S
Severe acute respiratory syndrome tests
Basics the nurse needs to know
How the test is done
Samples will be collected from various sources in the body where the virus is known to locate.
Interfering factors
NURSING CARE
Pretest
During the test
Posttest
Sickle cell tests
Basics the nurse needs to know
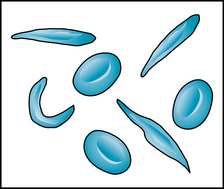
Sickle cell hemoglobin (HbS) is the most common of the variant hemoglobins. The term sickled is used because when there is low level of oxygen in the blood, HbS converts the erythrocytes into sickle or crescent shapes (Figure 87). In sickle cell disease, these damaged erythrocytes carry less oxygen to cells and tissues. Ongoing hemolysis of the damaged erythrocytes also occurs and causes chronic hemolytic anemia throughout life. In a sickle cell crisis, the many sickled cells become trapped in small blood vessels, causing obstruction, infarction, thrombus, or embolus in the circulation, with acute or chronic damage to organs and tissues.
Sickle cell trait or disease is an autosomal recessive genetic disorder. The homozygous (pure) form of HbS causes the disease of sickle cell anemia (HbSS). Abnormal chromosomes that produce hemoglobin S were inherited from both parents. The heterozygous (mixed) form of HbS produces sickle cell trait. The person with sickle cell trait inherited the HbS chromosome from one parent but not the other. The person with the trait condition does not have sickle cell anemia and under normal physiologic conditions will not develop a vaso-occlusive crisis (Pack-Maybien & Haynes, 2009).
How the test is done
Heelstick capillary puncture is used to obtain a specimen of blood from the heel of the neonate.
Capillary puncture in the finger is used for older children and adults.
Interfering factors
NURSING CARE
Nursing measures include care of the capillary puncture site as described in Chapter 2, with the following additional measures.
Posttest
Health promotion
In all states of the United States and its territories, all newborns now have mandated screening for sickle cell disease, regardless of ethnicity (U.S. Preventive Services Task Force, 2007).
Sigmoidoscopy and anoscopy
Basics the nurse needs to know
Sigmoidoscopy uses a flexible, fiberoptic endoscope (sigmoidoscope) to examine the sigmoid colon and rectum. About 50% of colon cancer and polyps of the colon are located in the left colon between the anus and the splenic flexure. During a sigmoidoscopy procedure, the polyps can be removed and suspicious tissue can be biopsied or cultures taken. The examination can be done in the physician’s office, without conscious sedation or pain medication. One of the drawbacks of sigmoidoscopy is that the other 50% of the polyps and cancerous tumors are located between the right colon and transverse colon, beyond the view of the sigmoidoscope. In addition, if a polyp or tumor is encountered by sigmoidoscopy, the patient will need a follow-up colonoscopy to view the remainder of the colon.
There is a low prevalence of anal cancer in the general population. However, there is a rising incidence of anal cancer in HIV-infected men who have sex with men. Testing for the human papilloma virus (HPV) may be done during the anoscopy examination. When indicated, the anal examination can include a male PAP smear and the cell brushings can be examined microscopically for abnormal cytology. The Bethesda system is used to grade the anal cytologic changes (see Box 8, p. 471). A biopsy will be taken of anal cells that are graded as high-grade dysplasia (precancerous) or cancerous for a definitive diagnosis.
How the test is done
The patient is placed in a lateral position on the examination table (Figure 88). The well-lubricated instrument is inserted into the anus and advanced to the desired depth. A tissue biopsy, PAP smear, or culture specimen may be obtained during the procedure. The time needed for the examination is 5 to 10 minutes.
Interfering factors
NURSING CARE
Health promotion
The US Preventive Task Force (2008) recommends that colorectal screening can be done by fecal occult blood test, flexible sigmoidoscopy, or colonoscopy. For the average-risk individual, the recommended routine screening schedule for adults should begin at age 50 and continue to age 75. They also recommend against routine screening for colorectal cancer for asymptomatic people aged 76 to 85 because the net benefits are small, and against routine colorectal screening of asymptomatic adults older than 85 because the benefits of screening do not outweigh the harm. The American Cancer Society recommends that asymptomatic adults have colorectal cancer screenings starting at age 50. The screening options are flexible sigmoidoscopy, double-contrast barium enema, or computed tomography colonography every 5 years or colonoscopy every 10 years (Wilkins & Reynolds, 2008).
Health promotion
The nurse can help teach people of the importance of colorectal cancer screening. The onset of this disease is usually after age 50 and the risk of developing colorectal cancer increases with each decade thereafter. Screening offers prevention by removal of polyps before they become cancerous and early detection of a tumor before symptoms occur. Prevention and early intervention for colorectal cancer has a higher rate of cure.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree