Characterized by hypoxemia (PaO2 less than 50 mm Hg) and/or hypercapnia (PaCO2 greater than 50 mm Hg) and acidosis (pH less than 7.35).
Occurs rapidly, usually in minutes to hours or days.
Characterized by hypoxemia (decreased PaO2) and/or hypercapnia (increased PaCO2) with a normal pH (7.35 to 7.45).
Occurs over a period of days to months to years, allowing for activation of compensatory mechanisms, including bicarbonate retention with normalization of pH.
Characterized by an abrupt increase in the degree of hypoxemia and/or hypercapnia in patients with preexisting chronic respiratory failure.
May occur after an acute upper respiratory infection, pneumonia, or exacerbation or without obvious cause.
Extent of deterioration is best assessed by comparing the patient’s present arterial blood gas (ABG) levels with previous ABG levels (patient baseline).
Primary problem is inability to adequately oxygenate the blood, resulting in hypoxemia, due to an abnormality in one or more parts of the respiratory system, central nervous system, respiratory muscles, or chest wall.
Hypoxemia occurs because damage to the alveolar-capillary membrane causes leakage of fluid into the interstitial space or into the alveoli and slows or prevents movement of oxygen from the alveoli to the pulmonary capillary blood.
Typically, this damage is widespread, resulting in many areas of the lung being poorly ventilated or nonventilated.
Consequences are severe ventilation-perfusion imbalance and shunt.
Hypocapnia may result from hypoxemia and decreased pulmonary compliance. Fluid within the lungs makes the lung less compliant or stiffer.
Change in compliance reflexively stimulates the increased ventilation.
Ventilation is also increased as a response to hypoxemia.
Ultimately, if treatment is unsuccessful, PaCO2 will increase and the patient will experience both an increase in PaCO2 and a decrease in PaO2.
Etiology includes:
Cardiogenic pulmonary edema (left-sided heart failure; mitral stenosis).
Acute respiratory distress syndrome (ARDS). Underlying causes of ARDS include shock, sepsis, pneumonia; trauma, such as fat emboli, head injury, lung trauma; aspiration, near drowning; inhaled toxins, such as oxygen in high concentrations, smoke, corrosive chemicals; hematologic conditions, such as massive transfusions, postcardiopulmonary bypass; and metabolic disorders, such as pancreatitis, uremia.
Primary problem is insufficient respiratory center stimulation or insufficient chest wall movement, resulting in alveolar hypoventilation.
Hypercapnia occurs because impaired neuromuscular function or chest wall expansion limits the amount of carbon dioxide removed from the lungs.
Primary problem is not the lungs. The patient’s minute ventilation (tidal volume [VT] times the number of breaths per minute) is insufficient to allow normal alveolar gas exchange.
The carbon dioxide (CO2) not excreted by the lungs combines with water (H2O) to form carbonic acid (H2CO3). This predisposes to acidosis and a fall in pH.
Hypoxemia occurs as a consequence of inadequate ventilation and hypercapnia. When PaCO2 rises, PaO2 falls unless increased amounts of oxygen are added to the inspired air.
Etiology includes:
Insufficient respiratory center activity (drug intoxication, such as opioid overdose, general anesthesia; vascular disorders, such as cerebral vascular insufficiency, brain tumor; trauma, such as head injury, increased intracranial pressure).
Insufficient chest wall function (neuromuscular disease, such as Guillain-Barré syndrome, myasthenia gravis, amyotropic lateral sclerosis, poliomyelitis; trauma to the chest wall resulting in multiple fractures; spinal cord trauma; kyphoscoliosis).
Primary problem is acute exacerbation or chronic progression of previously existing lung disease, resulting in CO2 retention.
Hypercapnia occurs because damage to the lung parenchyma and/or airway obstruction limits the amount of CO2 removed by the lungs.
Primary problem is preexisting lung disease—usually chronic bronchitis, emphysema, or severe asthma. This limits CO2 removal from the lungs.
The CO2 not excreted by the lungs combines with H2O to form H2CO3. This predisposes to acidosis and a fall in pH.
Hypoxemia occurs as a consequence of hypoventilation and hypercapnia. In addition, damage to the lung parenchyma and/or airway obstruction limits the amount of oxygen that enters the pulmonary capillary blood.
Etiology includes:
Chronic obstructive pulmonary disease (COPD) (chronic bronchitis, emphysema).
Severe asthma.
Cystic fibrosis.
Hypoxemia—restlessness, agitation, dyspnea, disorientation, confusion, delirium, loss of consciousness.
Hypercapnia—headache, somnolence, dizziness, confusion.
Tachypnea initially; then, when no longer able to compensate, bradypnea.
Accessory muscle use.
Asynchronous respirations.
 NURSING ALERT
NURSING ALERT
ABG analysis—shows changes in PaO2, PaCO2, pH, and possibly HCO3 from patient’s normal; or PaO2 less than 50 mm Hg, PaCO2 greater than 50 mm Hg, pH less than 7.35.
Pulse oximetry—decreasing SpO2.
End tidal CO2 monitoring—elevated.
Complete blood count, serum electrolytes, chest x-ray, urinalysis, electrocardiogram (ECG), blood and sputum cultures— to determine underlying cause and patient’s condition.
Oxygen therapy to correct the hypoxemia.
Turn patient regularly and mobilize when clinically stable to improve ventilation and oxygenation.
Bronchodilators and possibly corticosteroids to reduce bronchospasm and inflammation.
Diuretics for pulmonary vascular congestion or pulmonary edema.
Mechanical ventilation as indicated. Noninvasive positivepressure ventilation using a face mask may be a successful option for short-term support of ventilation.
 NURSING ALERT
NURSING ALERT
Oxygen toxicity if prolonged high FiO2 required.
Barotrauma from mechanical ventilation intervention.
Note changes suggesting increased work of breathing (dyspnea, tachypnea, diaphoresis, intercostal muscle retraction, fatigue) or pulmonary edema (fine, coarse crackles or rales; frothy pink sputum).
Assess breath sounds.
Diminished or absent sounds suggest inability to ventilate the lungs sufficiently to prevent atelectasis.
Crackles may indicate ineffective airway clearance, fluid in the lungs.
Wheezing indicates narrowed airways and bronchospasm.
Rhonchi and crackles suggest ineffective secretion clearance.
Assess level of consciousness (LOC) and ability to tolerate increased work of breathing.
Confusion, lethargy, rapid shallow breathing, abdominal paradox (inward movement of abdominal wall during inspiration), and intercostal retractions suggest inability to maintain adequate minute ventilation.
Assess for signs of hypoxemia and hypercapnia.
Analyze ABG and compare with previous values.
If the patient cannot maintain a minute ventilation sufficient to prevent CO2 retention, pH will fall.
Mechanical ventilation or noninvasive ventilation may be needed if pH falls to 7.30 or below.
Determine vital capacity (VC) and respiratory rate and compare with values indicating need for mechanical ventilation:
VC < 15 mL/kg.
Respiratory rate > 30 breaths/minute.
Negative inspiratory force < -15 to -25 cm H2O.
Refractory hypoxia.
Determine hemodynamic status through assessment of blood pressure (BP), heart rate, pulmonary wedge pressure, cardiac output, and SvO2 and compare with previous values. If patient is on mechanical ventilation with positive end-expiratory pressure (PEEP), venous return may be limited, resulting in decreased cardiac output.
Monitor closely and document complete assessments. Evaluate closely for any changes in clinical assessments.
Perform thorough systematic assessment, including mental status, vital signs, respiratory status, and cardiovascular status.
Evaluate for signs of hypoxia when anxiety, restlessness, confusion, or aggression of new onset are noted. Do not administer sedatives unless hypoxia has been ruled out by performing respiratory assessment.
Notify appropriate health care provider of significant findings of hypoxia: SpO2 < 92%, cyanosis, circumoral pallor, rapid and shallow respirations, abnormal breath sounds, change in behavior or level of consciousness (LOC). Request assessment and intervention by health care provider, as indicated.
Use extreme caution in administering sedatives and opioids to patients at risk for respiratory compromise.
Impaired Gas Exchange related to inadequate respiratory center activity or chest wall movement, airway obstruction, and/or fluid in lungs.
Ineffective Airway Clearance related to increased or tenacious secretions.
Administer oxygen to maintain PaO2 of 60 mm Hg or SaO2 greater than 90% using devices that provide increased oxygen concentrations (aerosol mask, partial rebreathing mask, nonrebreathing mask, noninvasive positive pressure ventilation or mechanical ventilation).
Administer antibiotics, cardiac medications, and diuretics as ordered for underlying disorder.
Monitor fluid balance by intake and output measurement, daily weight, and direct measurement of pulmonary capillary wedge pressure to detect presence of hypovolemia or hypervolemia.
Provide measures to prevent atelectasis and promote chest expansion and secretion clearance, as ordered (incentive spirometer, nebulization, head of bed elevated 30 degrees, turn frequently, out of bed when clinically stable).
Monitor adequacy of alveolar ventilation by frequent measurement of SpO2, ABG levels, respiratory rate, and VC.
Compare monitored values with criteria indicating need for mechanical ventilation (see above in Nursing Assessment section). Report and prepare to assist with noninvasive ventilation or intubation and initiation of mechanical ventilation, if indicated.
Administer medications to increase alveolar ventilation— bronchodilators to reduce bronchospasm, corticosteroids to reduce airway inflammation.
Teach slow, pursed-lip breathing to reduce airflow obstruction and improve oxygen levels. Chest physiotherapy may be considered for retained secretions.
Suction patient, if needed, to assist with removal of secretions.
If the patient becomes increasingly lethargic, cannot cough or expectorate secretions, cannot cooperate with therapy, or if pH falls below 7.30, despite use of the above therapy, report and prepare to assist with intubation and initiation of mechanical ventilation.
Instruct patient with preexisting pulmonary disease to seek early intervention for infections to prevent acute respiratory failure, pneumonia, and exacerbations.
Teach patient about medication regimen.
Proper technique for inhaler use
Dosage and timing of medications
Monitoring for adverse effects of corticosteroids to report to health care provider: weight gain due to fluid retention, hyperglycemia, mood changes, insomnia, bruising, fragile skin; vision changes due to cataracts or glaucoma.
Encourage patients at risk, especially older adults and those with preexisting lung disease, to get pneumococcal pneumonia immunization.
Pneumococcal vaccine protects against Streptococcus pneumoniae bacteria, a major cause of morbidity and mortality.
If a person received their first pneumococcal vaccination before age 65, they should be revaccinated after age 65, if more than 5 years have elapsed since the previous dose.
Pneumococcal polysaccharide vaccine is recommended for anyone age 2 to 64 who has heart or lung disease, sickle cell disease, diabetes, alcoholism, cirrhosis, leaks of cerebrospinal fluid or cochlear implants, lymphoma or leukemia, kidney failure, multiple myeloma, impaired immune function, or asplenia; currently a smoker; or residents of nursing homes or long-term care facilities.
Encourage annual immunization for influenza in persons 6 months and older. If vaccine is in limited supply, the Centers for Disease Control and Prevention recommends immunization of persons age 6 months to 4 years and over 49 years, and all patients with the following characteristics:
Chronic pulmonary (including asthma), renal, hepatic, neurologic, hematologic, or metabolic disorders (including diabetes mellitus).
Are or will be pregnant during the influenza season.
Age 6 months to 18 years and receiving long-term aspirin therapy.
American Indians/Alaska Natives.
Morbidly obese (body mass index 40 or greater).
Immunocompromised.
Residents of nursing homes or chronic care facilities.
Cardiovascular disease (excluding hypertension).
Health care workers.
Household contacts of those at risk for influenza.
Inactivated influenza vaccine should be given to people age 6 months to 5 years and in those age 50 and older.
Intranasal live attenuated vaccine is an alternative for people ages 5 to 49 without chronic conditions, human immunodeficiency virus (HIV), or asthma.
 Evidence Base
Evidence Base Evidence Base
Evidence Base
ABG values within patient’s normal limits.
Decreased secretions; lungs clear.
 Evidence Base
Evidence Base
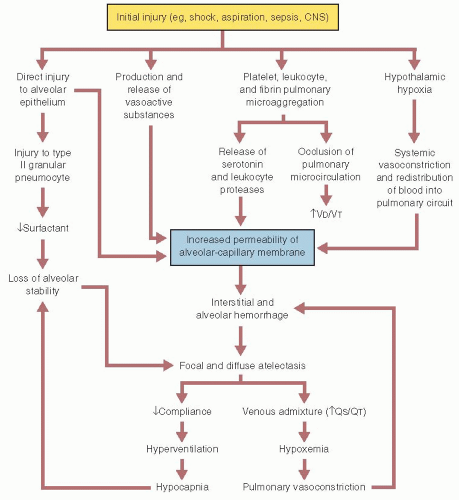
Pulmonary and/or nonpulmonary insult to the alveolarcapillary membrane causing protein-rich fluid leakage into interstitial and alveolar spaces, resulting in edema.
Inflammation in the interstitium and alveolar space promote atelectasis and lung damage.
This is associated with severe hypoxemia and reduced pulmonary compliance.
Fibroproliferative state often accompanied by capillary thrombosis, lung fibrosis, and neovascularization follows.
Diffuse alveolar damage with ventilation-perfusion (V/Q) mismatch caused by shunting of blood (see Figure 11-1).
Mechanisms are unclear. Acute lung injury includes both pulmonary capillary endothelium and alveolar epithelium. Etiologies are numerous and can be pulmonary or nonpulmonary. Predisposing factors include (but are not limited to):
Infections, including sepsis, pneumonia (usually bacterial or aspiration).
Shock (any cause), trauma, pulmonary contusion, near drowning, direct or indirect lung injury, burns, pancreatitis.
Inhaled agents—smoke, high concentration of oxygen, corrosive substances.
Major surgery including coronary artery bypass graft, fat emboli, lung or bone marrow transplantation, transfusion of blood products, reperfusion pulmonary edema.
Acute onset of severe dyspnea, tachypnea, tachycardia, use of accessory muscles, cyanosis.
Increasing requirements of oxygen therapy. Hypoxemia refractory to supplemental oxygen therapy.
Scattered crackles and rhonchi heard on auscultation.
Decreased pulmonary compliance, evidenced by increasing pressure required to ventilate patient on mechanical ventilator.
Diagnosis is based on clinical, hemodynamic, and oxygen criteria. The hallmark signs for ARDS include acute-onset, severe hypoxemia, despite increasing oxygen therapy, and chest x-ray exhibiting bilateral infiltrates.
Pulmonary artery catheter readings show pulmonary artery wedge pressure >18 mm Hg, absence of left atrial hypertension, and no clinical signs of heart failure.
Current ARDS treatment is primarily supportive. The underlying cause for ARDS should be determined so appropriate treatment can be initiated.
Mechanical ventilation is nearly always required to decrease work of breathing and improve oxygenation.
Low VT by mechanical ventilation (6 mL/kg of predicted body weight) reduces mortality compared to high-volume ventilation.
Protective ventilation (ie, maximum inspiratory pressure of <35 cm) should be instituted.
PEEP should be used to improve PaO2 (keeps the alveoli open, thereby improving gas exchange). Therefore, a lower oxygen concentration (FiO2) may be used to maintain satisfactory oxygenation.
Fluid management must be maintained. The patient may be hypovolemic due to the movement of fluid into the interstitium of the lung. Pulmonary artery catheter monitoring and inotropic medication can be helpful.
Medications are aimed at treating the underlying cause. Corticosteroids are used infrequently due to the controversy regarding benefits of usage.
Adequate nutrition should be initiated early and maintained.
 NURSING ALERT
NURSING ALERT
Infections, such as pneumonia, sepsis.
Respiratory complications, such as pulmonary emboli, barotrauma, oxygen toxicity, subcutaneous emphysema, or pulmonary fibrosis.
GI complications, such as stress ulcer, ileus.
Cardiac complications, such as decreased cardiac output and dysrhythmias.
Renal failure, disseminated intravascular coagulation.
Multiorgan failure and sepsis, which may result in death.
Cognitive impairment.
 Evidence Base
Evidence Base
Primarily viral etiology, but may also arise from bacterial agents. Exposure to irritants may also trigger bronchitis.
Airways become inflamed with decreased mucociliarly function. Airways may become clogged with mucus and irritated with increased mucus production.
Dry cough, which may become productive.
Productive cough, clear to purulent sputum.
Occasional pleuritic chest pain.
Diffuse rhonchi and crackles heard on auscultation.
Chest x-ray—no evidence of infiltrates or consolidation.
Sputum Gram stain and culture have limited value.
Spirometry to determine forced vital capacity (FVC), forced expiratory volume in 1 second (FEV1), and FEV1/FVC ratio, which may indicate underlying COPD.
Antibiotic therapy is normally avoided due to predominantly viral cause of infection. If bacterial infection is present or strongly suspected, or for patients with underlying COPD, antibiotics are usually prescribed based on community resistance patterns and patient history and physical examination.
Hydration and humidification.
Secretion clearance interventions for retained or excess mucus (may include controlled cough, positive expiratory pressure (PEP) valve therapy, chest physical therapy).
Bronchodilators for bronchospasm and related cough in patients with evidence of airflow obstruction.
Symptom management for cough and fever, if present.
Obtain history of respiratory infection, course, and length of symptoms.
Assess severity of cough and characteristics of sputum production.
Auscultate chest for diffuse rhonchi and crackles as opposed to localized crackles usually heard with pneumonia.
Ineffective Airway Clearance related to sputum production.
Supportive care with symptom management is usually first line in otherwise healthy patients. For those with bacterial infections or underlying COPD, administer or teach self-administration of antibiotics, as ordered.
Encourage mobilization of secretions through patient mobilization and, possibly, hydration, chest physical therapy, and coughing. Educate patient that beverages with caffeine or alcohol do not promote hydration.
If ordered, administer or teach self-administration of inhaled bronchodilators to reduce bronchospasm and enhance secretion clearance.
Caution patients on the use of over-the-counter cough suppressants, antihistamines, and decongestants that may cause drying and retention of secretions. Cough preparations containing the mucolytic guaifenesin may be appropriate.
Instruct patient about medication regimen, including the completion of the full course of antibiotics, if prescribed, and the effects of food on the absorption of the medications. If patient is not being treated with antibiotics, reassure patient that the majority of cases of people recover from bronchitis without antibiotic treatment, but to advise health care provider if symptoms do not improve.
Encourage patient to seek medical attention for shortness of breath and worsening condition.
Advise patient that a dry cough may persist after bronchitis due to irritation of the airways. A bedside humidifier and avoidance of dry environments may help.
Encourage patient to discuss complementary and alternative therapies with health care provider. When questioned, some people use garlic as an antimicrobial. Other herbs that many believe to be helpful for asthma and bronchitis are Echinacea, eucalyptus, and thyme; however, there are no definitive studies that show benefit. Since many herbal products are mixed with other ingredients and are not standardized, safety cannot be ensured.
Coughs up clear secretions effectively.
 Evidence Base
Evidence Base
The development of community-acquired pneumonia (CAP) is normally due to a defect in host defenses, exposure to a virulent microorganism, or an overwhelming exposure. An organism gains access to the lungs through aspiration of oropharyngeal contents, by inhalation of respiratory secretions from infected individuals, by way of the bloodstream, or from direct spread to the lungs as a result of surgery or trauma.
Risk factors for pneumonia include altered mental status, smoking, alcohol use, hypoxemia, acidosis, toxic inhalations, pulmonary edema, uremia, malnutrition, bronchial obstruction, advanced age immunosuppression, heart or lung disease (cystic fibrosis, bronchiectasis, COPD, ciliary dysfunction, lung cancer), viral respiratory infection, and history of pneumonia. Patients with bacterial pneumonia may have an underlying disease that impairs host defense; pneumonia arises from endogenous flora of the person whose resistance has been altered or from aspiration of oropharyngeal secretions.
Immunocompromised patients include those receiving corticosteroids or immunosuppressants, those with cancer, those being treated with chemotherapy or radiotherapy, those undergoing organ transplantation, alcoholics, intravenous (IV) drug abusers, and those with HIV disease and acquired immunodeficiency syndrome (AIDS).
These people have an increased risk of developing overwhelming infection. Infectious agents include aerobic and anaerobic gram-negative bacilli; Staphylococcus; Nocardia; fungi; Candida; viruses such as cytomegalovirus; Pneumocystis jiroveci (previously known as P. carinii); reactivation of tuberculosis (TB); and others.
When bacterial pneumonia occurs in a healthy person, there is usually a history of preceding viral illness.
Other predisposing factors include conditions interfering with normal drainage of the lung, such as tumor, general anesthesia, and postoperative immobility; depression of the central nervous system (CNS) from drugs, neurologic disorders, or other conditions, such as alcoholism; and intubation or respiratory instrumentation.
Pneumonia may be divided into three groups:
Community acquired, due to a number of organisms.
“Typical” organisms include Streptococcus pneumoniae (most common organism), Haemophilus influenzae, Staphylococcus aureus, Group A streptococci, Moraxella catarrhalis, anaerobes, and aerobic gram-negative bacteria.
Atypical pneumonia may be caused by Legionella species, Mycobacterium pneumoniae, and Chlamydophila pneumoniae.
Hospital or nursing home acquired (nosocomial), due primarily to gram-negative bacilli and staphylococci.
Pneumonia in the immunocompromised person.
People older than age 65 have a high rate of mortality, even with appropriate antimicrobial therapy.
 NURSING ALERT
NURSING ALERT
Defined by clinical signs and symptoms (fever, tachypnea, rales, cough, sputum production, pleuritic chest pain, with chest x-ray confirmation). Local epidemiology and patient travel history, history of exposures, local or national outbreaks may help in pneumonia identification.
Pleuritic chest pain may be aggravated by respiration/coughing.
Dyspnea and tachypnea may be accompanied by respiratory grunting, nasal flaring, use of accessory muscles of respiration, fatigue.
Tachycardia may be present.
Table 11-1 Commonly Encountered Pneumonias | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Chest x-ray shows a discernable infiltrate and presence/extent of pulmonary disease, typically consolidation.
Patients with CAP should be investigated for specific pathogens that would significantly alter standard management decisions, when such pathogen is suspected on the basis of clinical and epidemiologic clues. Gram stain and culture and sensitivity tests of sputum may be indicated to determine offending organism in select cases. Endobronchial specimens should be obtained from intubated patients. Indications for sputum culture in persons with a productive cough include:
Admission to intensive care unit.
Antibiotic failure.
Cavitary lesion on chest x-ray.
Active alcohol abuse.
Severe lung disease.
Positive Legionella or pneumococcal urinary antigen test.
Pleural effusion.
The value of sputum Gram stain and culture in nosocomial pneumonia, especially ventilator-associated pneumonia, is more universally acknowledged. Sputum Gram stain and culture are indicated for all patients with hospital-acquired pneumonia.
Pretreatment blood samples for culture to detect bacteremia should be obtained from patients with admission to intensive care unit, cavitary lesion on chest x-ray, leukopenia, active alcohol abuse, chronic severe liver disease, asplenia, positive pneumococcal urinary antigen test, or pleural effusion.
Immunologic tests may be ordered to detect microbial antigens in serum, sputum, and urine.
Severity-of-illness scores, such as the CURB-65 criteria (confusion, uremia, respiratory rate, low blood pressure, age 65 or greater), or pneumonia severity index can be used to identify patients with CAP who may be candidates for outpatient treatment.
 Evidence Base
Evidence Base
Antimicrobial therapy—depends on empiric recommendations and/or laboratory identification of causative organism and sensitivity to specific antimicrobials.
Oxygen therapy, if patient has inadequate gas exchange.
Patients with hypoxemia or respiratory distress who are refractory to oxygen should receive a cautious trial of noninvasive ventilation unless they require immediate intubation due to severe hypoxemia or acute respiratory failure.
Low VT ventilation (6 mL/kg ideal body weight) for diffuse bilateral pneumonia or ARDS.
Early mobilization when clinically stable reduces length of facility stay.
Assess influenza and pneumococcal vaccination status and if not currently vaccinated, perform either at hospital discharge or during outpatient treatment.
Advise and assist with smoking cessation in currently smoking patients.
Respiratory hygiene measures, including the use of hand hygiene and masks or tissues for patients with cough, should be used in outpatient settings and EDs to reduce the spread of respiratory infections.
Pleural effusion.
Sustained hypotension and shock, especially in gram-negative bacterial disease, particularly in older patients.
Superinfection: pericarditis, bacteremia, and meningitis.
Delirium—considered a medical emergency.
Atelectasis—due to mucus plugs.
Delayed resolution.
Take a careful history to help establish etiologic diagnosis.
History of recent respiratory illness including mode of onset, complete medical history including chronic lung or liver disease, asplenia, immunologic status including HIV infection, exposure to animals, and recent travel.
Presence of purulent sputum, increased amount of sputum, fever, chills, chest pain, dyspnea, tachypnea.
Any family illness.
Medications (including recent antibiotics), alcohol, tobacco, or IV drug use.
Observe for anxious, flushed appearance, shallow respirations, splinting of affected side, confusion, disorientation.
Auscultate for crackles overlying affected region and for bronchial breath sounds when consolidation (filling of airspaces with exudate) is present.
Impaired Gas Exchange related to decreased ventilation secondary to inflammation and infection involving distal airspaces.
Ineffective Airway Clearance related to excessive tracheobronchial secretions.
Acute Pain related to inflammatory process and dyspnea.
Risk for Injury secondary to complications.
Observe for cyanosis, dyspnea, hypoxia, and confusion, indicating worsening condition.
Follow ABG levels/SaO2 to determine oxygen need and response to oxygen therapy.
Administer oxygen at concentration to maintain Pao2 at acceptable level. Hypoxemia may be encountered because of abnormal V/Q mismatch with shunt in affected lung segments.
Use caution with high concentrations of oxygen in patients with COPD, particularly with evidence of CO2 retention; use of high oxygen concentrations may worsen alveolar ventilation in some patients by depressing the patient’s only remaining ventilatory drive. If high concentrations of oxygen are given, monitor alertness and PaO2 and PaCO2 levels for signs of CO2 retention.
Place patient in an upright position as tolerated to obtain greater lung expansion and improve aeration. Frequent turning and increased activity (up in chair, ambulate as tolerated) should be employed.
If ordered, obtain freshly expectorated sputum for Gram stain and culture, preferably early morning specimen, as directed. Instruct the patient as follows:
Perform oral care and rinse mouth with water to minimize contamination by normal flora.
Breathe deeply several times.
Cough deeply and expectorate raised sputum into sterile container.
Encourage patient to cough; retained secretions interfere with gas exchange. Suction as necessary.
Encourage increased fluid intake, unless contraindicated, to thin mucus and promote expectoration and replace fluid losses caused by fever, diaphoresis, dehydration, and dyspnea.
Humidify air or oxygen therapy, which may loosen secretions and improve ventilation.
Employ chest wall percussion and postural drainage, when appropriate, to loosen and mobilize secretions.
Auscultate the chest for crackles and rhonchi.
Cough suppressants may be appropriate in some cases when coughing is nonproductive.
Mobilize patient to improve ventilation and secretion clearance and reduce risk of atelectasis and worsening pneumonia.
Place patient in a comfortable position (semi-Fowler’s) for resting and breathing; encourage frequent change of position to prevent pooling of secretions in lungs and atelectasis.
Demonstrate how to splint the chest while coughing.
Avoid suppressing a productive cough.
Administer prescribed analgesic agent to relieve pain. Use opioids cautiously in patients with a history of COPD.
Use comfort measures to improve symptom control.
Encourage modified bed rest during febrile period.
Watch for abdominal distention or ileus, which may be due to swallowing of air during intervals of severe dyspnea. Insert a nasogastric (NG) or rectal tube, as directed.
 GERONTOLOGIC ALERT
GERONTOLOGIC ALERT
Remember that fatal complications may develop during the early period of antimicrobial treatment.
Monitor temperature, pulse, respiration, BP, oximetry, mentation, and for evidence of dyspnea at regular intervals to assess the patient’s response to therapy.
Auscultate lungs and heart. Heart murmurs or friction rub may indicate acute bacterial endocarditis, pericarditis, or myocarditis.
Employ special nursing surveillance for patients with:
Alcoholism, COPD, immunosuppression—these people as well as older patients may have little or no fever.
Chronic bronchitis—it may be difficult to detect subtle changes in condition because the patient may have seriously compromised pulmonary function and regular mucus production.
Epilepsy—pneumonia may result from aspiration after a seizure.
Delirium—may be caused by hypoxia, meningitis, delirium tremens of alcoholism.
Assess these patients for unusual behavior, alterations in mental status, stupor, and heart failure.
Assess for resistant fever or return of fever, potentially suggesting bacterial resistance to antibiotics.
 NURSING ALERT
NURSING ALERT
Advise patient to complete entire course of antibiotics.
Advise patient that fatigue and weakness may be prolonged after pneumonia.
Once clinically stable, encourage gradual increase in activities to improve ventilation and reduce hazards of immobility.
Encourage breathing exercises to clear lungs and promote full expansion and function.
Explain that a chest x-ray is usually taken 4 to 6 weeks after recovery to evaluate lungs for clearing and detect any tumor or underlying cause.
Advise smoking cessation. Cigarette smoke destroys tracheobronchial cilial action, which is the first line of defense of lungs; also irritates mucosa of bronchi and inhibits function of alveolar scavenger cells (macrophages).
Advise the patient to keep up natural resistance with good nutrition, adequate rest, and physical activity, when tolerated. One episode of pneumonia may make the patient susceptible to recurring respiratory infections.
Instruct patient to avoid fatigue, sudden extremes in temperature, and excessive alcohol intake, which lower resistance to pneumonia.
Assess for and encourage vaccination with pneumococcal polysaccharide vaccine (see page 280).
Encourage annual influenza vaccination (see page 280). Influenza vaccine is associated with reduced hospitalizations for pneumonia, influenza, and death in community-dwelling older adults.
Advise avoidance of contact with people who have upper respiratory infections for several months after pneumonia resolves.
Respiratory and hand hygiene includes frequent handwashing, especially after contact with others.
Cyanosis and dyspnea reduced; ABG levels and SaO2 improved.
Coughs effectively; absence of crackles.
Appears more comfortable; free of pain.
Fever controlled, no signs of resistant infection.
Patients at risk and factors associated with risk:
Loss of protective airway reflexes (swallowing, cough) caused by altered state of consciousness, alcohol or drug overdose, during resuscitation procedures, seriously ill or debilitated patients, abnormalities of gag and swallowing reflexes.
NG tube feedings.
Obstetric patients—from general anesthesia, lithotomy position, delayed emptying of stomach from enlarged uterus, labor contractions.
GI conditions—hiatal hernia, intestinal obstruction, abdominal distention.
Prolonged endotracheal (ET) intubation/tracheostomy— can depress glottic and laryngeal reflexes from disuse.
Effects of aspiration depend on volume and character of aspirated material.
Particulate matter—mechanical blockage of airways and secondary infection.
Anaerobic bacterial aspiration—from oropharyngeal secretions.
Gastric juice—destructive to alveoli and capillaries; results in outpouring of protein-rich fluids into the interstitial and intra-alveolar spaces. (Impairs exchange of oxygen and CO2, producing hypoxemia, respiratory insufficiency, and respiratory failure.)
Tachycardia, fever.
Dyspnea, cough, tachypnea.
Cyanosis.
Crackles, rhonchi, wheezing.
Pink, frothy sputum (may simulate acute pulmonary edema).
Chest x-ray may be normal initially; with time, shows consolidation and other abnormalities.
Clearing the obstructed airway.
If foreign body is visible, it may be removed manually.
Place the patient in tilted head-down position on right side (right side more commonly affected if patient has aspirated solid particles).
Suction trachea/ET tube—to remove particulate matter.
Laryngoscopy/bronchoscopy may be performed for aspiration of solid material.
Fluid volume replacement for correction of hypotension.
Antimicrobial therapy if there is evidence of superimposed bacterial infection.
Correction of acidosis; respiratory acidosis and metabolic acidosis indicate a severe reaction due to aspiration of gastric contents.
Oxygen therapy and assisted ventilation if adequate ABG values cannot be maintained.
Lung abscess; empyema.
Necrotizing pneumonia.
ARDS.
Assess for airway obstruction.
Assess for risk factors for aspiration.
Assess for development of fever, foul-smelling sputum, and development of congestion.
Impaired Gas Exchange related to decreased ventilation secondary to inflammation and infection involving distal airspaces.
Ineffective Airway Clearance related to excessive tracheobronchial secretions.
Acute Pain related to inflammatory process and dyspnea.
Risk for Injury secondary to complications.
Be on guard constantly and monitor patients at risk as described earlier.
Elevate head of bed for debilitated patients, for those receiving tube feedings, and for those with neurologic or motor diseases of the esophagus.
Place patients with impaired cough and/or gag reflexes in an upright position.
Make sure NG tube is patent.
Give tube feedings slowly, with patient sitting up in bed. Check for tube feeding residuals.
Check position of tube in stomach before feeding.
Check seal of cuff of tracheostomy or ET tube before feeding.
Keep the patient in a fasting state before anesthesia (at least 8 hours).
Feed patients with impaired swallowing slowly, and make sure that no food is retained in mouth after feeding.
 NURSING ALERT
NURSING ALERT Evidence Base
Evidence Base
Obstruction, either partial or full, of pulmonary arteries, which causes decrease or absent blood flow; therefore, there is ventilation but no perfusion (V/Q mismatch).
Hemodynamic consequences:
Increased pulmonary vascular resistance.
Increased pulmonary artery pressure (PAP).
Increased right-sided heart workload to maintain pulmonary blood flow.
Right-sided heart failure.
Decreased cardiac output.
Decreased BP.
Shock.
Pulmonary emboli can vary in size and seriousness of consequences.
Predisposing factors include:
Stasis, prolonged immobilization.
Concurrent phlebitis.
Heart failure, stroke.
Injury to vessel wall.
Coagulation disorders, hypercoagulable state.
Malignancy.
Advancing age, estrogen therapy, oral contraceptives
Fracture of long boxes.
Obesity.
 NURSING ALERT
NURSING ALERT
Rapid onset of dyspnea at rest, pleuritic chest pain, cough, syncope, delirium, apprehension, tachypnea, diaphoresis, hemoptysis.
Chest pain with apprehension and a sense of impending doom occurs when most of the pulmonary artery is obstructed.
Tachycardia, rales, fever, hypotension, cyanosis, heart gallop, loud pulmonic component of S2 (split S2).
Calf or thigh pain, edema, erythema, tenderness or palpable cord (signs suggestive of deep vein thrombosis).
 NURSING ALERT
NURSING ALERT
Thoracic imaging: V/Q scan (possibly using single-photon emission computed tomography) or helical contrast-enhanced computed tomography (CT).
Pulmonary angiography if noninvasive testing is inconclusive or not candidate for noninvasive testing. Contrast studies should be avoided in persons who are pregnant or have advanced renal failure.
D-Dimer assay for low to intermediate probability of pulmonary embolism.
ABG levels—decreased PaO2 is usually found, due to perfusion abnormality of the lung.
Chest x-ray—normal or possible wedge-shaped infiltrate.
 NURSING ALERT
NURSING ALERT
Oxygen is administered to relieve hypoxemia, respiratory distress, and cyanosis and to dilate pulmonary vasculature.
An infusion is started to open an IV route for drugs and fluids.
Vasopressors, inotropic agents such as dopamine, and antidysrhythmic agents may be indicated to support circulation if the patient is unstable.
ECG is monitored continuously for findings suggestive of right-sided heart failure, which may have a rapid onset. Changes may include sinus tachycardia, Q waves, late T-wave inversion, S wave in lead I, right bundle-branch block, right axis deviation, atrial fibrillation, and T-wave changes.
Small doses of IV morphine may be given to relieve anxiety, alleviate chest discomfort (which improves ventilation), and ease adaptation to mechanical ventilator, if this is necessary.
Pulmonary angiography, thoracic imaging, hemodynamic measurements, ABG analysis, and other studies are carried out.
IV heparin—stops further thrombus formation and extends the clotting time of the blood; it is an anticoagulant and antithrombotic.
IV loading dose usually followed by continuous pump or drip infusion or given intermittently every 4 to 6 hours.
Dosage adjusted to maintain the partial thromboplastin time (PTT) at 1½ to 2 times the pretreatment value (if the value was normal).
Protamine sulfate may be given to neutralize heparin in event of severe bleeding.
Oral anticoagulation with warfarin is usually used for follow-up anticoagulant therapy after heparin therapy has been established; interrupts the coagulation mechanism by interfering with the vitamin K-dependent synthesis of prothrombin and factors VII, IX, and X.
Dosage is controlled by monitoring serial tests of prothrombin time (PT); desired PT is 2 to 3 times control value.
Reported as international normalized ratio (INR) of 2.0 to 3.0 by most laboratories.
Anticoagulation is used to prevent new clot formation but does not dissolve previously formed clots. Thrombolytics are used to dissolve clots.
Thrombolytic agents, such as streptokinase, may be used in patients with massive pulmonary embolism.
Effective in lysing recently formed thrombi.
Improved circulatory and hemodynamic status.
Administered IV in a loading dose followed by constant infusion.
Newer clot-specific thrombolytics (tissue plasminogen activator, streptokinase activator complex, single-chain urokinase) are preferred.
Activate plasminogen only within thrombus itself rather than systematically.
Minimize occurrence of generalized fibrinolysis and subsequent bleeding.
 GERONTOLOGIC ALERT
GERONTOLOGIC ALERT
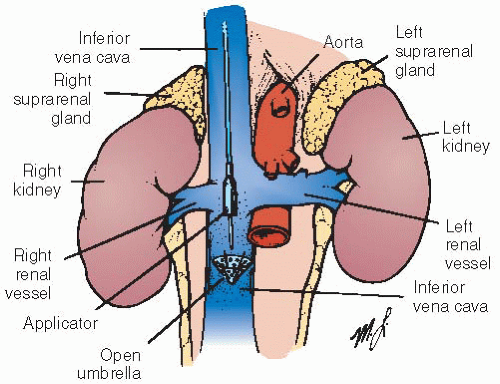
Interruption of vena cava—reduces channel size to prevent lower extremity emboli from reaching lungs. Accomplished by:
Ligation, plication, or clipping of the inferior vena cava.
Placement of transvenously inserted intraluminal filter in inferior vena cava to prevent migration of emboli (see Figure 11-2); inserted through femoral or jugular vein by way of catheter.
Embolectomy (removal of pulmonary embolic obstruction).
Bleeding as a result of treatment.
Respiratory failure.
Pulmonary hypertension, cor pulmonale.
Take nursing history with emphasis on onset and severity of dyspnea and nature of chest pain.
Examine the patient’s legs carefully. Assess for swelling of leg, duskiness, warmth, pain on pressure over gastrocnemius muscle, pain on dorsiflexion of the foot (positive Homans’ sign), which indicate thrombophlebitis as source.
Monitor respiratory rate—may be accelerated out of proportion to degree of fever and tachycardia.
Observe rate of inspiration to expiration.
Percuss for resonance or dullness.
Auscultate for friction rub, crackles, rhonchi, and wheezing.
Auscultate heart; listen for splitting of second heart sound.
Evaluate results of PT/PTT tests and INR for patients on anticoagulants and report results that are outside of therapeutic range promptly; anticipate a dosage change.
Ineffective Breathing Pattern related to acute increase in alveolar dead airspace and possible changes in lung mechanics from embolism.
Ineffective Tissue Perfusion (Pulmonary) related to decreased blood circulation.
Acute Pain (pleuritic) related to congestion, possible pleural effusion, possible lung infarction.
Anxiety related to dyspnea, pain, and seriousness of condition.
Risk for Injury related to altered hemodynamic factors and anticoagulant therapy.
Assess for hypoxia, dyspnea, headache, restlessness, apprehension, pallor, cyanosis, behavioral changes.
Monitor vital signs, ECG, oximetry, and ABG levels for adequacy of oxygenation.
Monitor patient’s response to IV fluids/vasopressors.
Monitor oxygen therapy—used to relieve hypoxemia.
Prepare patient for assisted ventilation when hypoxemia does not respond to supplemental oxygen. Hypoxemia is due to abnormalities of V/Q mismatch.
Closely monitor for shock—decreasing BP, tachycardia, cool, clammy skin.
Monitor prescribed medications given to preserve right-sided heart filling pressure and increase BP.
Maintain patient on bed rest during acute phase to reduce oxygen demands and risk of bleeding.
Monitor urinary output hourly because there may be reduced renal perfusion and decreased glomerular filtration.
Antiembolism compression stockings should provide a compression of 30 to 40 mm Hg.
Watch patient for signs of discomfort and pain.
Ascertain if pain worsens with deep breathing and coughing; auscultate for friction rub.
Give morphine, as prescribed, and monitor for pain relief and signs of respiratory depression.
Position with head of bed slightly elevated (unless contraindicated by shock) and with chest splinted for deep breathing and coughing.
Evaluate patient thoroughly for signs of hypoxia when anxiety, restlessness, and agitation of new onset are noted, before administering as-needed sedatives. Consider calling health care provider when these signs are present, especially if accompanied by cyanotic nail beds, circumoral pallor or cyanosis, and increased respiratory rate.
Correct dyspnea and relieve physical discomfort.
Explain diagnostic procedures and the patient’s role; correct misconceptions.
Listen to the patient’s concerns; attentive listening relieves anxiety and reduces emotional distress.
Speak calmly and slowly.
Do everything possible to enhance the patient’s sense of control.
Be alert for shock from low cardiac output secondary to resistance to right-sided heart outflow or to myocardial dysfunction due to ischemia.
Assess for skin color changes, particularly nail beds, lips, earlobes, and mucous membranes.
Monitor BP, pulse, and SpO2.
Measure urine output.
Monitor IV infusion of vasopressor or other prescribed agents.
Bleeding—related to anticoagulant or thrombolytic therapy.
Assess patient for bleeding; major bleeding may occur from GI tract, brain, lungs, nose, and genitourinary (GU) tract.
Perform stool guaiac test to detect occult blood loss.
Monitor platelet count to detect heparin-induced thrombocytopenia.
Minimize risk of bleeding by performing essential ABG analysis on upper extremities; apply digital compression at puncture site for 30 minutes; apply pressure dressing to previously involved sites; check site for oozing.
Maintain patient on strict bed rest during thrombolytic therapy; avoid unnecessary handling.
Discontinue infusion in the event of uncontrolled bleeding.
Notify health care provider on call immediately for change in LOC or sensation or ability to follow commands, move limbs, or respond to questions with clear articulation. Intracranial bleed may necessitate discontinuation of anticoagulation promptly to avert massive neurologic catastrophe.
Advise patient of the possible need to continue taking anticoagulant therapy for 6 weeks up to an indefinite period as well as safety considerations and drug and food interactions with anticoagulants.
Teach about signs of bleeding, especially of gums and nose, bruising, and blood in urine and stools.
For patients on anticoagulants, instruct to use soft toothbrush, avoid shaving with blade razor (use electric razor instead), and avoid aspirin-containing products. Notify health care provider of bleeding or increased bruising.
Warn against taking medications unless approved by health care provider because many drugs interact with anticoagulants.
Instruct patient to tell dentist about taking an anticoagulant.
Warn against inactivity for prolonged periods or sitting with legs crossed to prevent recurrence.
Warn against sports/activities that may cause trauma or injury to legs and predispose to a thrombus.
Encourage wearing a MedicAlert bracelet, identifying patient as anticoagulant user.
Instruct patient to lose weight, if applicable; obesity is a risk factor.
Discuss contraceptive methods with patient, if applicable; females with history of pulmonary embolus are advised against taking hormonal contraceptives.
Verbalizes less shortness of breath.
Vital signs stable; adequate urinary output.
Reports freedom from pain.
Appears more relaxed; sleeping at long intervals.
Progresses without complications.
usually infects the lung but can occur at virtually any site in the body.
 Evidence Base
Evidence Base
The term Mycobacterium is descriptive of the organism, which is a bacterium that resembles a fungus. The organisms multiply at varying rates and are characterized as acid-fast aerobic organisms that can be killed by heat, sunshine, and ultraviolet light.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



 GERONTOLOGIC ALERT Confusion may be only presenting feature in older patient
GERONTOLOGIC ALERT Confusion may be only presenting feature in older patient