Respiratory Alkalosis
QUICK LOOK AT THE CHAPTER AHEAD
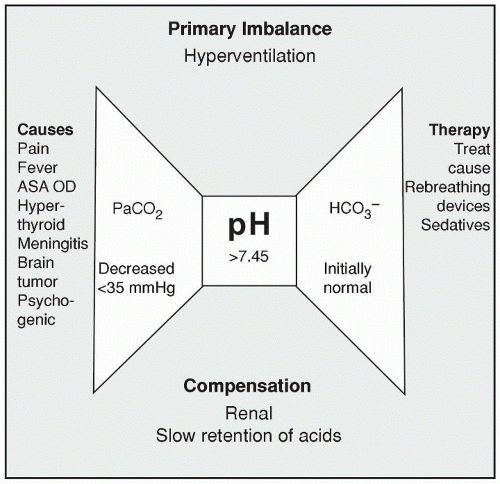
Respiratory alkalosis is associated with a carbonic acid deficit leading to a pH level greater than 7.45 and a CO2 blood content of less than 7.35 mm Hg. Respiratory alkalosis secondary to hyperventilation may be intentional, as with mechanical ventilation, or accidental, as with a panic attack. In this chapter we examine the causes, manifestations, and treatment of respiratory alkalosis.
Respiratory alkalosis is the result of alveolar hyperventilation and a loss of carbon dioxide (hypocapnia) faster than the body can replace it. It is associated with a carbonic acid deficit that leads to a pH > 7.45 and a CO2 blood content of less than 7.35 mm Hg. Respiratory alkalosis occurs secondary to hyperventilation when too much carbonic acid is expelled during expiration. The respirations are rapid and deep in hyperventilation. Panic attacks that result from high anxiety are a common cause of respiratory alkalosis. A less common cause is gram-negative septicemia, which triggers the respiratory center in the brainstem to increase respirations to the point of hyperventilation. Other causes are fever or oxygen deprivation, such as that triggered in high altitudes. The early stages of salicylate toxicity also stimulate the medullary respiratory center of the brainstem to hyperventilate.
An intentional cause for hyperventilation is through anesthesia or mechanical ventilation.
An intentional cause for hyperventilation is through anesthesia or mechanical ventilation.
Get Clinical Tree app for offline access