Chapter 26 SAFETY AND PROTECTION
FACTORS AFFECTING THE SAFETY OF CLIENTS
AGE
Not all adolescents take part in these behaviours. Many have a strong grasp on, and accept and practise, the rules and laws that are designed to protect everyone in the community; for example, don’t drink and drive, don’t drink alcohol and swim, wear a seatbelt in the car. Young people in the years leading up to and during adolescence can be kept safe from these specific dangers if they receive appropriate information and guidance about how to say no to drugs, choices about abstinence from sexual activity or how to practise safe and effective birth control. They need to be able to discuss and ask questions about these issues in an environment where they feel comfortable to do so. Nurses are frequently in the position to practise health promotion by teaching safety measures, answering questions and facilitating discussion with adolescents in the health care setting.
Young and middle-aged adults tend to be at a level of risk according to their lifestyle practices. For example, a high-fat diet, smoking and lack of exercise increase the risk of respiratory and cardiovascular disorders and cancer. The types of leisure activities indulged in, particularly sports, are often linked to injury in this age group. Workplace injuries are also common, particularly in males and particularly among tradesmen. The risk of being involved in a motor vehicle accident also remains significant (Australian Bureau of Statistics 2005).
As a normal part of ageing, older adults may experience physiological changes, including decreased muscle strength, diminished sensory acuity and slowed reflexes. Many older people adapt successfully and modify lifestyle practices to accommodate the physical changes of ageing, but statistics indicate that getting older does increase the risk of accident and injury. For example, injury from falls becomes much more common in adults over age 65. The rate of individuals needing medical attention as a result of falls is higher in residential care and hospital settings than in the community generally (National Ageing Research Institute 2004).
ELDER ABUSE
Abuse of older people is a safety issue that nurses need to be aware of when assessing clients. Elder abuse, particularly of those who have dementia, is sometimes related to the actions of family carers who are so tired and stressed by the hard and constant work of caring that their tolerance level reaches zero. Carers are often ashamed or too embarrassed to ask for help, and clients often do not have the courage or privacy needed to speak out about what is happening to them (Faye & Sellick 2003). Nurses must be alert for signs and symptoms of abuse when assessing clients (see Chapter 23) and recognise when family carers might need interventions such as regular periods of respite.
INTELLECTUAL, MENTAL OR PSYCHOLOGICAL IMPAIRMENT
Sometimes clients may have a condition that leads them to harm themselves. Examples of self-harming behaviour include self-inflicted wounds such as cuts or burns, ingesting or injecting poisonous substances, or inserting objects into body orifices. Close monitoring is required in such cases to protect the client from self-harm (see Chapter 45). Behaviours such as these have been associated with what mental health nurses might call ‘disabling distress’ — behaviour that results from serious unresolved anxiety (Watkins 2001). Any circumstance or condition that increases anxiety may interfere with a person’s normal pattern of behaviour. It does not, in most situations, lead to self-harm, but it is not uncommon for anxiety to lead to feelings of utter panic. People who are anxious or experiencing feelings of panic can sometimes react to situations with such intensity that clear thinking and logical responses to what is happening are impossible. These individuals may experience levels of anxiety so severe that it affects their perception of, and ability to react appropriately to, the threat of harm. (Chapter 13 discusses nursing responses to anxiety and panic.)
RISK ASSESSMENT AND MANAGEMENT
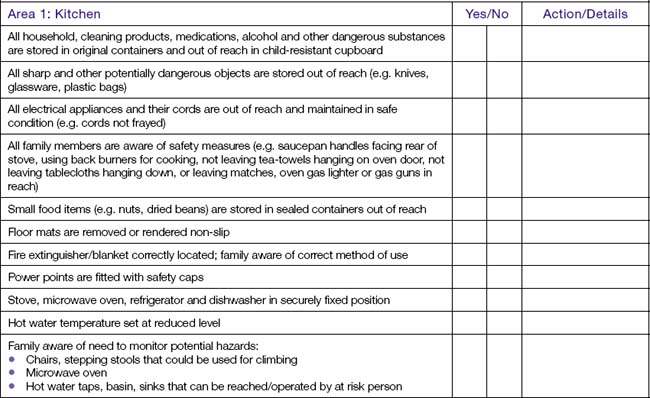
The goal of nursing practice in relation to the need for safety is to prevent injury or harm. Nurses need to assess potential risks then plan interventions that can prevent accidents that are often the cause of injury or harm to clients. The nurse assessing potential risks to safety in relation to young children or at-risk clients living at home needs to check the entire house and garden area. Organisations responsible for community health frequently have assessment tools designed to aid the assessment of home safety. Clinical Interest Box 26.1 provides an example of one part of an assessment tool used to assess home safety. The example provided relates to checking for safety risks in a home kitchen.
Nursing interventions need to be considered in relation to the level of risk that a client faces and the impact of the intervention on social benefits and enjoyment of life. People balance risk against the pleasure or sense of achievement they will gain when they make choices about what activities they will pursue throughout life: there is a level of risk in many leisure and work activities. Whenever possible, clients should continue to be given the opportunity to consider the risks they face and make informed choices about which interventions are in their best interests. For example, a nurse visiting a client at home may be very concerned about the number of times the client has tripped over a lively pet dog. The nurse may consider the potential for serious injury is high but, even when the risks and possible outcomes are explained, the client may choose to live with the risk of tripping over the dog again and suffering an injury rather than losing the pleasure and sense of security provided by the pet.
Often risk assessment presents difficult decisions; for example, the person who has swallowing difficulties and is at risk of choking may prefer to take the risk of eating and drinking substances they enjoy, even when they increase the risk of choking. Decisions are especially difficult when the person who is at risk is deemed not competent to make an informed decision, as may be the case with people who have intellectual or cognitive impairment (Clinical Interest Box 26.2). The nurse should discuss risk assessment issues with other members of the health care team and clearly document all related discussions with the client in situations such as these.
CLINICAL INTEREST BOX 26.2 FRANK AND MARY’S STORY
(story told by Frank, 77, carer of Mary, who had Alzheimer’s dementia and died aged 76)
It is the nurse’s role to assess the client and the client’s environment for hazards that are a potential cause of injury, whether the environment is in the home or in a health care facility. Infective microorganisms present a significant threat in health care settings (the safety and protection measures needed to deal with this risk are addressed in Chapter 25). Some of the other most common causes of injury or harm result from thermal injuries, contact with sharp objects, poisons and pollutants, and falls.
COMMON CAUSES OF INJURY
THERMAL INJURIES
Protection from burns and scalds includes protecting clients from the threat of fire and also from everyday risks of thermal injury. Burns or scalds can result from exposure to flame, hot liquids or objects, electrical or gas appliances, or from overexposure of the skin to the direct hot rays of the sun. Serious damage may also occur when the body tissues are exposed to extreme cold. (See Chapter 48 for information about the first aid management of burns, scalds and heat and cold trauma after exposure to the natural environment.)
Many fires and thermal injuries occur in the home. Clinical Interest Box 26.3 identifies safety measures recommended for senior citizens to prevent fire in the home.
CLINICAL INTEREST BOX 26.3 Safety measures recommended for senior citizens to prevent fire inside the home
Children are at particular risk of thermal injury. Not all people recognise areas of risk and the nurse can play an important role in health promotion by educating clients and families about safe practices; for example, the nurse may need to educate parents about ways to prevent thermal injuries to children (Box 26.1).
Box 26.1 Protecting children and other vulnerable individuals from thermal injury in the home environment
Reducing the risk of fire in health care facilities
SHARP OBJECTS
In the event of an injury from a sharp object, such as a needle-stick injury, the incident is reported immediately and documented on an incident report form (see Chapter 20). The level of risk of an infection being transmitted via the needle-stick injury is assessed and the individual treated in accordance with the policies of the health care facility. (See Chapter 25 for information concerning protective measures after possible exposure to blood-borne microorganisms.)
Measures to prevent injury from glass ampoules include:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree