The person with epilepsy
CASE AIMS
After examining this case study the reader should be able to:
• Briefly explain the normal mechanism that allows an impulse to be passed along a neuron.
• Define the term epilepsy.
• Identify investigations that are likely to be carried out in order to diagnose epilepsy.
• Highlight why misdiagnosis is a problematic feature in epilepsy.
• Discuss the general management and administration of anti-epileptic drugs.
• Demonstrate an understanding of the mode of action and side-effects of valproate and lamotrigine.
• Explain how epilepsy is monitored to ensure that the medication regime is effective.
• Discuss the role of the nurse in patient concordance.
• Identify the care and medication needed in status epilepticus.
• Describe the information that would be given to carers about sudden unexpected death in epilepsy.
CASE
Mr Ralph is a 45-year-old man who has recently experienced the second of two seizures, in which he fell to the floor with violent jerking of his muscles. He has been admitted to A&E, as his care staff are concerned about his slow recovery from the second attack. It appears that he has experienced a tonic-clonic seizure, but this has yet to be confirmed. He shares a house with two other men and they all receive help with everyday living as they all have learning disabilities. Mr Ralph’s learning disability is described as ‘moderate’. He is independent in self-care skills and is able to communicate his wishes using a simple vocabulary.
1 What is the normal mechanism that allows an impulse to be passed along a neuron?
2 What do you understand by the term ‘epilepsy’?
4 What types of misdiagnosis can occur when a person is thought to have epilepsy?
After investigations and an outpatient appointment, Mr Ralph has been diagnosed with epilepsy. He has been prescribed sodium valproate. Over the next few months he continues to experience seizures, resulting in him being prescribed lamotrigine alongside sodium valproate.
5 Discuss the general management and administration of anti-epileptic drugs (AEDs)
6 Identify the action of valproate and specific issues around its use
7 Identify the action of lamotrigine and specific issues around its use
8 How should Mr Ralph’s epilepsy be monitored to ensure that his medication regime is effective?
9 How can Mr Ralph be helped to ensure that he adheres to his medication regime, bearing in mind that he self-medicates when there are no care staff at his house?
10 If Mr Ralph were to develop status epilepticus (often known as ‘status’), what changes might be needed to his care and medication?
11 What is SUDEP? What information should be given to Mr Ralph and his carers about this condition?
ANSWERS
1 What is the normal mechanism that allows an impulse to be passed along a neuron?
A Neurons differ a great deal in shape but they all consist of dendrites, a cell body and an axon. The dendrites respond to the chemical messengers (neurotransmitters) released from other neurons. The axon carries the impulse from the cell body towards the synaptic terminals, where neurotransmitters transfer the impulse to the next neuron.
Neurons are able to transmit nerve impulses by the following mechanism:
• The exterior of the cell has a greater concentration of positively charged sodium ions and inside the cell there are more positively charged potassium ions. This situation is maintained by special channels within the cell wall called sodium–potassium pumps. The interior of the cell contains negatively charged chloride ions, which gives the interior an overall negative charge, as compared to the exterior. This situation is known as the ‘resting potential’.
• The resting potential is restored by potassium ions moving outside the axon. The sodium–potassium pumps then pump out the sodium ions that entered the axon and bring the potassium ions back into the cell, restoring the cell to its resting potential.
• The impulse is passed to the next neuron at the synapse. Here there is a tiny gap between the end of the axon of one neuron and the end of the dendrite of the next. As the nerve impulse reaches the synapse it causes vesicles (small spherical packages) to release a chemical neurotransmitter. There are a variety of these within the nervous system.
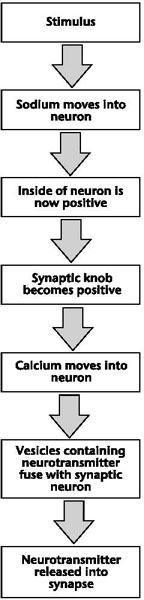
Figure 11.1 Flow chart of a neuron firing
2 What do you understand by the term ‘epilepsy’?
A Epileptic seizures have been described as repeated abnormal discharges of a group of neurons. This is caused by a high level of neuronal excitation and a deficit in the mechanism which inhibits this excitation. Put simply, an epileptic seizure is caused by abnormal firing of cerebral neurons, which spreads from a local starting point to other parts of the brain. Epileptic seizures can take many forms, depending on the part of the brain affected and the extent of the spread of abnormal activity. There are more than 40 types of seizure, with some described as unclassifiable (Manford 2003).
3 What investigations are likely to be carried out to determine whether Mr Ralph is suffering from epilepsy and, if so, what type(s) of epilepsy he is experiencing?
A Anyone with newly suspected seizures should be seen urgently (within two weeks) by a specialist. The most important information in the diagnosis of epilepsy is an accurate description of the events. Every piece of information, including the events before and after the seizure, can assist with this process. This will need to be provided by a witness (NICE 2012).
The following information is needed:
• Details of the events, as described by observers and the person. Mr Ralph may be able to describe what happened before the seizure and how he felt afterwards. The duration of the seizures is also important (Kerr 2009).
• The circumstances surrounding the event.
• Any patterns in the seizures such as the time, or any relationship to sleep.
• Any activity the person was undertaking at the time (e.g. exercise, resting, watching TV).
• Any possible circumstances that may have acted as a trigger. This might include stress, sleep deprivation, flickering lights or alcohol intake.
• Personal and family history. However, with people with intellectual disability, there may not always be access to family health information (Panayiotopoulos 2010).
If available, video recordings can be helpful in diagnosis, but clearly consent from Mr Ralph would need to be sought. A complete physical examination will also be carried out in order to identify any neurological abnormalities, any cardiac problems and to assess Mr Ralph’s mental status. NICE (2012) recommends an electroencephalogram (EEG) after a second seizure. The most commonly used investigation when epilepsy is suspected is the EEG, which records the electrical activity of the brain. In some cases this investigation will confirm a diagnosis. However, the results can provide a normal reading, and up to 50% of people who have been diagnosed with epilepsy have a normal EEG. Non-specific abnormalities may also be found that cannot be used to confirm a diagnosis (Welsh and Kerley 2009).
Mr Ralph may also be asked to hyperventilate while the recording is being made. This will involve him breathing deeply for about three minutes. If he is unable to understand this instruction, he may asked to blow on an item such as a pinwheel (if this approach has to be used it is important to remember to do this in a way that is as age-appropriate as possible). Hyperventilation is the most effective procedure for stimulating absence seizures and abnormal patterns of electrical activity in the brain. The EEG technician may also use intermittent photic stimulation (flashing lights), which can be a trigger for some people. Informed consent is required when photic stimulation and hyperventilation are used.
Brain imaging may also used to assist with diagnosis. This can involve magnetic resonance imaging (MRI), which can display structural abnormalities that may be the underlying cause of Mr Ralph’s possible epilepsy. X-ray computerized tomography (CT) scans may also be required, but they are less effective than an MRI.
Mr Ralph may also be sent for blood tests to rule out metabolic disorders and for an ECG to rule out heart conditions. On diagnosis, it is important that Mr Ralph and his carers, with his consent, are provided with information on epilepsy, access to counselling, details of an epilepsy specialist nurse and a named individual as a point of contact.
4 What types of misdiagnosis can occur when a person is thought to have epilepsy?
A Epilepsy can be difficult to diagnose accurately, with misdiagnosis occurring in up to 25% of people. Conditions that may be misdiagnosed as epilepsy include syncope (a brief loss of consciousness). This can have many causes but among them are some potentially serious conditions such as cardiac arrhythmias. In people with a learning disability, conditions that may be misdiagnosed as epilepsy are also likely to include:
• a variety of repetitive behaviours or apparent unresponsiveness;
• stereotyped movements associated with some syndromes (e.g. Rett syndrome);
• side-effects of medication;
• self-stimulation of seizures (Iddon et al. 2010).
This type of misdiagnosis can lead to people receiving medication they do not require, along with the possible side-effects. An underlying condition may remain untreated. They may also experience stress, social stigma and unnecessary lifestyle changes. People with epileptic seizures can also be misdiagnosed as having migraine or even encephalitis, resulting in mismanagement of their condition.
Table 11.1 Differential diagnosis of epilepsy
| Syncope |
| Non-epileptic attack disorder |
| Migraine |
| Daydreaming |
| Vertigo |
| Panic attacks |
| Drop attacks |
| Narcolepsy |
| Transient global amnesia |
| Movement disorder |
5 Discuss the general management and administration of AEDs
A The aim of treatment with AEDs is freedom from seizures without side-effects, or at least minimal reactions. The ability of Mr Ralph to be involved in treatment decisions should always be considered. Some general points include:
• A person-centred approach should be taken, in order to produce a comprehensive care plan, which will include a medication plan.
• Some anti-epileptics act by stabilizing the neuron membrane in order to reduce the excitability of the neuron. Others increase the activity of gamma-aminobutyric acid (GABA) (a transmitter which has an inhibiting effect at the synapse), while some appear to combine both actions.
• Polytherapy is best avoided, but Mr Ralph failed to respond to a single drug. This is the case in about 30–50% of patients. Side-effects are more likely in relation to polytherapy.
• It is important that patients and carers are informed regarding the purpose of the medication, the duration of treatment and possible adverse reactions.
• Many AEDs are effective only for certain seizure types and can be contraindicated for others. Others are described as ‘broad spectrum’, being effective for more than one type of seizure.
• AEDs are particularly prone to drug interactions.
• Side-effects caused by anti-epileptic drugs fall into the following groups: CNS-related (e.g. sedation, poor coordination, tremor and headache); behavioural/mental health-related (e.g. depression) (however, some AEDs have mood-stabilizing properties); cardiovascular and renal effects.
• People with learning disabilities commonly experience weight changes, gait disturbance and altered mood (Sipes et al. 2011).
• People with learning disabilities and epilepsy appear to be more at risk of falls, due either directly to the seizures or to the effects of medication (Willgoss et al. 2010).
• When working with people with limited communication, carers need to be particularly observant to detect adverse drug reactions.
• If drugs need to be changed or withdrawn, this needs to be done slowly, the dose being gradually changed (normally every two weeks).
• It is recommended that the medication dispensed should be obtained from one manufacturer, as there can be differences in the bio-availability of medication obtained from different manufacturers.
Table 11.2 Most commonly used drugs in epilepsy
| Primary generalized epilepsies | Focal epilepsies |
| Sodium valproate | Carbamazepine |
| Lamotrigine | Lamotrigine |
| Phenytoin (in the developing world) | Sodium valproate |
| Phenobarbital and phenytoin (in the developing world) |
6 Identify the action of valproate and specific issues around its use
A Sodium valproate is effective for virtually all types of seizure. It is believed to have two modes of action. Firstly, it triggers the release of the neurotransmitter GABA. GABA is found throughout the CNS and is considered to be the main inhibitory neurotransmitter. Alongside this it inhibits the sodium channels in the walls of the neuron (Galbraith et al. 2007).
Sodium valproate is eliminated from the body via the liver and one of the major concerns is that it can damage this organ. Mr Ralph may need to have liver function tests before it is prescribed and any impairment of his liver function will prevent him from taking this medication. His liver function might also be monitored for the first six months. Page et al. (2006) identify that toxic effects on the liver are more likely when sodium valproate is used alongside another AED. Liver problems are more likely in people with learning disabilities.
Sodium valproate can also be associated with pancreatitis and thrombocytopenia. A full blood count should be carried out before Mr Ralphs starts the medication and prior to any surgery. Mr Ralphs’s carers need to be alerted to the symptoms of liver disease and pancreatitis (nausea, vomiting, anorexia, jaundice) and thrombocytopenia (bleeding and bruising). Other possible effects might be increased appetite and weight gain, hair loss and ataxia or tremor. The tremor is usually reversible if the medication is stopped or reduced. He may also experience gastric problems, which can be reduced by the use of an enteric-coated formulation. He should be advised to take his medication with food. Some patients may also experience drowsiness and even confusion, although this is unusual (Bourgeois 2009).
Sodium valproate interacts with other medications. For example, it inhibits the metabolism of drugs such as phenobarbitone, lamotrigine and phenytoin, all of which can be used in the treatment of epilepsy. Sodium valproate is hydroscopic, i.e. it attracts water from the air. For this reason it is packed in foil. If a half tablet is prescribed, the remaining half should be discarded as it will be inactivated by moisture from the air (BNF 2012).
Sodium valproate may have mood stabilizing properties. Lower doses of psychotropic drugs may be used in people receiving sodium valproate. This may be helpful for Mr Ralph if he experiences mood changes (Leunissen et al. 2011).
7 Identify the action of lamotrigine and specific issues around its use
A Lamotrigine is used for generalized seizures that are poorly controlled by other medications. The action of lamotrigine involves the inhibition of the passage of sodium through the walls of the neuron. It also reduces the release of glutamate, which is an excitatory neurotransmitter. These actions reduce the uncontrolled repeated firing of the neurons (BNF 2012).
The main advantage of lamotrigine is that it has fewer side-effects, such as cognitive and psychomotor effects, than other medication. However, side-effects can occur and one of the most common is a skin rash. This is more common when the drug is combined with sodium valproate. The rash is often itchy and it can progress to involve the mucous membranes (Stevens-Johnson syndrome) or even toxic epidermal necrolysis, which is a potentially life-threatening condition (Matsuo and Riaz 2009).
Other side-effects include insomnia, headache, nausea, dizziness and double vision, particularly when given in combination with other AEDs. Lamotrigine does interact with other medication. When given with sodium valproate it can reduce the rate of elimination of valproate from the body. Mr Ralph and the people caring for him need to be informed regarding the side-effects in general, and in particular the possibility of a rash.
8 How should Mr Ralph’s epilepsy be monitored to ensure that his medication regime is effective?
A It is important that this patient’s condition is monitored so that medication levels can be adjusted to provide the best possible treatment with minimum side-effects. The monitoring should include:
• Regular reviews. A regular structured review at least annually with a specialist or generalist is important, depending on the success of the treatment regime.
• Regular blood test monitoring, unless there are specific indications. This may be useful if it is suspected that the drug regime is not being adhered to, or if toxicity or drug interactions are suspected.
• The occurrence of any seizures, their duration and any change in their nature.
• Adverse effects observed, such as changes in Mr Ralph’s ability to function, his behaviour and anything that he is able to indicate to his carers.
• Possible use of specific screening tools. the Glasgow Epilepsy Outcome Scale (GEOS-C) allows the person with epilepsy to report their concerns about the situation (Watkins et al. 2006).
9 How can Mr Ralph be helped to ensure that he adheres to his medication regime, bearing in mind that he self-medicates when there are no care staff at his house?
A Adherence to medication can be assisted by:
• Education for the person and their carers on their condition and the medication they are prescribed.
• Reducing the stigma of having epilepsy. This may be less of an issue for Mr Ralph, as epilepsy is common among people with learning disabilities – however, you should not make assumptions.
• A simple medication regime. Medication can be dispensed in packaging that simplifies the process.
• A positive relationship between Mr Ralph and his carers and health care professionals. Carers should be aware of the most likely side-effects of his medication, any idiosyncratic effects and sources of help and advice (Welsh and Kerley 2009).
10 If Mr Ralph were to develop status epilepticus (often known as ‘status’), what changes might be needed to his care and medication?
A Status epilepticus (often described as ‘status’) is a condition in which a seizure is prolonged or seizures follow on rapidly from each other. When this occurs in a tonic-clonic seizure, intervention is required as the condition can cause permanent cerebral damage and can be life-threatening. Tonic-clonic status has been defined as prolonged or recurrent seizures lasting for 30 minutes or more (Shorvon 2010). However, some services may use other criteria.
Status requires urgent treatment and the two most commonly used emergency medications are rectal diazepam or buccal midazolam. When a person is known to be prone to status, one of these drugs will often be prescribed and made available for carers to administer. Training will be required in administration. Buccal midazolam is now more often given as it is squirted using a syringe between the lower jaw and the cheek on one side of the mouth, making administration easier and more dignified. For Mr Ralph, his carers will need to be trained in how to identify and treat his status, should it recur, and how to recognize the need to summon emergency help. The service will also need to consider the possibility of this occurring when the house is unstaffed – a careful risk assessment will need to be carried out, along with Mr Ralph, in order to plan his care.
11 What is SUDEP? What information should be given to Mr Ralph and his carers about this condition?
A SUDEP (sudden unexpected death in epilepsy) occurs in about one death per 2500 people with mild epilepsy and about one death per 100 people with those with severe epilepsy. It usually occurs after a seizure of a convulsive type. People with a learning disability are particularly at risk. The condition is poorly understood, but it may be the result of respiratory arrest or cardiac arrhythmias. It occurs most often when people are asleep or alone. Respiration after a seizure can be encouraged by stimulation, which may explain why witnessed seizures are less likely to be followed by SUDEP.
In relation to Mr Ralph, he has the right to know about all the risks posed by his epilepsy. The issue of how much people should be told about SUDEP condition has been debated. Neurologists and epilepsy specialist nurses are more likely to discuss it with patients who are at risk or who have asked about the condition. In general, staff should be guided by how much a patient wants to learn about their condition. Consideration should also be given to the fact that any action to reduce the number of attacks experienced by Mr Ralph will reduce the risk of SUDEP (Lewis 2011).
KEY POINTS
• The axon of a neuron carries the impulse from the cell body towards the synaptic terminals, where neurotransmitters transfer the impulse to the next neuron.
• Epileptic seizures have been described as repeated abnormal discharges of a group of neurons.
• Careful observation is required to ensure an accurate diagnosis of epilepsy.
• AEDs are prone to drug interactions and side-effects. With a person with learning disability, carers need to be observant in order to detect any problems. Regular reviews are important.
• The action of lamotrigine involves the inhibition of the passage of sodium and reduces the release of glutamate, which is an excitatory neurotransmitter.
• Any changes to medication need to be carried out gradually, under medical supervision.
• Status epilepticus is more common in people with learning disabilities – care staff need to be able to identify this and know how to respond.
• SUDEP occurs in about one death per 2500 people with mild epilepsy and about one death per 100 people with those with severe epilepsy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


