INTRODUCTION
When the new student nurse is first identified as ‘a nurse’ by their home community everyone appears to make a mental note, so that when an emergency occurs friends and relatives know where to turn for help. This general principle appears to apply equally to all nurses, including those who have specialized in diverse areas of practice, as many members of the public only recognize the traditional general nurse, and all nurses are expected to fill this role. How the nurse fulfils their role in the emergency situation when called to help as ‘a nurse’ has many implications. While it is important to begin by addressing the nursing knowledge needed to support the provision of resuscitation and emergency care, this chapter also focuses upon issues surrounding how the nurse might participate in emergency. Although remaining mostly in the same order to others in the book for convenience of reading, some components of psychosocial knowledge can be found within the section on professional knowledge. This is because many elements of the two sections are combined in this subject, needing to be considered together. This also allows for logical consideration of physical emergency care. It is, however, important to move through the chapter to remind yourself about the implications of participating in care at the same time as determining how you might do this and what types of knowledge you might need.
SUBJECT KNOWLEDGE
UNDERLYING PRINCIPLES OF EMERGENCY PHYSIOLOGY
Please revise the homeostatic mechanisms described in Chapter 7 before continuing with the following section.
Before considering the practicalities of resuscitation, it is important to have an understanding of the potential mechanism of sudden collapse so that a more logical approach can be made. The Resuscitation Council Guidelines (2005) have a basic assumption which is worth mentioning: that is, the most common cause of non-traumatic sudden pulseless collapse in adults is cardiac in origin, and more specifically ventricular fibrillation (VF), which will be described further in the next section. ‘Collapse’ can be defined as ‘a potentially reversible, sudden and unexpected loss of normal consciousness’ (sometimes this follows a period of deterioration). In infants and children, as we will see later, the situation is usually different, hence there is a different set of guidelines for them. The primary cause of non-traumatic collapse in children is classically of respiratory origin.
THE CARDIAC COLLAPSE
The heart and ventricular fibrillation
The heart is a four-chambered organ situated centrally and slightly to the left in the chest, behind the sternum (Figure 4.1 and Figure 4.2).
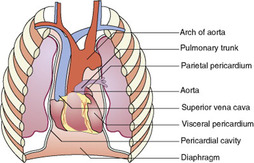 |
| Figure 4.1 (adapted from Montague et al 2005, with kind permission of Elsevier). |
 |
| Figure 4.2 (from Montague et al 2005, with kind permission of Elsevier). |
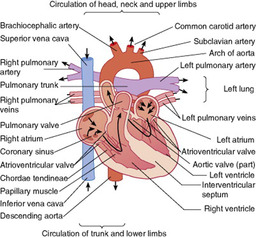
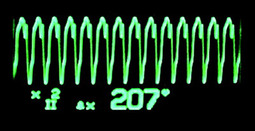
A characteristic of cardiac muscle is its ability to contract in the absence of any external stimulation. This independent mechanism is coordinated by a unique electrical system within the heart, which results in a coordinated contraction of the heart muscle. This is sinus rhythm (Fig. 4.3) – a regular, coordinated cardiac rhythm producing a palpable pulse.
Figure 4.3 is a representation of the normal electrical activity of the heart as measured by skin electrodes and a cardiac monitor. This is an electrocardiograph or ECG.
Referring to a physiology textbook, explain the pattern in relation to the way the electrical activity coordinates cardiac muscle contraction. Remember that this is only an indication of electrical activity and it does not necessarily relate directly to mechanical function.
 |
| Figure 4.3 |
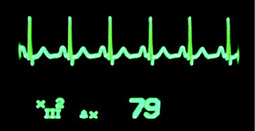
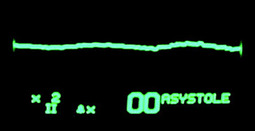
When the normal electric conduction system in the heart fails because of ischaemic heart disease (IHD), instead of stopping ‘dead’ (known as asystole; Fig. 4.4), each muscle fibre independently contracts and relaxes, giving the heart a shivering appearance: this is ventricular fibrillation (VF; Fig. 4.5). Although the heart is active there is no effective pumping action, therefore the collapsed individual will have no pulse and will quickly lose consciousness.
 |
| Figure 4.4 |
 |
| Figure 4.5 |
The significance of VF is the relative simplicity of treatment – passing an electric discharge over the heart (known as defibrillation) will often terminate a chaotic rhythm and (hopefully) allow a return to a spontaneous rhythm. The key factor in the success of the process of defibrillation is time. The longer the delay between the onset of VF and treatment by defibrillation, the worse the outcome. While the patient is in VF there is no coronary circulation and therefore no myocardial oxygenation, so the patient deteriorates rapidly. It is unlikely that basic life support (BLS) resuscitation is very efficient in maintaining an effective coronary circulation. It does, however, buy the patient time until further help is available.
During VF the lack of oxygen supply to the cardiac muscle results in the VF activity becoming less ‘strong’ or ‘coarse’ with time and eventually decaying to asystole.
Asystole (Fig. 4.4) is the classic ‘straight line’ (which, if you look carefully, is not really straight) on the cardiac monitor that is frequently used in films and TV soaps. Asystole indicates no apparent cardiac electrical activity and commonly occurs as a result of prolonged hypoxia or another significant illness. In practice, apparently well patients do not usually suddenly collapse into asystole as presented by the media.
The third rhythm (and the second requiring defibrillation) is pulseless ventricular tachycardia (with an emphasis on the word ‘pulseless’). Within normal limits, as the heart rate increases, so does the cardiac output (rate × stroke volume); however, at very high pulse rates stroke volume will drop due to inadequate time for the heart to refill. As the heart rate increases a patient will initially become dizzy (cerebral hypoxia) and will show progressive symptoms of collapse as the blood pressure falls. Ultimately the patient will present as a cardiac arrest even though a connected electrocardiograph (ECG) will show a very rapid ventricular rate (Fig. 4.6).
 |
| Figure 4.6 |
Pulseless electrical activity (PEA) is the fourth rhythm associated with cardiac arrest (Fig. 4.7). In this situation, the nurse will see a rhythm on the cardiac monitor which is normally expected to be associated with a cardiac output, but no palpable carotid pulse is found on examining the patient. Essentially, the electrical conduction system within the cardiac muscle is functioning but there is no associated cardiac output (hence PEA). It is most often found in hospital patients after a period of deterioration. In the simplest situation, when a patient has lost most of the circulating blood volume, the heart will continue to work while it is still oxygenated, but no significant amount of blood will be circulated. There are several causes of PEA, including hypovolaemia (fluid loss, including bleeding and dehydration), severe pneumothorax (collapsed lung), hypothermia (low body temperature) and electrolyte imbalance in the blood and intracellular fluids. All these situations occur in adults and children, so both groups can present with PEA.
 |
| Figure 4.7 |
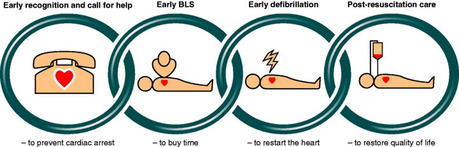
THE CHAIN OF SURVIVAL
The ideal survival scenario from ventricular fibrillation was first described by Cummins et al (1991) in the ‘chain of survival’ concept, further updated by the Resuscitation Council (UK) (2005), indicating the links required (Fig. 4.8). Following these stages can help guide you through the emergency situation. However, you will need further skills training to become competent in all aspects:
• Early BLS slows deterioration.
• Early defibrillation (when appropriate) is the key to reversing the situation.
• Finally the provision of post-resuscitation life care to stabilize the patient and promote recovery.
 |
| Figure 4.8 |
As the VF scenario is potentially so treatable, this is the target of the adult resuscitation guidelines. Conveniently, all other medical emergencies are also reasonably managed by these guidelines.
THE COLLAPSED CHILD: DOES AGE MATTER?
Sudden collapse can occur in any victim of any age. Consideration must be given to the changes in anatomy and physiology between birth and adulthood as this requires a different approach in resuscitation skills (see Evolve 4.1).
The causes of collapse in infants (under 1 year old) and children (1–8 years old) are usually respiratory problems and resulting hypoxia rather than the cardiac problems found in adults, as degenerative heart disease is not common in children (Nadkarni et al 1997). This is due to the growing respiratory system, see below. Cardiac failure in children and infants rarely occurs as an initial problem and is usually linked to congenital cardiac abnormalities.
• The normal physiological parameters of children and adults.
• Different physiological responses of children and adults to emergency and traumatic situations.
• How you can use this information in identifying potential emergency situations in your practice.
The National Audit of Paediatric Resuscitation (NAPR) Study records out-of-hospital cardiopulmonary events (Resuscitation Council 2006); by July 2006 the sample stood at 642. The findings are as follows:
| Cardiac | 27% |
| Respiratory | 25% |
| Trauma | 12% |
| Sudden infant death syndrome (SIDS) | 9% |
| Drowning | 5% |
| Threatened airway | 5% |
| Fitting | 1% |
| Other | 16% |
This suggests the amalgamated figure of respiratory events exceeds those of a cardiac nature. However, events leading up to the cardiac and respiratory situations were not recorded so the actual cause is not clear.
The greatest mortality during childhood occurs in the first years of life. Causes include congenital problems, prematurity and infection due to the immature immune system. Sudden infant death syndrome (SIDS) remains the main cause of death in infants aged between 1 month and 1 year, although the guidelines on positioning infants have reduced this number considerably (Department of Health, 1992, Coyne, 1996 and SIDS 2008). In children over 1 year of age, trauma is the most frequent cause of death (Child Accident Prevention Trust 2008). Choking is the third most common cause of childhood death; the Child Accident Prevention Trust (CAPT; 2008) states that in 2005, 16 children under 15 years of age died as a result of choking, and 12 children under 5.
Children who have had an out-of-hospital cardiac arrest and arrive in accident and emergency departments not breathing and pulseless have a poor outcome due to the brain damage resulting from lack of oxygen. There are three potential outcomes of child arrest: survival, survival with neurological insult or death (Advanced Life Support Group 2005).
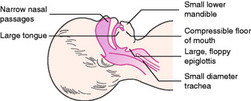
The respiratory system (Fig. 4.9) in children continues to develop until approximately 8 years of age. Therefore the following points need to be considered in emergency care:
• Infants tend to breathe only through their nose until the age of 3 months, which adds to the problems of resuscitation as the nasal passages are small.
• The tongue is very large and collapses into the oropharynx easily, thus blocking the airway.
• The lower mandible is small in comparison to the large tongue, which further exacerbates the problem of airway obstruction.
• The diameter of the trachea increases threefold by puberty – the trachea is approximately the same size as the child or infant’s little finger, thus increasing the resistance to air entering and leaving the lungs.
• The epiglottis is floppy and will easily occlude the airway.
 |
| Figure 4.9 (from Advanced Life Support Group 2005). |
The following additional anatomical characteristics should also be borne in mind:
• The cartilaginous rings of the trachea are soft and easily compressed.
• Respiration depends upon movement of the diaphragm as the intercostal muscles are not fully developed and therefore abdominal respirations are observed until at least 6 years of age.
• The left ventricle of the heart does not develop its characteristic thick muscular wall until about 6 months of age, and this affects how well blood circulates around the body because of the limited power of each contraction.
• The basal metabolic rate and oxygen consumption in infants are much higher than in adults resulting in increased heart and respiratory rates, and therefore they are much more prone to hypoxia and resulting neurological damage.
The BLS guidelines are thus based on maintaining oxygenation rather than restoring normal cardiac rhythm. However, without oxygen an infant or child will soon become bradycardic (i.e. have a slow pulse rate) and this will quickly progress to pulselessness.
CARE DELIVERY KNOWLEDGE
ACTION IN AN EMERGENCY SITUATION
Personal safety of the rescuer
The personal safety of the rescuer is an obvious priority, so it is important always to look carefully at any situation before ‘diving in’.
There is never a situation when to consider personal safety first is wrong. Potential hazards can include electricity, gas, fire, water, or a casualty holding a double-barrelled shotgun! While one concern might be that time spent looking carefully at the situation could be ‘wasted’, in fact it only takes about the same time as putting on a pair of disposable gloves, which is probably a good thing to be doing (if they are available) while thinking. Another health and safety consideration is infection control. Although there is much concern in this area regarding first-aider safety, there is little current evidence that this is a great problem as long as the usual universal precautions are followed, for example wearing gloves when handling body fluids (see Ch. 5 on infection control for more information).
Much concern has been raised about the possibility of a rescuer catching the human immunodeficiency virus (HIV) while carrying out mouth-to-mouth resuscitation. At the time of writing the authors of this chapter have heard of no such cases. However, there are other infections that pose a potentially greater risk. Barrier devices (simple protective devices which can be placed on the patient’s face) for use with mouth-to-mouth resuscitation need to be considered by the individual rescuer. In order to make use of such devices, it is essential to be well practised in their use on a mannikin first. The pocket mask (Fig. 4.10) is especially useful, as an oxygen supply can be added to the mask, increasing the percentage of oxygen delivered to the casualty from less than 20% to up to 50%, so making the whole process much more efficient.
Refer to Chapter 5 on infection control and other literature on HIV and its mode of spread.
• List the potential airborne infections that might be a risk to rescuers.
• Review the effectiveness of any methods at present available to reduce risk to the first-aider.
• Review the potential for preventive immunizations from those organisms of high risk.
• Regarding the potential ‘risk’ of mouth-to-mouth breathing in resuscitation, would you socially kiss a new friend without demanding an HIV screen?
 |
| Figure 4.10 |
Assessing help required and establishing priorities
A call for help must include sufficient information to allow the emergency services coordinator to produce a full and adequate response (i.e. it is important to know the number and nature of the casualties). If this information is not accurately provided it will be up to the first emergency services vehicle to fulfil this role, resulting in a further delay. Clearly if a bystander is available this role can be delegated, but confirmation that the call has been made must be ensured.
Most acute hospitals have an emergency team who provide internal emergency support, for example the cardiac arrest or critical care outreach team. The UK NHS national internal emergency number is 2222, but check that this applies where you work (some smaller hospitals with limited internal emergency support may use the UK 999 system).
You are the first person to arrive at the scene of a road traffic accident where two cars have hit each other. In the first car the elderly male driver has severe chest pain and a minor head injury. On the back seat of the car is a 30-year-old female with profound learning disabilities who is screaming loudly. In the second car the female driver is bleeding badly from an arm laceration. In the passenger seat of the second car lies an unconscious baby.
• How might you initially deal with the situation, assuming no help is available?
• What information will it be necessary to give the emergency services when you make your 999 call or direct a passer-by to do so?
ASSESSING THE CRITICALLY ILL PATIENT
The early detection and prevention of collapse
Survival from the pulseless collapse remains poor despite advances in the science of resuscitation and hence there is increasing interest in preventing cardiac arrest and in the determination of risk factors.
Hodgetts et al (2002) point out the potential advantages of a designated emergency team to attend to deteriorating patients prior to a cardiac arrest. Often it is fairly difficult to quantify events such as ‘nurse concern’ which occur prior to the eventual collapse; the most important observation for nurses is the routine measurement of respiratory effort and rate.
Recognition of the critically ill victim follows a quick assessment process focusing on the physical assessment of the victim by the healthcare professional. This assessment can be found in the advance life support (ALS) manuals for both adults and children. This simple process formulates the information regarding the victim in a format that is clearly understood by nursing and medical staff.
The general ABC approach is described well in the BLS guidelines which will follow later in the chapter. After this initial assessment, a more comprehensive assessment can be undertaken.
For the acutely ill or injured patient an ABCDE approach is taken. There are many versions of this approach, targeting different levels of expertise (notably Smith et al 2002). The principles are that ABCDE identifies the priorities in order of significance, each major problem being managed before moving on to the next stage. However, if there is a need to deal with a priority, the whole examination should be continued, completed and repeated, as soon as possible.
The ABCDE (and potentially FGH) assessment
The process described below follows an ‘ABC’ quick approach followed by a more detailed (and potentially slower) ‘ABCDEFGH’ approach; this has been found to be helpful for less experienced healthcare staff.
The initial ABC quick approach focuses on the primary assessment to identify whether the patient requires immediate resuscitation, followed by a more detailed approach if this is not required.
Conscious?
An initial general assessment of the patient’s consciousness level should be made by calling to them and gently shaking the shoulder (depending on potential injuries). The following assessment can then be undertaken:
Airway (A)
General issues will be considered first, and then variations to this process for specific situations.
The unresponsive casualty may not breathe unless he or she has a patent airway. Although it is not physically possible to swallow the tongue, this phrase is often used to describe the relaxed tongue dropping into and blocking the posterior pharynx. The manoeuvres described aim to relieve this obstruction. When opening the airway, the position of the lower jaw is at least as important as the head tilt (Fig. 4.11), especially the need to realign it into its normal functional position with the upper and lower teeth on the same plane. (NB: Remember the specific needs of infants discussed in the physiology section earlier.)
 |
| Figure 4.11 |
A brief simultaneous look into the mouth may show food debris (and hence a risk of airway obstruction) or other airway abnormality.
An additional manoeuvre is the jaw thrust (Fig. 4.12). The idea for this is to bring the lower jaw upwards – along with the jaw will come the attached tongue, thus clearing it from the airway. This is an especially important manoeuvre if the casualty has a potential neck injury, in which case it can be used alone without the head tilt manoeuvre (Fig. 4.11), which could cause further damage.
 |
| Figure 4.12 |
Breathing (B)
Airway opening must be maintained when assessing breathing. While assessing breathing, the patient could be making a purposeful respiration, have gasping/agonal (uncoordinated) breathing or not breathing at all.
Observation should be of the chest wall in older children and adults, whereas for children under 6 years the focus should be on the abdomen as the diaphragm is the dominant respiratory muscle. The healthcare professional should be aware of the normal respiratory rates for infants, children and adults. The significance of gasping and agonal breathing is that it indicates that there is lack of control of breathing and this is inadequate to maintain normal oxygen levels; therefore it is treated as not breathing.
Ultimately, the rescuer needs to decide whether the patient’s breathing is adequate – if it is not, then support is required.
Circulation (C)
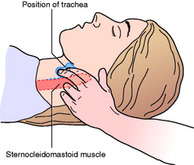
When checking the circulation, the only appropriate pulse to initially check is the carotid pulse, as the peripheral pulses are unreliable indicators in the collapsed patient (they can disappear as a result of normal blood pressure homeostasis). In order to prevent uncertainty when the rescuer is anxious and adrenaline levels are high, the carotid pulse is best felt via anatomical landmarks rather than by guesswork. On the patient’s neck the trachea and the sternomastoid muscle should be palpated. The fingers should be placed in the trough between these two structures in the mid-neck region and pressure exerted by the tips of the fingers until they reach the bottom of the trough (Fig. 4.13). This should be performed on the side nearest the first-aider to avoid occluding the trachea. When practising this exercise, it is essential to press on one side only, or fainting may be caused as a result of reducing blood flow to the brain; equally the rescuer should not press too hard as this will stop the blood flow if the blood pressure is low.
 |
| Figure 4.13 |
Handley et al (1997) comment that the practice of the pulse check may be a less than reliable technique, especially by lay first-aiders, and perhaps the expression ‘look for signs of a circulation’, which includes a more general assessment of circulation as well as a pulse check, is more appropriate.
If unsure and the patient appears effectively ‘dead’, the rescuer should commence chest compressions. Because time is very limited this needs to be undertaken quickly. There is no evidence that ‘inappropriate’ chest compressions stop the heart and if you review the approach of advanced life support, chest compressions are used to initially support the heart which has recently restarted.
In infants, because of the short neck, the initial pulse assessment is made using the brachial artery, which is found just medial (towards the centre of the body) to the biceps tendon in the antecubital fossa (the front of the elbow).
Disability (neurological) (D)
Although the Glasgow Coma Scale is generally used in hospital, it is time-consuming to apply and requires regular practice; a faster and more straightforward system is the AVPU system (Box 4.1), which is widely used in pre-hospital care. The rescuer simply records the patient’s best response.
Box 4.1
| A | Alert | Patient fully responsive, eyes are open without prompting |
| V | Voice | Patient drowsy, eyes only open to command |
| P | Pain | A painful stimulus (applying a finger squeeze to the trapezius muscle) is required to elicit a response from the patient |
| U | Unresponsive | No response |
If the patient is in pain an assessment can be made here (see Ch. 11, pp. 256–257, for pain assessment structures).
Exposure (environment) (E)
The patient should be fully examined from top to toe to detect any physical injuries or abnormalities. The patient’s temperature should be recorded here.
F, G and H
These are not found in traditional systems and integrate into the above but they may be useful reminders for the less experienced rescuer.
Function (F)
Pertaining to limb injuries (which are often involved). Is there a peripheral circulation? (Can a peripheral pulse be found, are the fingers/toes warm?) Has the patient normal sensation and is there a full range of movements?
Glucose (G – included in D with other systems)
Low blood glucose (hypoglycaemia) is a relatively common cause of altered consciousness or behaviour and should be investigated. And while we are on the subject of the patient’s concurrent health problems – do they have any other health related conditions?
History (H)
If the assessment is still unclear, revisit the history of the incident (mechanism of injury) and find out how the patient has been in the previous day/hours to see if there are any other clues.
Outreach teams and medical emergency teams (MET)
A driver for enhancing the skills of ward staff regarding recognition of critically ill adults was the Department of Health’s report Comprehensive Critical Care (2000). Many trusts have taken this development on board as the evidence supports the proposed changes. Priestley et al (2004) found a significant difference in mortality before and after the implementation of a critical care outreach service for adult in-patients. Tibballs et al (2005) found that with the implementation of a medical emergency team, the risk of ill children having a cardiopulmonary arrest on the ward was reduced and the number of calls from nurses requesting an assessment of the child increased. A critical component of outreach and MET is knowing when they should be called. This has led to the development of early warning systems for both adults and children. Use  4.3 to find out more.
4.3 to find out more.
 4.3 to find out more.
4.3 to find out more.INTERVENTION
Resuscitation guidelines
The aim of the BLS guidelines is to produce an accurate and rapid diagnosis, ensure appropriate help is summoned and limit the effects of hypoxia (lack of oxygen).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access


