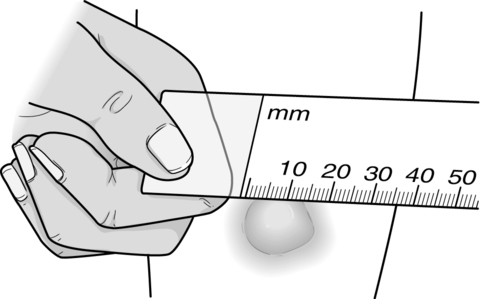
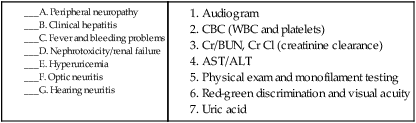
1. What is TB, and what microorganism causes it? 2. What is the route of transmission for TB? 3. The Centers for Disease Control and Prevention (CDC) recommends screening people at high risk for TB. List five populations at high risk for developing active disease. 4. Describe the two methods for TB screening. 5. How do you determine whether a Mantoux test is positive or negative? 6. What additional information would you want to obtain from B.A. before interpreting her skin test result as positive or negative? 7. Determine whether B.A.’s skin test is positive or negative. 8. B.A. asks you what a positive PPD result means. How will you respond? 9. What steps will need to be done to determine whether B.A. has an active TB infection? 10. What is a latent TB infection (LTBI)? 11. What parameters are used to determine whether treatment should be initiated for LTBI? 12. According to the most current CDC guidelines, what constitutes usual preventive therapy for LTBI? 13. Different medications are associated with different side effects. Identify the test used to monitor each possible side effect listed as follows: 14. Nonadherence to drug therapy is a major problem that leads to treatment failure, drug resistance, and continued spread of TB. The CDC recommends two methods to ensure compliance with medication for all patients who have drug-resistant TB and for those who take medication two or three times every week. Identify one of those methods. 15. What information should B.A. receive before leaving the clinic? 1. Are these orders appropriate for M.N.? State your rationale. 2. What gastrointestinal complication might result from one of the medications listed in M.N.’s orders? Four hours after admission, the nursing assistive personnel (NAP) reports to you the following: 3. Based on her vital signs, what do you think could be happening with M.N., and why? 4. You know M.N. is at risk for postoperative pneumonia and atelectasis. What is atelectasis, and why is M.N. at risk? 5. Describe the assessment you would need to perform to differentiate what might be occurring with M.N. 6. Describe four actions you would take next in the next few hours. 7. Outline nursing interventions that are used to prevent pulmonary complications in patients undergoing abdominal surgery. 8. To promote optimal oxygenation with M.N., which action(s) could you delegate to the NAP? (Select all that apply.) a. Reminding the patient to cough and deep breathe b. Instructing the patient on the use of IS c. Assisting the patient in getting up to the chair d. Taking the patient’s temperature and reporting elevations e. Encouraging the patient to splint the incision 9. Identify three outcomes that you expect for M.N. as a result of your interventions. 10. M.N.’s sister questions you, saying, “I don’t understand. She came in here with a bad gallbladder. What has happened to her lungs?” How would you respond? 11. Despite your interventions, 4 hours later M.N. is not improved. Using SBAR, what would you report to the physician? 12. The physician orders a CXR. Radiology calls with a report, confirming that M.N. has atelectasis. Will that change anything that you have already planned for M.N.? Explain what you would do differently if M.N. had pneumonia. 2. Identify two of the main types of apnea, and explain the pathology of each. 3. Identify at least five signs or symptoms of obstructive sleep apnea (OSA), and star those symptoms that S.R. is experiencing. 4. What tests help the provider diagnose OSA? 5. S.R. and his wife ask why it is so important to determine whether or not S.R. has OSA. You would tell them that properly diagnosing OSA is important because effective treatment is necessary to prevent which common complications of OSA? (Select all that apply.) 1. Are B.T.’s vital signs (VS) acceptable? State your rationale. 2. What is the pathophysiology of asthma? 3. How is asthma categorized? Describe the characteristics of each classification. 4. Interpret B.T.’s arterial blood gas results. 5. What is the rationale for immediately starting B.T. on O2? 6. You will need to monitor B.T. closely for the next few hours. Identify four signs and symptoms of impending respiratory failure that you will be assessing for. 7. What is the rationale for the albuterol 2.5 mg plus ipratropium 250 mcg nebulizer treatment STAT (immediately)? 8. Identify the drug classification and expected outcomes B.T. should experience through using metaproterenol sulfate (Alupent) and Fluticasone (Flovent). 9. B.T. stated he had taken his Advair that morning, then again when he started to feel short of breath. Is fluticasone/salmeterol (Advair) appropriate for use during an acute asthma attack? Explain. 10. What are your responsibilities while administering aerosol therapy? 11. When combination inhalation aerosols are prescribed without specific instructions for the sequence of administration, you need to be aware of the proper recommendations for drug administration. What is the correct sequence for administering B.T.’s treatments? 12. List five independent nursing interventions that may help relieve B.T.’s symptoms. 15. What common mistakes has B.T. made when using the inhaler? 16. What would you teach B.T. about the use of his MDI? 17. B.T.’s wife asks about the possibility of B.T. having another attack. How would you respond? 18. B.T. states he would like to read more about asthma on the Internet. List three credible websites you could give him. 1. As the intake nurse, what routine information do you want to obtain from L.B.? 2. L.B.’s chief complaint is a cough. What are the main causes of chronic cough, and what questions should you ask to elicit information about each cause? 4. The provider orders a predilator and postdilator pulmonary function test (PFT). What is the purpose of completing the PFTs predilator and postdilator? 5. The diagnosis of asthma is confirmed, and L.B. returns to the clinic for asthma education. What topics will you address? 6. What is a PFM? Give L.B. precise instructions to perform the PFM maneuver. 7. L.B. asks why she has to use the PFM. Explain the purpose of the peak expiratory flow rate (PEFR) measurement and what role it plays in L.B.’s self-management of her asthma. 8. The provider ordered triamcinolone (Azmacort) two puffs bid and albuterol (Ventolin) two puffs q6h prn. What points will you include when teaching L.B. about her medications? 9. L.B. asks, “Why do I have to use this inhaler? Can’t I just take some different pills?” Your response to L.B. is based on the knowledge that the inhalation route is: a. Safer and more effective than pills b. Less expensive than combination therapy c. Easier to master than oral therapy 10. You instruct L.B. in the proper use of the metered-dose inhaler (MDI) using a spacer. How would you explain proper MDI use? 11. Because L.B. is taking two puffs twice daily of triamcinolone (Azmacort), how long should the inhaler last? The canister label states that it contains 200 inhalations. 12. What will you teach L.B. to do if her PEFR value falls? 13. You would recognize the need for additional teaching if L.B. says: (Select all that apply.) a. “I will use the albuterol inhaler thirty minutes before exercising.” b. “My husband needs to know what to do in case I have an attack.” c. “I will keep a diary of all of my PEFR measures.” d. “I will place a plastic cover on our mattress and my pillows.” e. “The bed linens need to be washed in cold water to reduce dust mites.”
Respiratory Disorders
Scenario
Case Study Progress
Case Study Progress
Scenario
Case Study Progress
Case Study Progress
Scenario
Case Study Progress
Scenario
Case Study Progress
Scenario
Case Study Progress
Respiratory Disorders
Get Clinical Tree app for offline access



