CHAPTER 1
Reproductive Anatomy, Physiology, and the Menstrual Cycle
1 Identify and locate the female organs of reproduction.
2 Describe the physiologic functioning of the female reproductive system.
3 Identify the parameters of sexual maturation and menstruation, including cycle interval, duration of menstrual flow, and perimenopause.
4 Describe the physiologic changes in the ovaries, uterus, and cervix that occur during the menstrual cycle.
5 Explain the physiologic pathways of the hypothalamic-pituitary-ovarian axis and their relationship to the normal menstrual cycle.
6 Describe variations in anatomy that affect reproduction.
7 Describe variations in physiology that affect reproduction.
8 Identify the common variations in the menstrual cycle.
9 Analyze the data from a reproductive history and physical examination to determine overt and covert anatomic and physiologic factors that could affect pregnancy.
10 Prepare a set of nursing interventions for teaching pertinent concepts of anatomy and physiology to clients.
INTRODUCTION
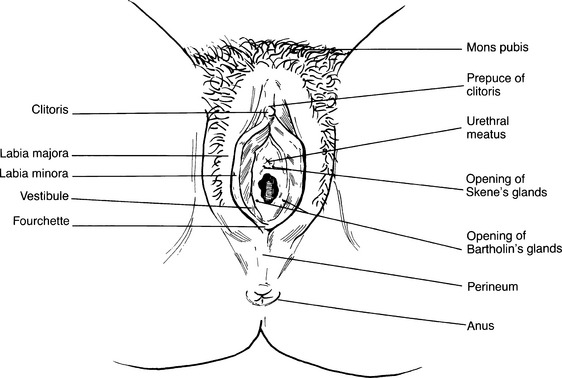
A External genitalia: Vulva (Figure 1-1)
1. Mons pubis (or mons veneris)
a. A rounded pad of subcutaneous fatty tissue over the symphysis pubis; covered with pubic hair
b. Function is the protection of the symphysis pubis during intercourse.
a. Two rounded folds of fatty and connective tissues, covered with pubic hair, that extend from the mons pubis to the perineum
a. Narrow folds of hairless skin located within the labia majora; begin beneath the clitoris and extend to the fourchette.
b. Highly vascular and rich in nerve supply; glands lubricate the vulva
c. Function is erotic; swell in response to stimulation and are highly sensitive.
4. Prepuce of clitoris is a hoodlike covering over the clitoris.
a. An erectile organ located beneath the pubic arch that consists of shaft and glans
b. Secretes smegma, a pheromone (olfactory erotic stimulant)
c. Extremely sensitive to touch, pressure, and temperature
a. An oval-shaped area whose boundaries are the clitoris, fourchette, and labia minora; contains the following:
(a) Tough, elastic, perforated, mucosa-covered tissue that forms a rim around the internal perimeter of the vaginal introitus
(b) Hymenal opening might be absent or small, impeding menstrual flow and intercourse.
(c) Characteristics of the hymen vary widely among women; the presence or absence of the hymen can neither confirm nor rule out sexual experience.
7. Fourchette is a point located midline below the vaginal opening where the labia majora and labia minora merge.
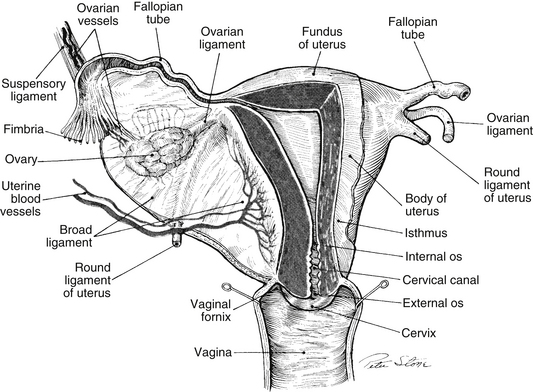
B Internal organs (Figure 1-2)
a. A hollow tubular structure located behind the bladder and in front of the rectum; extends from the introitus to the cervix
b. Thin-walled; composed of smooth muscle; capable of great distention as well as collapse
c. Lined with a glandular mucous membrane that is arranged in folds called rugae
d. Highly vascular and relatively insensitive; adds little sensation for the female during coitus
e. Functions as the outflow track for menstrual fluid and for vaginal and cervical secretions, the birth canal, and the organ for coitus
a. Located behind the symphysis pubis between the bladder and the rectum
b. Muscular, hollow, smooth, mobile, nontender, firm, and symmetric
c. In a woman who has not been pregnant, uterine size ranges from 5.5 to 8 cm (2.2 to 3.2 inches) long, 3.5 to 4 cm (1.4 to 1.6 inches) wide, and 2 to 2.5 cm (0.8 to 1 inch) deep; size increases after childbirth.
d. Is similar in shape to a light bulb or pear
e. Is a single organ composed of four distinct areas:
(a) The upper, rounded portion above the insertion of the fallopian tubes
(b) Beginning at the 20th week of pregnancy, uterine size is measured in centimeters from the height of the fundus to the top of the symphysis pubis.
(2) Corpus (or body) is the main portion of the uterus, located between the cervix and the fundus.
(4) Cervix (or opening of the uterus)
(a) Divided into two portions: the portion above the site of attachment of the cervix to the vaginal vault is called the supravaginal portion; the portion below the attachment site that protrudes into the vagina is called the vaginal portion.
(b) Composed of fibrous connective tissue
(c) Diameter varies from 2 to 5 cm (0.8 to 2 inches), depending on childbearing history.
(d) Length is usually 2.5 to 3 cm (1 to 1.2 inches) in a nonpregnant woman.
(e) Vaginal portion is smooth, firm, and doughnut shaped, with visible central opening called the external os.
(f) Internal os is the opening of the cervix inside the uterine cavity.
(g) Cervical canal forms the passageway between the external os of the cervix and the uterine cavity; major feature is the ability to stretch to a diameter large enough to allow passage of an infant’s head and then to return to a closed position.
(h) Produces mucus in response to cyclic hormones; thickened cervical mucus can impede the passage of sperm and bacteria; thin cervical mucus facilitates the movement of sperm and prolongs sperm life; observation of changes in cervical mucus is important in fertility awareness methods of family planning.
(i) At maturity the cervical vaginal surface is covered with squamous epithelium; cervical canal is lined with columnar epithelium.
[i] Area where two types of epithelium meet is called the squamocolumnar (SC) junction; also called the transformation zone or T-zone.
[ii] Prior to puberty, the cervix is covered with columnar epithelium, and the SC junction is located on the outer surface of the cervix.
[iii] Beginning at puberty, under the influence of estrogen, the SC junction gradually recedes back toward the external os, with squamous epithelium replacing the columnar epithelium.
[iv] The SC junction is the most frequent site of changes associated with the development of cervical cancer; cells from the SC junction and other areas of the cervix are assessed via the Papanicolaou (Pap) test.
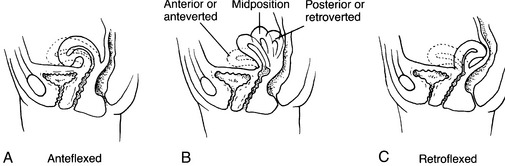
f. Uterine position (Figure 1-3)
g. Uterine support (see Figure 1-2)
(1) Anterior ligament extends from the anterior cervix to the bladder.
(2) Cardinal (transverse) ligaments
(3) Posterior ligament extends from the posterior cervix to the rectum.
(a) Endometrium is a highly vascular mucous membrane that responds to hormone stimulation first by hypertrophy and then by secretion to prepare to receive the developing ovum; sloughs if pregnancy does not occur, resulting in menstruation; if pregnancy occurs, sloughs after delivery.
(b) Myometrium is composed of smooth muscle in layers.
[i] Outer layer is composed of longitudinal fibers, which predominate in the fundus and provide power to expel the fetus.
[ii] Middle layer is composed of fibers interlaced with blood vessels in a figure-eight pattern; contraction following childbirth helps control blood loss.
[iii] Inner layer is composed of circular fibers concentrated around the internal cervical os; provides sphincter action to help keep the cervix closed during pregnancy.
(c) Parietal peritoneum covers most of the uterus, except for the cervix and a portion of the anterior corpus.
3. Fallopian tubes or oviducts (see Figure 1-2)
a. Attached to the uterine fundus and curve around each ovary
b. Provide a passageway for the ovum into the uterus
c. 10 cm (4 inches) in length and 0.6 cm (0.25 inch) in diameter
(1) Infundibulum: the most distal portion; funnel-shaped; covered with fimbriae that guide the ovum into the tube by creating a wavelike motion
(2) Ampulla: next most distal portion of the fallopian tube and site of fertilization
(3) Isthmus: narrowed part of the fallopian tube; closest to the uterus
(4) Interstitial: narrowest portion, which passes through the uterine myometrium and opens into the uterine cavity
4. Ovaries (female gonads) (see Figure 1-2)
a. Comparable with the testes in the male
b. Located on either side of the uterus, below and behind the fimbriated ends of the oviducts
c. Supported by the ovarian ligaments and the mesovarian portion of the broad ligament
d. Similar to shelled almonds in size and shape; smooth, mobile, slightly tender, and firm
e. Functions include ovulation and production of hormones (estrogen, progesterone, and androgens).
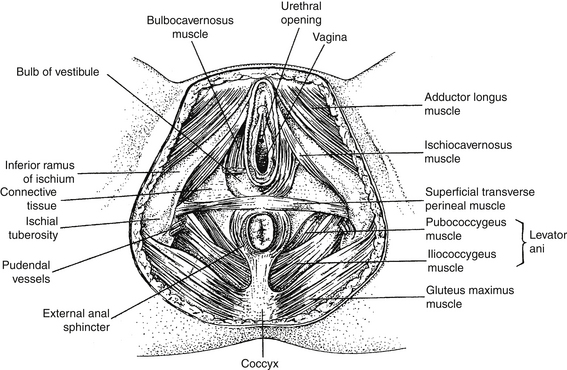
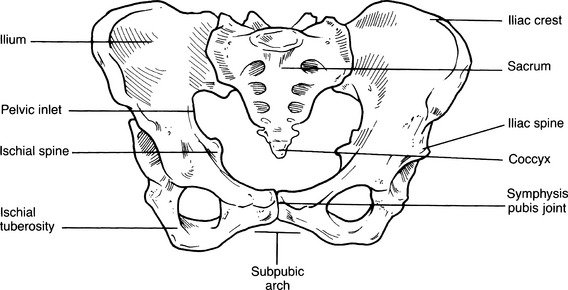
C Support for organs of reproduction
a. Blood is supplied to the pelvis by arteries branching from the hypogastric artery (which branches from the iliac artery, a division of the aorta).
b. Major pelvic arteries include the uterine, vaginal, pudendal, and perineal arteries.
c. Ovarian arteries branch directly from the aorta.
d. Lymphatic drainage is accomplished from the uterus, ovaries, and fallopian tubes to nodes around the aorta, with some use of the femoral, iliac, and hypogastric nodes.
(1) Support of the suspended internal organs of reproduction
(2) Support for sphincter control, allowing for expansion of the vagina with expulsion of the fetus, and closure of the vagina after delivery
b. Pelvic diaphragm (Figure 1-4)
c. Urogenital diaphragm (see Figure 1-4): transverse perineal muscles
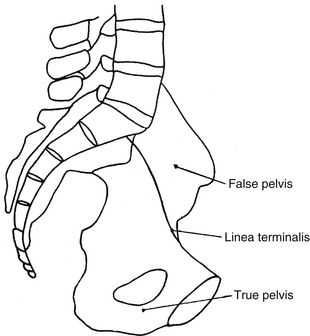
a. Functions include support and protection of pelvic structures, and support for a growing fetus during gestation.
c. Ilium, ischium, and pubic bones fuse after puberty; the pelvic bone then is called the right or left innominate bone.
(1) Area of the pelvis above the anterior, superior iliac spines
(2) Provides no useful data for estimating the size of the birth canal
e. True pelvis (see Figure 1-6)
(1) Composed of three pelvic planes
(a) Pelvic inlet is bordered by anterior and superior iliac spines and the sacral promontory.
(b) Midpelvis is the area between the inlet and the outlet.
(c) Pelvic outlet is bordered by ischial tuberosities and the coccyx.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree