mode of action and side-effects of angiotensin-converting enzyme inhibitors.
• Discuss the role of the nurse in advising relatives regarding taking angiotensin-converting enzyme inhibitors.
• Demonstrate an understanding of the mode of action and side-effects of statins.
• Discuss the role of the nurse in advising relatives regarding taking statins.
CASE
Mr J is a 55-year-old man who presented to his GP with elevated blood pressure, which had been monitored by the practice nurse for the preceding three months. A mean score of 185/95mmHg had been recorded at varying times of the day.
1 Why is blood pressure important to Mr J’s circulatory system?
2 How does Mr J’s body normally regulate his blood pressure?
Mr J has a BMI of >32 and is clinically described as obese. He is a type 2 diabetic with elevated low density lipoprotein (LDL) cholesterol levels (4.90mmol/L), reduced high density lipoprotein (HDL) cholesterol (1.034 mmol/L) and triglycerides (5.645mmol/L). His total cholesterol is 6.19mmol/L. He has a waist circumference of 50in (127cms), is a current smoker of 25 years and drinks above the recommended 21 units per week for a male. He takes no exercise and his diet remains high in fat.
3 What risk factors are involved in the development of hypertension?
4 Why does the doctor want to know Mr J’s BMI, waist/hip ratio and lipid profile?
Mr J’s GP starts him on the angiotensin-converting enzyme (ACE) inhibitor perindopril 10mg and atorvastatin 10mg (a lipid-lowering drug). He immediately recommends lifestyle changes. Mr J also has bloods taken for liver function tests (LFTs) and U&Es. He is advised to return to the surgery in one week for the results of his blood test and a blood pressure check.
5 Describe the mechanism of action and side-effects of ACE inhibitors
6 What advice would you give to Mr J about his ACE inhibitor?
7 Explain the action of Mr J’s lipid-lowering drug
8 What advice would you give Mr J about his lipid-lowering drug?
ANSWERS
1 Why is blood pressure important to Mr J’s circulatory system?
A Blood circulates due to the heart pump establishing a pressure gradient. Blood pressure is determined largely by the hydrostatic (water) pressure which is exerted by the blood on the walls of blood vessels. The heart is actually two pumps. The left side is responsible for exerting strong pressure within the left ventricle to push blood forward through the aorta into the systemic system. The highest average pressure, created in the left ventricle, is observed in the aortic arch before the coronary branches, and measures approximately 95mmHg.
The right side of the heart, where deoxygenated blood is returning to the lungs, is at a much lower pressure. The average lowest pressure is at the junction of the superior and inferior vena cava as it returns to the right atrium, where it is about 3–5mmHg. Blood circulates in these two systems. The rate of flow is dependent upon arterial blood pressure and the peripheral resistance (opposition to blood flow) provided by blood vessels and blood viscosity (stickiness of blood).
The flow rate of any fluid is proportional to the pressure applied to that fluid, and, as such, fluid flows from high pressure to low pressure regions. The greater the pressure differential, the faster the movement of the fluid. However, flow will only continue if the pressure exceeds the opposing forces of resistance. The rate of flow is inversely proportional to the resistance – since for a given pressure, the higher the resistance, the lower the flow rate (Clancy and McVicar 2009).
The blood vessels are responsible for delivering blood flow from the heart to the cellular level following a direct sequence, as follows.
• The arteries that carry blood away from the heart and towards the tissues, while the heart ventricles pump blood into the aorta (systemic system) and the pulmonary artery (bringing deoxygenated blood back to the lungs for reoxygenation).
• The arterioles, smaller subdivisions of the arteries, carry blood into the capillaries – tiny, thin-walled vessels that allow for gaseous exchanges between the two systems.
• The capillaries then unite the arterioles with the venules – small vessels that receive blood from the capillaries and begin the transportation of deoxygenated blood back to the veins.
• The veins are formed at the merger of the venules. Ultimately their role is to return deoxygenated blood to the right side of the heart (Cohen 2012).
2 How does Mr J’s body normally regulate his blood pressure?
A
• Among the factors that affect blood pressure is the total blood volume available. On average, a 70kg healthy man has approximately 5L of blood in his body. This equates to 20% circulating volume for each litre respectfully. Should a loss of volume occur (through haemorrhage, for example), blood pressure will drop. Other considerations are:
• heart rate;
• stroke volume (the volume of blood ejected from the ventricle with each beat of the heart);
• blood vessel compliance;
• blood vessel elasticity;
• resistance to blood flow (Watson 2003).
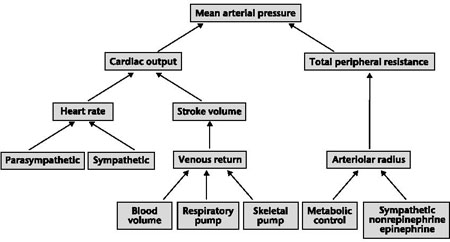
Figure 12.1 Summary of factors that affect mean arterial pressure
THE RENIN–ANGIOTENSIN SYSTEM
The renin–angiotensin system is the most important of the endocrine systems controlling blood pressure, and works in the following way.
• The kidneys’ juxtaglomerular apparatus secretes renin (an enzyme that is released in response to low serum sodium or low blood pressure).
• Renin activates the inactive plasma protein angiotensinogen to produce angiotensin I (still a physiologically inactive substance).
• This in turn is rapidly converted into angiotensin II in the lungs by ACE.
• Angiotensin II is a potent vasoconstrictor and, as such, causes a rise in blood pressure. It also stimulates the release of aldosterone from the adrenal glomerulosa, which results in both sodium and water retention. These chemical reactions are in a direct response to either reduced glomerular under-perfusion or a reduced salt intake (Thibodeau and Patton 2007).
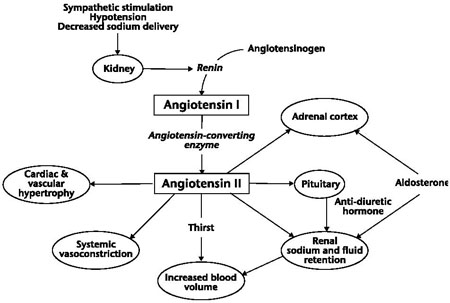
Figure 12.2 The renin-anglotensinogen cycle
3 What risk factors are involved in the development of hypertension?
A There are a number of risk factors that can contribute to hypertension. They fall into two categories: modifiable (risks a person can change) and non-modifiable (risks a person cannot change). Factors that are modifiable include smoking, raised cholesterol, diabetes, obesity, stress, lack of exercise, diet (especially consuming larger than average amounts of salt) and alcohol consumption. As we can see from this list, Mr J has seven of the risk factors within his medical profile. Non-modifiable factors include racial background (Afro-American people are more likely to get hypertension in comparison with Caucasians), age, gender (more men get hypertension than women) and inherited genetic factors such as hyperlipidaemia (high cholesterol level) (DH 2000; Noble et al. 2005).
4 Why does the doctor want to know Mr J’s BMI, waist/hip ratio and lipid profile?
A BMI
The development of obesity is an independent risk factor for developing diseases such as hypertension, raised blood cholesterol and type 2 diabetes. The management and control of the increase in obese and overweight people is indirectly costing the UK approximately £2 billion per year. To try to control the spiralling costs of caring for obese and overweight patients it has become important to identify individuals who may present as a risk of developing complications of obesity and potential diseases such as hypertension by assessing a person’s BMI (kg/m2) (DH 2000). This has become an internationally accepted numerical range to define degrees of obesity in Caucasians.
WAIST/HIP RATIO
Although widely used and accepted as a risk assessment tool, BMI is not a particularly good indicator of the development of cardiovascular disease and an alternative measure is the waist/hip ratio. As waist size increases in comparison with the hip measurement there is a greater chance of developing hypertension, diabetes, MI and strokes due to the increased laying down of adipose tissue around the abdominal organs as visceral fat. Doctors are claiming that men with a waist size above 40in (102cm) and women with a waist size above 35in (89cm) can quadruple their risk of developing obesity-related diseases (Kaplan and Victor 2010).
LIPID PROFILE
Lipids are a group of naturally occurring organic molecules that do not dissolve in water. Although the term ‘lipid’ is used interchangeably with the term ‘fat’, a fat is a lipid but a lipid is not necessarily a fat. The body uses lipids as a source of energy to produce hormones, absorb fat-soluble vitamins and to provide structure to cell membranes. Generally we talk about two main types of lipoproteins: HDLs and LDLs.
HDLs are the smallest of the lipoprotein particles and the densest as they contain the highest proportion of protein to cholesterol. This is why they are regarded as ‘good fats’. HDLs are capable of picking up cholesterol from cells by interaction with adenosine triphosphate and delivering it to the liver where it is excreted in bile. Ultimately bile goes to the intestines, either directly or indirectly, after conversion into bile acids. The delivery of HDL cholesterol is an important synthesis for the adrenals, ovaries, testes and for the synthesis of steroid hormones such as glucocorticoids.
HDL cholesterol and its lipid and protein constituents is a vital component in inhibiting oxidation, inflammation, activation of endothelium coagulation and platelet aggregation. HDL cholesterol is therefore to remove cholesterol from the body and thus reduce the risk of the development of atherosclerosis of the arteries (NICE 2011).
LDLs have a similar mechanism. They also transport cholesterol around the body but deliver it to the artery walls, where it is retained and attracts macrophages that engulf the LDL particles and begin the formation of plaque (build up of fatty deposits), which increases the likelihood of developing atherosclerosis over time.
Diabetic patients, like Mr J, have an increased risk of the development of atherosclerosis due to the action of insulin resistance from an increased amount of adipose tissue. If the build-up of plaque over time eventually ruptures this activates the blood clotting process which leads to either arterial stenosis (narrowing of the lumen) or total occlusion of the vessel. Ultimately this can lead to heart attacks, stroke or peripheral vascular disease. With the development of atherosclerosis the walls of the lumen of the arteries become stiff (hardening of the arteries) which in turn forces the heart to pump past this vascular resistance to deliver blood around the body (Jowett and Thompson 2007).
5 Describe the mechanism of action and side-effects of ACE inhibitors
A MECHANISM
These drugs work by preventing the activation of the hormone angiotensin II from its precursors, renin and angiotensin I. As angiotensin II is a powerful vasoconstrictor, ACE inhibitors open up blood vessels resulting in a lowering of blood pressure. Their mechanism of action not only helps to reduce blood pressure but also protects the kidneys of people with diabetes and hypertension.
ACE inhibitors are a first-choice antihypertensive treatment in diabetes, unless contraindicated. They prevent renal absorption of sodium by lowering the production of aldosterone, which ultimately has a diuretic effect, causing sodium loss and potassium retention. The ACE inhibitors group includes all the ‘prils’ – for example, captopril, enalapril, lisinopril and ramipril (NICE 2011; BNF 2012).
SIDE-EFFECTS
Although ACE inhibitors are very effective in their treatment of blood pressure the initial taking of this medication can cause a sudden fall in blood pressure. Therefore patients are advised to monitor their blood pressure initially. ACE inhibitors can cause a dry, irritating cough (especially at night) which can affect sleep. A newer class of ACE inhibitors was introduced in 1995 called angiotensin receptor blockers (ARBs). These drugs work by blocking the angiotensin II receptors, and for this reason they have a more specific effect on blood pressure, and do not cause the irritating dry cough. ARBs are the ‘artans’ – for example, candesartan, irbesartan, losartan and valsartan. This group of drugs is often used if there is an intolerance to ACE inhibitors, but may be prescribed in addition to ACE inhibitors in heart failure (Richards 2009; NICE 2011).
6 What advice would you give to Mr J about his ACE inhibitor?
A
• You should first ascertain that Mr J does not have an allergy or hypersensitivity to this class of drugs as this carries the risk of anaphylaxis (possible with almost any drug).
• You need to know if Mr J has any renal artery stenosis as these drugs reduce the glomerular filtration rate and may cause progressive renal failure.
• It is important for Mr J to be aware of any potential side-effects, most likely to be a persistent dry cough in about 10–20% of users.
• You can advise Mr J that ACE inhibitors can be replaced with ARBs if he suffers from the cough.
• Mr J is drinking over the recommended amount of alcohol each week for a man, so you need to give him information regarding the fact that alcohol also acts as a diuretic. The combination of ACE inhibitor and alcohol can in some cases lead to hypotension (low blood pressure) (Jordan 2009; BNF 2012).
7 Explain the action of Mr J’s lipid-lowering drug
A
• Lipid-lowering drugs are referred to as ‘statins’ and include atorvastatin, fluvastatin, pra-vastatin, rosuvastatin and simvastatin.
• Statins are the first-choice drug for lowering cholesterol levels.
• They act by reducing the formation of lipids or hastening their removal from the body.
• Evidence suggests that taking statins lowers the harmful LDLs and raises the protective HDLs.
• Statins work by inhibiting an important enzyme needed by the liver in the synthesis of cholesterol, known as hydroxymethylglutaryl coenzyme A reductase (HMG CoA reductase). If this enzyme is inhibited, the cells in the liver will reduce their manufacture of cholesterol. This leads to an increase of LDL receptor sites on cell surfaces as there is less cholesterol available to them. This has an added benefit as additional receptor sites further increase the removal of LDLs from the bloodstream.
• Mr J has been prescribed atorvastatin which, apart from lowering blood cholesterol, is also responsible for stabilizing plaque and helping to prevent strokes through anti-inflammatory mechanisms.
8 What advice would you give Mr J about his lipid-lowering drug?
A
• Mr J should be advised to refrain from eating grapefruit or drinking grapefruit juice, as there is a chemical in grapefruit that can increase the level of the statin in the bloodstream, thus increasing the risk of side-effects.
• It is important to advise Mr J that he needs to inform his GP if he develops any sudden shortness of breath or a cough, as, although rare, statins can cause interstitial lung disease.
KEY POINTS
• Blood pressure is determined largely by hydrostatic (water) pressure which is exerted by the blood on the walls of blood vessels.
• The renin–angiotensin system is considered the most important of the endocrine systems controlling blood pressure.
• Risk factors for developing hypertension fall into two categories: modifiable and non-modifiable.
• Although widely used as a risk assessment tool, BMI is now considered a less effective indicator for cardiovascular disease than waist/hip ratio.
• ACE inhibitors work by opening up blood vessels (vasodilation), resulting in the lowering of blood pressure.
• Lipid-lowering drugs (statins) act by reducing the formation of lipids or hastening their removal from the body.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


