The person with diabetes mellitus type 2
CASE AIMS
After examining this case study the reader should be able to:
• Briefly explain what observations and investigations would be carried out in order to diagnose type 2 diabetes.
• Describe the pathophysiology of type 2 diabetes in order to explain the symptoms.
• Discuss the advice the nurse would give regarding diet and exercise in managing type 2 diabetes.
• Outline the key points of the National Institute for Health and Clinical Excellence (NICE) guidelines with regard to oral hypoglycaemics.
• Demonstrate an understanding of the mode of action and side-effects of metformin.
CASE
Deborah Jones, aged 55, has been complaining of feeling tired, generally feeling unwell and being thirsty all the time. She complains that her feet have been feeling ‘hot’. She has also been unkind to her children, shouting and arguing with them for no apparent reason. She complains of craving for chocolates and sweet things. She says she knows something is not right. On examination, Mrs Jones explains that she has noticed she has been going to the toilet more than in the past, sometimes getting up at night three to four times. She also complains of itchiness ‘down below’ (pruritis vulvae) and blurred vision, which she attributes to ‘getting old’. Mrs Jones is also overweight with a body mass index (BMI) of 28.
1 What observations and investigations would the doctor carry out in order to confirm the diagnosis?
2 Why has Mrs Jones developed symptoms of feeling thirsty, tired and suffering polyuria, nocturia and itchiness?
3 Discuss the role that diet and exercise will have in managing Mrs Jones’ type 2 diabetes.
After three months, Mrs Jones returns to the practice still complaining of feeling tired, thirsty and getting up five to six times a night to go the toilet. Her blood glucose is 15mmol/L. Her HbA1c is 59 mmol/mol (7.5%). On further questioning, it is discovered that Mrs Jones has not been following any specific meal plan as advised by the dietician. Mrs Says that because of her job and children and other commitments, she does not have time to comply with the meal plan. She tends to cook a high- energy food, with a large amount of fried foods. She also says that she cannot fit the suggested exercise plan into her busy lifestyle. The doctor advises her that he must start her on metformin, an oral hypoglycaemic, because the lifestyle advice about diet and exercise has failed to achieve the target blood glucose and HbA1c as recommended by NICE.
4 What are the key points of the NICE guidelines with regard to oral hypoglycaemics?
5 What are the modes of action and side-effects of metformin?
ANSWERS
1 What observations and investigations would the doctor carry out in order to confirm the diagnosis?
A HISTORY
The following are key areas when taking this person’s history:
• It is important that the doctor considers other illnesses. Malignancy of the liver or pancreas, hyperparathyroidism and Cushing’s disease may produce signs and symptoms similar to diabetes mellitus.
• There are some commonly used medications that may precipitate diabetes mellitus. They are also known as diabetogenic drugs. Some examples are steroids, beta-blockers, such as atenolol, and thiazide diuretics.
• Mrs Jones will be asked about her smoking habits and alcohol intake.
• Her occupational history is also important. Diabetes mellitus, if left uncontrolled and unmanaged, may interfere with judgement and dexterity.
• The doctor will also be asking about any symptoms suggestive of current vascular symptoms – for example, chest pain, breathlessness or orthopnoea (Wass et al. 2011).
EXAMINATION
The doctor will do a complete physical examination, focusing on the cardiovascular assessment. A major complication of diabetes mellitus is macro-vascular complications, such as:
• hypertension;
• heart disease;
• stroke.
Another set of complications is micro-vascular problems, such as:
• diabetic retinopathy;
• neuropathy;
• nephropathy (National Collaborating Centre for Chronic Conditions for NICE 2008).
The doctor will also do a foot examination, including the main pulses in the lower limbs:
• the femoral;
• the popliteal;
• the dorsalis pedis;
• the posterior tibial.
Absence of these pulses may suggest that the artery may be blocked by atheroma, thrombosis or by an embolus. Remember that Mrs Jones complained that her feet were feeling hot. Absence and/or lack of feelings, and ‘pins and needles’ in her feet and legs may be suggestive of peripheral neuropathy.
A complete examination may find that there is some evidence of infection, such as a ‘boil’, which may have precipitated Mrs Jones into frank diabetes. Mrs Jones is also overweight, which may be a contributing factor.
INVESTIGATIONS
• According to the American Diabetes Association (2012), type 2 diabetes is diagnosed if the ‘fasting plasma glucose’ level is 6.9mmol/L or greater. In a person who has no symptoms, the investigation must be repeated. If the repeat test is also above 6.9mmol/L, then the person is diagnosed with diabetes mellitus.
• A random plasma glucose level is inexpensive and convenient to obtain, and most people find the test acceptable. However, it has poor sensitivity and specificity compared with the glucose tolerance test. If a random glucose test is used, the findings have to be interpreted with great care, since there may be a risk of a missed diagnosis.
• A fasting plasma glucose level has greater sensitivity and specificity than the random plasma glucose level. However, if the repeat test is normal, the patient would be advised to be monitored regularly by the doctor or nurse. The patient has to fast for at least eight hours prior to the blood test.
• The doctor would ask for a blood test known as HbA1c (glycosylated haemoglobin). This test is also used to monitor the progress of Mrs Jones’ diabetes. Glycosylated haemoglobin (HbA1c) is a blood test that measures the average plasma glucose concentration over two to three months. This gives a good indication of the blood glucose level in the previous two to three months. If Mrs Jones’ blood glucose is normal, it will produce a normal amount of glycosylated haemoglobin, which is in the range 20–42mmol/mol (4–6%). However, if Mrs Jones’ HbA1c is above 48 mmol/mol (6.5%) it may indicate that she has diabetes mellitus. However, to establish a definitive diagnosis, there must be two different criteria – for example, a combination of an elevated HbA1c and elevated fasting plasma glucose.
• A urine test may be carried out to investigate for glucose, acetone and albumin. If acetone is found then Mrs Jones’ diabetes is in urgent need of control and this will be done before any investigations are undertaken.
• Blood would be taken to test urea and electrolytes (U&Es) and creatinine. This is to ensure that Mrs Jones’ electrolytes are well within parameters, because a consequence of polyuria is electrolyte loss. Electrolyte imbalance may cause cardiac arrhythmias. Fasting lipids will be carried out, since a high level in people with diabetes predisposes them to acute coronary disease.
• An electrocardiograph may also be done to assess the physiology of the heart and detect any abnormalities early on.
2 Why has Mrs Jones developed symptoms of feeling thirsty, tired and suffering polyuria, nocturia and itchiness?
A
• Polyuria is the act of going to the toilet for passing urine more frequently than normal. It is caused by osmotic diuresis caused by a high glucose level in the blood (glycosuria). Getting up at night more than usual to empty the bladder is known as nocturia.
• A pruritis vulva in women is the result of glycosuria and candida infection. Infection is present because hyperglycaemia increases the risk of infection and also because infections stimulate the secretion of stress hormones which weaken the immune system. We know that 50% of women have candida living naturally in their vagina without it causing any problems. However, in diabetes mellitus, the high level of glucose surrounding the vagina affects the balance of acidity and alkalinity, causing an increase in the growth of the yeast-like fungi called candida. Candida causes pruritus vulvae (vaginal thrush) in women, and should be a warning sign for diabetes mellitus.
• Feeling tired is due to the fact that there is a shortage of energy being produced from the carbohydrate ingested, due to either insulin deficiency or resistance to insulin action in the peripheral tissues or both. The energy deficit may be due to glucose being lost through the urine, which may amount to several calories per day.
• Blurred vision is due to glucose-related osmotic changes to the shape of the lens.
Incidentally, the reason why Mrs Jones was so irritable with her children may have been due to mood swings caused by hyperglycaemia (Wass et al. 2011).
3 Discuss the role that diet and exercise will have in managing Mrs Jones’ type 2 diabetes
A
• The initial management of type 2 diabetes consists of weight loss and exercise which, if substantial, will reverse hyperglycaemia. However, most patients with type 2 diabetes have been making the ‘wrong’ lifestyle choices all their lives and rarely respond to standard approaches (NICE 2012).
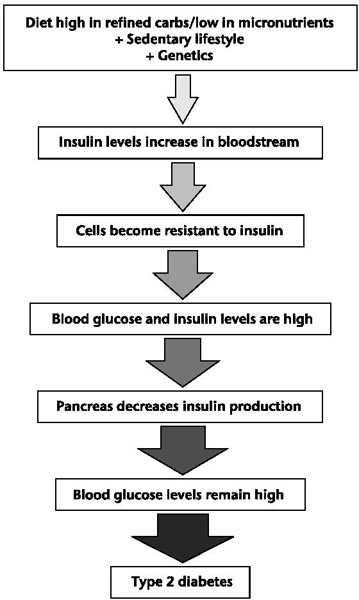
Figure 10.1 How insulin resistance progresses towards type 2 diabetes
• Advice should be given about the appropriate timing for meals and snacks and the amount of carbohydrate eaten. According to dietary recommendations, people suffering from diabetes should eat starchy foods regularly; eat more fruit and vegetables; reduce animal, saturated and trans-fatty acids; eat low-fat dairy products and oily fish; cut down on sugar; and reduce salt. Mrs Jones should be able to enjoy some foods containing sugar as long as these are part of her overall balanced diet.
• Mrs Jones should be advised about commonly available food marketed specifically for people with diabetes: these tend to be expensive and not necessarily very helpful.
• Advice on alcohol consumption should also be given. Alcohol may compound the effect of diabetes on blood pressure which may have a deleterious effect on the cardiovascular system and specifically the heart. Drinking moderate alcohol (two drinks daily for men, one for women) is acceptable, but drinking alcohol in excess of the recommended level increases the risk of hypoglycaemia as well as other untoward events.
• If Mrs Jones smokes, advice, support and help will be given to help her stop. She should be helped to enrol in a ‘smoking cessation’ programme.
• Since Mrs Jones is overweight, she will be given advice, help and support to lose some weight. She will be advised that the nearer she gets to a healthy body weight, the better it will be for her long-term health (NICE 2006).
• Mrs Jones will be advised to take regular exercise. This may be used as a complementary tool to caloric restriction for weight reduction and to improve insulin sensitivity in the overweight insulin-resistant person. The objectives for Mrs Jones should be to promote the incentive to incorporate exercise into her daily life – for example, walking. Mrs Jones should also be given advice on how to prevent the complications of exercise – for example, hypoglycaemia. However, if she has any evidence of heart disease, the doctor will have to assess her prior to increasing levels of exercise (Di Loreto et al. 2005).
4 What are the key points of the NICE guidelines with regard to oral hypoglycaemics?
A The NICE guidelines recommend that the management of type 2 diabetes should include:
• patient education;
• advice about diet;
• advice about exercise;
• advice about smoking;
• advice about alcohol;
• advice about lifestyle.
If these initial strategies, as carried out for Mrs Jones above, fail to achieve the blood glucose objectives, blood glucose lowering therapy should then be started. Metformin should be the drug of choice if there is no contraindication.
Table 10.1 Tablets used in type 2 diabetes
| Drug group | Product name | Information |
| Biguanides | Metformin | Helps the cells of the body to use insulin. Does not cause hypoglycaemia as it does not stimulate the pancreas to secrete insulin. Does not cause weight gain. May cause nausea and vomiting |
| Sulphonureas | Glipizide | These drugs stimulate the pancreas to produce more insulin. They can cause hypoglycaemia and lead to weight gain; therefore they should be prescribed to people of normal weight |
| Meglitinides | Nateglinide (Starlix) | Increase the amount of insulin produced during a meal. Can be used alongside metformin |
| Thiazolidinediones | Rosiglitazone | Help insulin sensitivity. May be used with either a sulphonurea or biguanide but not both. At present cannot be used alongside insulin |
| Alpha-glucosidase inhibitors | Acarbose (Glucobay) | Works by delaying the rate at which sugars are digested. Side-effects include flatulence, a bloated feeling and diarrhoea. Acarbose can be used alongside other hypoglycaemic agents in this table |
5 What are the mode of action and side-effects of metformin?
A MODE OF ACTION
Metformin is the treatment of choice when strict dieting has failed to control diabetes. It may also be an option for patients who are not overweight. Metformin works via three mechanisms:
• By reducing hepatic glucose production by inhibiting gluconeogenesis (the formation of glucose from non-carbohydrate carbon) and glycogenolysis (the formation of glucose by converting glycogen) in the liver. This reduces the hepatic glucose output which underpins basal and night-time hyperglycaemia (Warrell et al. 2010).
• By increasing insulin sensitivity in the muscles it improves peripheral glucose uptake and utilization.
• It also delays intestinal glucose absorption.
Metformin only works in the presence of endogenous insulin, therefore it is essential that there is secretion of endogenous insulin. At maximal effective doses, metformin may reduce HbA1c by 1 to 2%. It rarely causes hypoglycaemia when used as monotherapy, because it does not stimulate insulin secretion. It is rarely associated with weight gain. Metformin has favourable effects on lipid metabolism, shown at therapeutic doses. It reduces total cholesterol, low density lipoprotein (LDL), cholesterol and triglyceride levels. Metformin is the only glucose-lowering therapy that has been shown to possibly reduce cardiovascular mortality in type 2 diabetes (UKPDS Group 1998).
SIDE-EFFECTS
Metformin has a short half-life and is therefore a short-acting drug. It needs to be given two or three times a day, which may impact on a patient’s compliance and concordance. Some of the side-effects of this drug are:
• nausea;
• vomiting;
• diarrhoea;
• gas;
• abdominal pain;
• taste disturbance;
• anorexia.
These side-effects may discourage Mrs Jones from being concordant with the medication regimen. She must be advised not to give up, since the problems are mild and will subside. The doctor may start the drug regimen with a low dose and increase it slowly to minimize the risk of side-effects (Cramer et al. 1989)
Metformin may impair the absorption of vitamin B12 leading to vitamin B12 deficiency in some patients, causing megaloblastic anaemia. Metformin should be stopped before surgery or contrast dye studies with radiographic dye injection, and not recommence until there is evidence of good renal function. It must be used with caution in patients with impaired renal and liver function and post MI, because there may be a risk of lactic acidosis. Blood lactate levels are slightly raised in patients receiving metformin, and can rise rapidly and cause life-threatening acidosis if lactate accumulates due to renal failure.
Mrs Jones should be advised to contact the doctor and/or the diabetic liaison nurses if she experiences any signs and symptoms associated with renal failure and acidosis. However, it should be emphasized to her not to stop her medications without consultation with the doctor or nurse (UKPDS Group 1998; BNF 2012).
KEY POINTS
• The gold standard for the diagnosis of diabetes is the oral glucose tolerance test.
• The blood test known as HbA1c (glycosylated haemoglobin) would enable the doctor to monitor the development and progress of Mrs Jones’ diabetes.
• The aim of treatment is to eliminate symptoms of hyperglycaemia without causing hypoglycaemia and to decrease the risk of long-term damage to organs and tissues.
• Mrs Jones would be advised about the importance of eating a well-balanced diet, taking her diabetes into consideration.
• Metformin works by reducing hepatic glucose production and increasing insulin sensitivity in the muscles,.
• The side-effects of metformin are mainly GI-related symptoms.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


