Chapter 35 Osteoarthritis (at least 75% of cases), which is also called degenerative joint disease (Fig. 35-1). Osteoarthritis typically occurs in those older than age 40 years and has few signs of inflammation on examination, thus the joints are not hot, red, or tender like in the other four types of arthritis listed earlier. Look for Heberden nodes (visible and palpable distal interphalangeal [DIP] joint osteophytes; Fig. 35-2) and Bouchard nodes (proximal interphalangeal [PIP] joint osteophytes), worsening of symptoms after use and in the evening, bony spurs, and increasing incidence with age. Treat with weight reduction and as-needed nonsteroidal antiinflammatory drugs (NSAIDs) or acetaminophen.
Rheumatology
1 What is the most common form of arthritis?

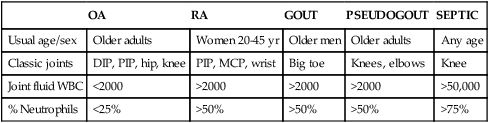
3 How do you distinguish among the common causes of arthritis?
OA
RA
GOUT
PSEUDOGOUT
SEPTIC
Usual age/sex
Older adults
Women 20-45 yr
Older men
Older adults
Any age
Classic joints
DIP, PIP, hip, knee
PIP, MCP, wrist
Big toe
Knees, elbows
Knee
Joint fluid WBC
<2000
>2000
>2000
>2000
>50,000
% Neutrophils
<25%
>50%
>50%
>50%
>75%
4 What other clues point to a diagnosis of osteoarthritis?

Nurse Key
Fastest Nurse Insight Engine
Get Clinical Tree app for offline access














