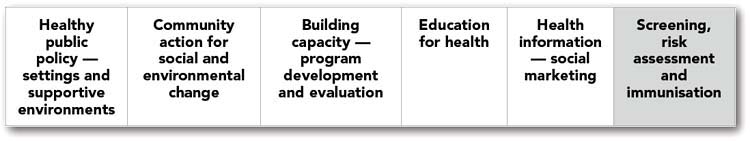
CHAPTER 9 Screening, risk assessment, immunisation and surveillance
In Chapter 9 we move to the far end of the continuum of health promotion approaches outlined in Chapter 1 and examine some of the medical approaches to health promotion. There is a range of strategies used in this approach. The four best known medical approaches to health promotion are: immunisation; screening for specific diseases, including non-communicable diseases; individual risk factor assessment; and surveillance.
When the medical approach to health promotion is used alone, it is known as selective Primary Health Care. Selective Primary Health Care is more limited than comprehensive Primary Health Care, discussed in Chapter 1, because control over health is maintained by health professionals who often concentrate on disease and do not necessarily take the social context of people’s lives into consideration. When we only address disease, we risk continually trying to fix the end result of the problem instead of addressing the root causes of diseases or the social conditions that perpetuate disease and other suffering.
IMMUNISATION, SCREENING, INDIVIDUAL RISK FACTOR ASSESSMENT AND SURVEILLANCE
Immunisation
Some vaccination programs are more acceptable to vulnerable population groups or parents than others and these factors will have an impact on vaccination rates. For example, research concerning the acceptability of vaccines for sexually transmitted infections demonstrated that perceived susceptibility of the disease and perceived benefits of receiving a vaccine to prevent a disease were important factors to consider (Dickson-Swift et al 2008). Cost, efficiency, physician recommendation, attitudes towards vaccination, knowledge, parental approval and geographical location are also important factors in the acceptability of vaccines (Dickson-Swift et al 2008). These potential barriers and enablers to vaccine up-take, and obtaining a sufficient pool to prevent a disease, need to be taken into consideration in developing immunisation programs.
Screening
Effectiveness of screening
There is controversy over the effectiveness of some screening procedures. For example, while the benefits of mammography screening for women over 50 years of age have been demonstrable, screening for younger women is disputed, and further there is no evidence that breast self-examination is effective in reducing mortality from breast cancer (Weller 1997 in Baum 2008). Prostate and colorectal cancer screening is also contested (Baum 2008).
 leads to over-detection and over-treatment
leads to over-detection and over-treatment
 may include invasive follow-up investigations and treatments
may include invasive follow-up investigations and treatments
 harm is immediate and benefits are delayed
harm is immediate and benefits are delayed
 few people experience benefits from screening compared with the number who would be expected to benefit from most treatments
few people experience benefits from screening compared with the number who would be expected to benefit from most treatments
 individual values and preferences are critical to screening decision-making
individual values and preferences are critical to screening decision-making
 evidence base for screening decision aids is often limited
evidence base for screening decision aids is often limited
 public attitude is that early detection and or prevention must be good
public attitude is that early detection and or prevention must be good
 little regulation is in place to protect consumers from aggressive marketing, and there may be strong financial incentives to get people to participate in screening.
little regulation is in place to protect consumers from aggressive marketing, and there may be strong financial incentives to get people to participate in screening.
 present the chances of having pseudo-disease as well as clinically important disease detected by screening
present the chances of having pseudo-disease as well as clinically important disease detected by screening
 give information about the whole of the early detection and treatment process
give information about the whole of the early detection and treatment process
 present balanced information about the cumulative chance of benefits and harms over equivalent time frames
present balanced information about the cumulative chance of benefits and harms over equivalent time frames
 present very small numbers by using large and consistent denominators, for example, outcomes per 1000 or per 10 000 people screened
present very small numbers by using large and consistent denominators, for example, outcomes per 1000 or per 10 000 people screened
 screening decision aids need to accommodate flexibility in labelling the outcomes of screening as benefits or harms
screening decision aids need to accommodate flexibility in labelling the outcomes of screening as benefits or harms
 explicitly declare where high quality evidence is lacking
explicitly declare where high quality evidence is lacking
 use ranges or some other method to convey uncertainty in numerical estimates
use ranges or some other method to convey uncertainty in numerical estimates
 explain that there is a choice and the reasons why people might decide to decline screening
explain that there is a choice and the reasons why people might decide to decline screening
 information about financial gains to the organisation offering the screening test may need to be included in decision aids.
information about financial gains to the organisation offering the screening test may need to be included in decision aids.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree