Chapter 42 SENSORY ABILITIES
Well, I must admit, it has made a big difference to my life. Joan was right and in a way I’m pleased she pushed me into action. I was just missing out on so many things. I could see her frustration and now realise that the answer was a simple hearing test and a hearing aid. I was too proud to be labelled ‘disabled’ so I struggled on for the last couple of years with my deteriorating hearing only catching the end of phrases, blaring the television out and picking up on a bit of lip-reading. No doubt my 40 years of working in the timber mill until my retirement and the fact that I’m now 76 years old are both contributing factors to my hearing loss. Of course, the biggest bonus is that the grandchildren hardly notice the hearing aid and now I can hear them and enjoy their little concerts they perform for me when they come to visit Grandpa.
COMPONENTS OF THE SENSORY EXPERIENCE
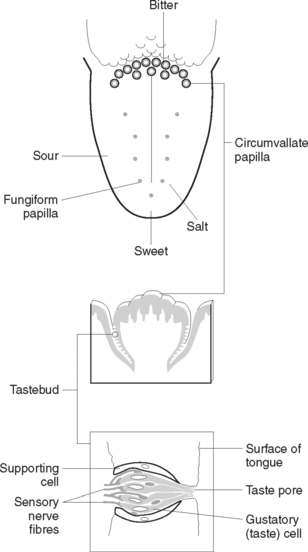
THE TONGUE (TASTEBUDS)
The sensory receptors for taste are the taste buds. They are widely scattered in the oral cavity, with most concentrated over the surface of the tongue (Figure 42.1) and a few found on the soft palate and inner surface of the cheeks. They are chemoreceptors that respond to substances present in food and generate nerve impulses that are transmitted to the brain for interpretation. The upper surface of the tongue is covered with small projections (papillae) some of which contain a taste bud. Each taste bud consists of sensory and supporting cells situated in the epithelium and opening into the surface through a small gustatory pore. Between the cells of the taste bud lie the ending of afferent nerve fibres derived from several cranial nerves. Taste buds on the anterior two-thirds of the tongue connect with fibres of the facial (seventh cranial) nerve. Taste buds on the posterior one-third of the tongue are associated with the fibres of the glossopharyngeal (ninth cranial) nerve, while pharyngeal taste buds send impulses to the brain via the vagus (tenth cranial) nerve.
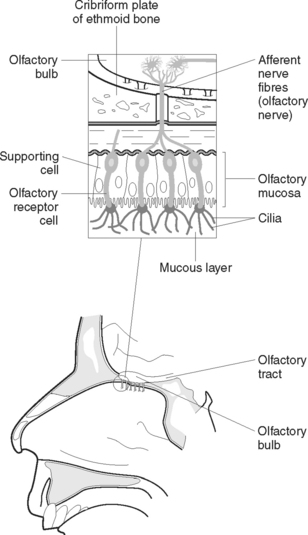
THE NOSE (OLFACTORY RECEPTORS)
The specific receptors for the sense of smell are the olfactory receptors. They are chemoreceptors that respond to airborne chemicals and generate impulses that are transmitted to the brain for interpretation. The olfactory receptors are situated in the mucous membrane lining the upper part of the nose (Figure 42.2). When these receptors are stimulated by chemicals they transmit impulses along the olfactory nerve to the brain. These receptors adapt quickly when exposed to an unchanging stimulus, which means that the client can become accustomed to an odour when constantly exposed to it.
SENSORY ALTERATIONS
Sensory deprivation
Sensory deprivation is thought of as a decrease or lack of meaningful stimuli. Because of reduced stimulation, a person becomes more acutely aware of the remaining stimuli and often perceives these in a distorted manner. The individual often experiences alterations in perception, cognition and emotion (Clinical Interest Box 42.1).
Sensory overload
Sensory overload can prevent the brain from ignoring or responding to specific stimuli. The clinical signs of sensory overload are listed in Clinical Interest Box 42.2.
Sensory deficits
A sensory deficit is impaired reception, perception, or both, of one or more of the senses. Impaired hearing and sight are sensory deficits. When only one sense is affected, other senses may become more acute to compensate for the loss. However, sudden loss of eyesight can result in disorientation. When there is a gradual loss of sensory function, people often develop behaviours to compensate for the loss; for example, a person with gradual hearing loss in the right ear may unconsciously turn the left ear towards a speaker. Clients with sensory deficits are at risk of both sensory deprivation and sensory overload (Kozier et al 2000).
Factors affecting sensory function
A range of factors affect the amount and quality of sensory stimulation, including a person’s developmental stage, culture, level of stress, medications, illness and lifestyle. These are outlined in Clinical Interest Box 42.3.
CLINICAL INTEREST BOX 42.3 Factors that influence sensory function
Age
Environment
Pre-existing illness
ASSESSING SENSORY FUNCTION
Nursing assessment of sensory-perceptual functioning includes:
CLINICAL INTEREST BOX 42.4 Interview to assess a client’s sensory-perceptual functioning
Visual
Gustatory
THE EYE
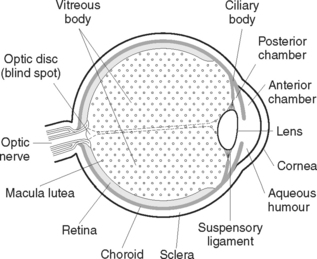
STRUCTURE OF THE EYE
The eye is a spherical structure (Figure 42.3) about 2.5 cm in diameter, consisting of three principal layers.
The outer layer
The outer fibrous layer consists of the sclera and the cornea, which is a transparent structure continuous with the sclera. About five-sixths of the outer surface is made up of a tough white opaque fibrous layer (sclera), while the cornea comprises the anterior one-sixth. Both the sclera and the cornea consist of layers of collagen fibres. In the cornea, the fibres are regular in size and arrangement, which accounts for its transparency. The cornea functions as a refracting and protective layer through which light rays pass en route to the brain.
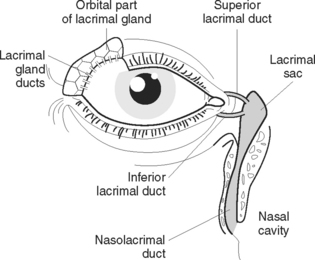
Extraocular structure — accessory structures
The lacrimal apparatus (Figure 42.4) consists of the lacrimal gland, which is situated over the eye at the upper outer corner and secretes tears, which constantly wash over the conjunctiva. Tears leave the gland via several small ducts, and pass over the front of the eye eventually draining into the lacrimal sac, which is the expanded end of the nasolacrimal duct. Tears are secreted on to the anterior surface of the eyeball and are spread over it by the blinking movements of the eyelids. An antimicrobial substance in tears protects the eyes against microorganisms. Excess tears drain down the nasal cavity. The lacrimal glands are stimulated in response to chemical and mechanical irritants, thus producing tears to wash away irritants. Tears may also be produced as a result of emotion such as sadness, or happiness.
The refractive media
The refractive media are the transparent parts of the eye, and have the ability to bend light rays at the surfaces of two transparent media. The refractive media are the cornea, the lens, the aqueous humour and the vitreous humour. The cornea functions as a refracting and protective layer through which light rays pass en route to the brain.
DISORDERS OF THE EYE
FACTORS AFFECTING SENSORY FUNCTION
SPECIFIC DISORDERS OF THE EYE
Degenerative disorders
Cataract
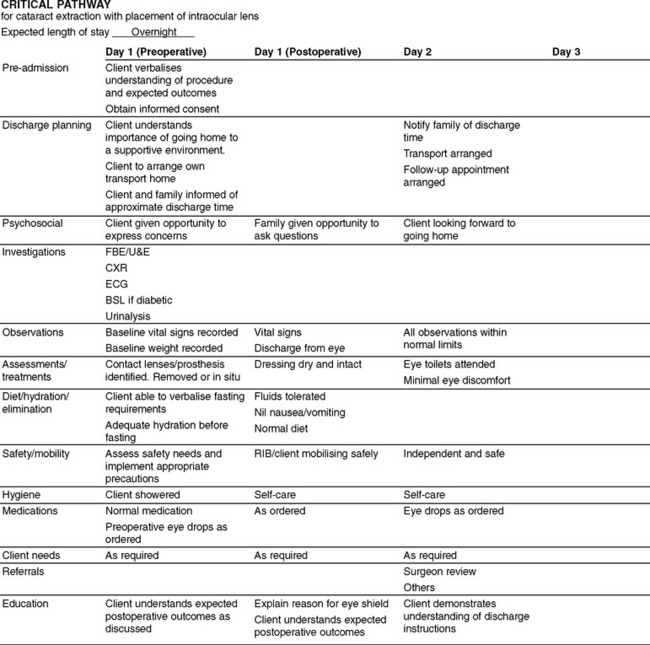
A cataract is a clouding of the lens of the eye. Cataracts generally develop bilaterally, with each progressing independently, with the exception of congenital and traumatic cataracts. Causes include the ageing process, inflammation, malignancy, metabolic factors, toxins, heredity and trauma. Manifestations generally begin with a decrease in visual acuity. The client complains of not being able to see clearly. They may also complain of blurred vision, glare and a decrease in colour perception. As the cataract progresses, the pupil appears milky white. Surgical removal of the cataract from the lens is indicated when activities of daily living are affected. Figure 42.5 outlines a sample critical pathway for a client having a cataract extraction.
Infectious disorders
Blepharitis
Blepharitis is inflammation of the eyelid margins. It may be caused by bacterial infection or an allergic reaction to smoke, dust or chemical. Seborrhoea, a disorder of the sebaceous gland, may also cause blepharitis. Manifestations include itching, burning, redness of the eyelid margins, chronic conjunctivitis and yellow purulent discharge crusts on the lashes.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree