Chapter 40 REPRODUCTIVE HEALTH
Judy and her partner had been trying to have a baby for 10 years. They underwent 10 cycles of IVF. During that time Judy had three ectopic pregnancies and two miscarriages. She had two operations (microsurgery) to her fallopian tubes. On the 10th cycle, Judy and her husband decided that this was the final attempt. Judy was 39 years old and she knew that this was her only chance of having a child. Only one ovum was harvested but the IVF procedure was a success. The pregnancy had been achieved but at a great emotional cost to the couple.
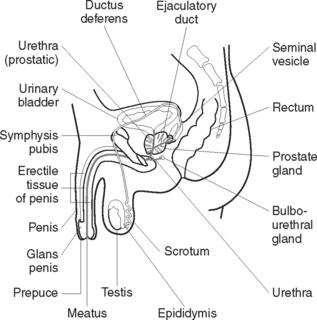
THE MALE REPRODUCTIVE SYSTEM
The male reproductive system (Figure 40.1) consists of essential and accessory organs. The essential organs, or gonads, are the testes. Accessory organs consist of a series of ducts or passageways, supportive sex glands and external structures.
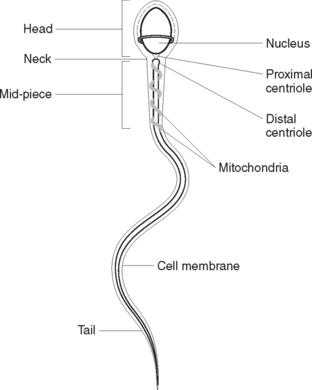
SPERMATOGENESIS
Sperm cells, or spermatozoa (Figure 40.2), are produced continuously throughout life from puberty onwards under the influence of the hormones testosterone and follicle-stimulating hormone (FSH). The anterior pituitary gland secretes FSH. Sperm cells originate from primordial cells that appear in the embryo early in gestation but are not functional until puberty. Before puberty the testes produce stem cells called spermatogonia. These cells multiply by mitotic division. At puberty, under the influence of FSH, spermatogonia undergo both mitotic and meiotic cell division, which results in sperm production. A mature sperm consists of a head, mid-piece and tail. The head contains the nucleus, with its genetic material (DNA). The mid-piece contains mitochondria to provide energy for the rapid tail movements. The tail propels the sperm with a lashing movement through the female reproductive tract.
DISORDERS OF THE MALE REPRODUCTIVE SYSTEM
HYDROCELE
Hydrocele is a painless collection of fluid within the tunica vaginalis of the testis from defective or inadequate reabsorption of fluid normally produced within the testis. It causes swelling of the scrotum and may be associated with infections, trauma or tumours. The individual may experience a feeling of heaviness or pain associated with increased scrotal size and may feel embarrassed because of the appearance of the scrotum.
DISORDERS OF THE PROSTATE GLAND
Benign prostatic hyperplasia
Researchers are working to develop BPH treatments that are more effective, less traumatic and have fewer side effects. These include using laser surgery, powerful electric currents and microwaves. Balloon urethroplasty and insertion of a stent into the urethra are other possible options.
PROSTATE SURGERY— PROSTATECTOMY
DISORDERS OF MULTIPLE CAUSE
Erectile dysfunction
Erectile dysfunction is defined as the inability to achieve and maintain an erection sufficient to permit satisfactory sexual intercourse. It may result from psychological, neurological, hormonal, arterial or cavernosal impairment or from a combination of these factors. The condition can be classified as psychogenic, organic, or mixed psychogenic and organic. Psychogenic factors may include performance anxiety, lack of arousability, relationship difficulties or mental health disorders such as depression and schizophrenia.
Organic causes of erectile dysfunction
Hormonal
A deficiency of androgens or an increase in prolactin secretion can both cause sexual dysfunction.
ASSESSMENT AND DIAGNOSTIC TESTS
EXAMINATION OF EXTERNAL GENITALIA
Testicular examination
Testicular self-examination (TSE [see Clinical Interest Box 40.1]) performed on a regular basis is the inspection and palpation of the testes to detect any changes. The testes are examined for size, shape, symmetry and texture. The earlier a change is discovered, the sooner it can be investigated and treated. It is important that the correct technique is taught to men in the target age group (15–40 years). Given that testicular cancer is most widespread in an age group in which men are generally healthy, there may be limited openings to teach TSE. Health promotion and screening in primary care, such as well-man clinics, affords an opportunity for education. Nurses working in the areas of adolescent, student and sexual health are seen as strategic professionals in educating men about TSE. Occupational health nurses involved in work-based screening may also have valuable opportunities to discuss health issues with men.
CLINICAL INTEREST BOX 40.1 Client teaching — testicular self-examination
INTERNAL AND SPECIMEN TESTING
Urethral culture
A small swab is inserted 3–5 cm into the urethra to obtain a specimen for microbiological analysis.
Semen analysis
A sample of semen is obtained and the sperm examined for motility, morphology, quantity and quality.
NURSING INTERVENTIONS IN MALE REPRODUCTIVE HEALTH
Men have specific health needs, experiences and concerns related to their gender as well as their biological sex. This is a relatively new concept in medical and nursing literature. Psychosocial factors related to male health are poorly understood and frequently ignored by many health practitioners. Men engage in less healthy lifestyles and adopt fewer health-promotion strategies than women, for reasons that are complex. An awareness of men’s health issues and poor health practices has led to the establishment of an international men’s health movement — the International Society for Men’s Health (www.ismh.org/). The aim of the movement is to increase awareness about current men’s health issues and promote men’s health initiatives.
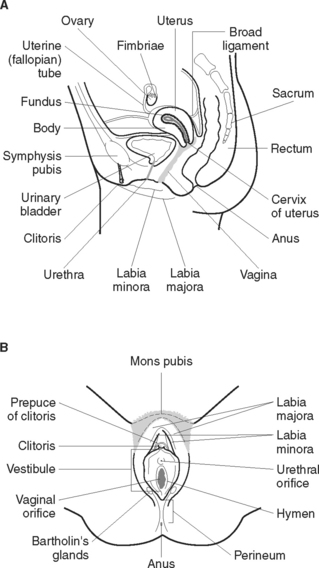
THE FEMALE REPRODUCTIVE SYSTEM
The female reproductive system functions to secrete hormones, produce ova, receive sperm and allow for fertilisation, implantation, development and birth of the baby. The female reproductive system (Figure 40.3) consists of essential and accessory organs. The essential organs, or gonads, are the ovaries. Accessory organs consist of a series of ducts, additional sex glands and external structures.
OOGENESIS
Oestrogen also stimulates the lining of the uterus to prepare for a fertilised ovum.
The effects of progesterone are to:
ACCESSORY ORGANS
The uterus is a hollow pear-shaped organ located in the pelvic cavity posterior to the urinary bladder and anterior to the rectum. It is suspended in the pelvis by a peritoneal fold (the broad ligament). Normally the uterus is in an anteverted position so that the upper portion rests on the bladder. The uterus consists of an upper rounded body and a lower narrow neck, the cervix. Above the point where the fallopian tubes enter is the fundus of the uterus. The walls of the uterus consist of an outer covering of peritoneum (perimetrium), a middle layer of thick involuntary muscle (myometrium) and an inner lining of mucous membrane (endometrium). The cervix is lined with mucus-secreting glands that provide lubrication. The functions of the uterus are to:
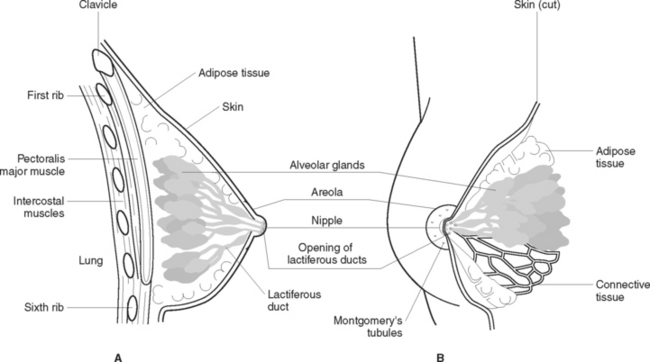
ACCESSORY GLANDS
Mammary glands (Figure 40.4) are accessory glands of the reproductive system. Their reproductive function is lactation. They are situated over the pectoral muscles and are attached to them by Cooper’s ligaments. The breast is a complex structure composed of a glandular and ductal network, fat, connective tissue, fascia, blood vessels, nerves and lymphatic vessels. In the centre of the breast a pigmented area, the areola, surrounds the nipple. Each breast contains 15–20 lobes that radiate around the nipple and are separated from each other by adipose tissue. Within the lobes are lobules that contain clusters of milk-producing cells called alveoli. Lactiferous ducts drain the alveoli into openings in the nipple. Breast development at puberty is influenced by ovarian hormones.
EXTERNAL GENITALIA (VULVA)
The clitoris is an area of erectile tissue about 5–6 mm in length and 6–8 mm in diameter situated between and partly covered by the anterior junction of the labia minora. It contains a large number of free nerve endings, which make it very sensitive to stimulation. Between the vaginal opening and the anus is a muscular layer covered with skin, the perineum.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree