Chapter 37 SKIN INTEGRITY AND WOUND CARE
THE INTEGUMENTARY SYSTEM
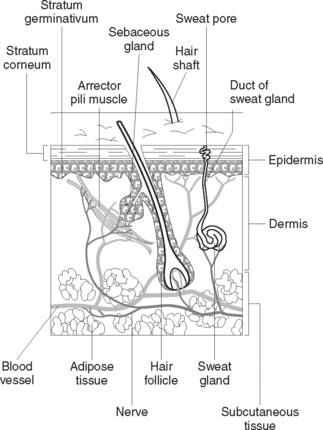
The integumentary system consists of the skin and its appendages; the hair, nails, sweat and sebaceous glands. The skin (or integument) is the largest organ of the body, covering about 7500 cm2 of surface area in an average adult (Figure 37.1). It is a protective barrier to the outside world, plays a vital role in homeostasis, and also provides a major means of communication through touch and sensation. The appendages of the skin — hair, nails and glands — arise from the epidermis but are present in the dermis.
STRUCTURE OF THE SKIN
FUNCTIONS OF THE SKIN
Protection
The skin is the first line of defence against the external environment. It provides a barrier to a variety of harmful agents, such as microorganisms, radiant energy and chemical substances. The skin acts as a barrier to harmful agents only as long as it remains intact. The waterproof quality of the outer layer prevents excess water absorption and abnormal loss of body fluids. The skin contains nerve endings that are sensitive to painful stimuli. The nerve endings transmit impulses to the brain that alert the individual that damage is occurring.
WOUND HEALING
THE INFLAMMATION PHASE
This phase begins the moment that injury is incurred. The capillaries contract and thrombose to facilitate haemostasis. Vasodilation of the surrounding tissues occurs in response to the release of histamine and other vasoactive chemicals. This process causes increased blood flow to the surrounding tissue, which produces erythema, swelling, heat and discomfort, such as throbbing. A variety of white blood cells called polymorphonuclear leucocytes arrives at the site of the wound as a defence response and is involved in the immune response to fight infection. Polymorphs, macrophages and their associated growth factors produce various local and systemic effects. This phase continues for about 3 days.
HEALING INTENTIONS
When the wound has minimal tissue loss and the edges can be brought together by sutures or clips, as in a surgical wound, the wound is said to heal by primary intention, or first intention. Granulation tissue is not obvious. Healing by secondary intention occurs when wound edges cannot be brought together, as with a gaping wound. Granulation tissue fills in the wound until re-epithelialisation takes place and a large scar results. Third intention, or delayed primary intention, healing occurs when wound closure is delayed for a few days, so that an infected or contaminated wound can be debrided (dirt, foreign objects, damaged tissue and cellular debris are removed from a wound or burn to prevent infection and promote wound healing). Closure of contaminated wounds is usually delayed until all layers of wound tissue show no signs of infection, usually within 4–10 days. At other times some wounds need surgical intervention such as the application of skin grafts or flaps to speed the healing process and reduce the risk of infection. Clinical Interest Box 37.1 provides details on skin grafts.
CLINICAL INTEREST BOX 37.1 Skin grafts
TYPES OF WOUNDS
ACUTE AND CHRONIC WOUNDS
Acute wounds
Acute wounds in early stages are frequently not colonised with bacteria, but infection can become a complication. Although infection cannot always be prevented, care should be taken to minimise transmission by thorough aseptic technique when attending to the wound. Examples of acute wounds are those made by surgical incision or traumatic injury. An example of a surgical wound is a skin flap (refer to Clinical Interest Box 37.2).
Chronic wounds
Chronic wounds are rarely sterile. Microbial colonisation is usually present, predisposing the wound to infection. Clinical infection depends on the virulence of the bacteria and the resistance of the host. Clinical Interest Box 37.3 provides the differences between inflammatory response and infection. An example of a chronic wound is a venous leg ulcer.
CLINICAL INTEREST BOX 37.3 Recognising the differences between inflammatory response and infection
| Inflammation | Infection |
|---|---|
Wounds can be described according to the amount of damage done to the tissues:
PATHOPHYSIOLOGICAL INFLUENCES/EFFECTS AND MAJOR MANIFESTATIONS OF SKIN DISORDERS
PATHOPHYSIOLOGICAL INFLUENCES AND EFFECTS
MAJOR MANIFESTATIONS OF SKIN DISORDERS
Various structural and functional changes accompany skin disorders.
Lesions
Depending on the type of skin disorder, one or a variety of lesions may be present. Observation of the patient includes assessing any lesions to determine their shape, size and distribution. Table 37.1 lists and describes the various types of skin lesions. Some types of lesions may discharge fluid, which is referred to as exudate.
| Term | Description | Examples |
|---|---|---|
| Bulla | Elevated, filled with clear fluid. Similar to a vesicle, but larger | Pemphigus vulgaris, drug eruptions, partial thickness burns |
| Comedo | A plug of secretion contained in a follicle | Acne |
| Crust | A superficial mass caused by dried exudate | Impetigo, eczema |
| Cyst | Encapsulated mass in the dermis or subcutaneous layer. May be raised or flat, and contain fluid or solid material | Sebaceous cyst |
| Erosion | Moist, red, depressed break in the epidermis. Follows rupture of a vesicle or bulla | Chickenpox |
| Excoriation | Superficial break in the skin | Scratches, abrasions |
| Fissure | Deep, linear, red crack or break exposing the dermis | Tinea pedis |
| Macule | Small circumscribed discolouration, e.g., red, white, tan or brown | Freckle, rubella, scarlet fever |
| Nodule | Circumscribed, elevated area — usually 1–2 cm in diameter | Ganglion, acne |
| Papule | Circumscribed, elevated, firm palpable area | Mole, wart, pimple |
| Plaque | Elevated, rough flat-topped areas | Psoriasis, seborrhoeic warts |
| Pustule | A vesicle or bulla containing pus | Acne, furuncle, folliculitis, impetigo |
| Scale | Mass of exfoliated epidermis | Dandruff, psoriasis |
| Scar (cicatrix) | Ranges from a thin line to thick, irregular fibrous tissue. May be white, pink or red | Healed surgical incision or wound |
| Tumour | Elevated, solid formation | Lipoma, melanoma, fibroma |
| Ulcer | Depressed circumscribed area involving loss of the epidermis, exposing the dermis, and may involve subcutaneous tissue | Decubitus ulcer, stasis ulcer |
| Vesicle | Circumscribed, elevated superficial area filled with clear fluid | Blister, herpes simplex infection, contact dermatitis |
| Weal | Transitory, elevated irregularly-shaped swelling of the epidermis | Urticaria, insect bites |
SPECIFIC DISORDERS OF THE SKIN
IDIOPATHIC DISORDERS
Idiopathic disorders are those in which no definite cause can be identified.
Pityriasis rosea is thought to be caused by a virus, and is characterised by a scaling, pink macular rash that spreads over the trunk and other parts of the body. The condition is self-limiting and usually disappears within 4–6 weeks.
Vitiligo is a benign disorder consisting of irregular patches of skin totally lacking in pigment.
HYPERSENSITIVITY DISORDERS
These disorders result from an immediate or delayed reaction after exposure to a certain substance.
NEOPLASIA
A melanoma is a malignant tumour that arises from melanocytes. The incidence of melanoma seems to be related to prolonged exposure to the sun, particularly by fair-skinned people. Because metastatic dissemination is relatively common, the mortality rate is high. In its pre-malignant stage, a melanoma appears as a flat, irregularly pigmented macule. Colour changes appear as the melanoma becomes malignant and invasive, with the colour ranging from red, brown and blue to black. Melanoma can occur on any part of the body but most frequently occurs in areas of the skin exposed to sunlight. There are many types of melanoma and, because of its invasive nature, the nodular type is the most serious. Australians have the highest rate of malignant melanoma in the world, and the incidence is particularly high in Queensland and the tropics.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree