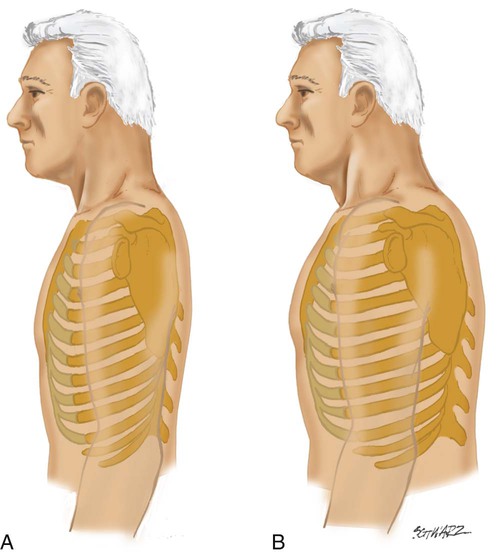
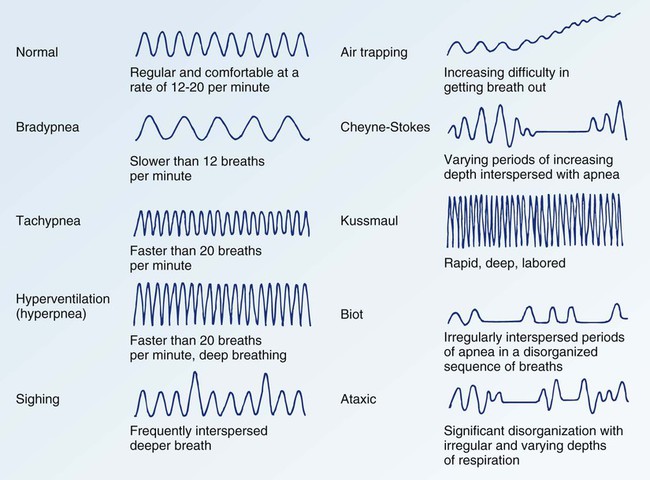
Chapter 18 The initial presentation of the patient determines the rapidity and direction of the interview. For a patient in acute distress, the history should be curtailed to just a few questions about the patient’s chief complaint and precipitating events. For a patient in no obvious distress, the history should focus on five areas: 1) review of the patient’s present illness; 2) overview of the patient’s general respiratory status; 3) examination of the patient’s general health status; 4) survey of the patient’s family and social background; and 5) description of the patient’s current symptoms.1 Specific items regarding each of these areas are outlined in the Box 18-1. Symptoms that are common in the pulmonary patient include dyspnea, cough, wheezing, edema, palpitations, fatigue, chest pain, hemoptysis, and sputum abnormalities. Information should be elicited regarding the location, onset and duration, characteristics, setting, aggravating and alleviating factors, associated symptoms, and efforts to treat the symptoms. If the cough is productive, the patient should be asked questions about the color, amount, odor, and consistency of the sputum.2–5 Four techniques are used in physical assessment: inspection, palpation, percussion, and auscultation. Inspection is the process of looking intently at the patient. Palpation is the process of touching the patient to judge the size, shape, texture, and temperature of the body surface or underlying structures. Percussion is the process of creating sound waves on the surface of the body to determine abnormal density of any underlying areas. Auscultation is the process of concentrated listening with a stethoscope to determine characteristics of body functions.6,7 Inspection of the patient should focus on three areas: 1) observation of the tongue and sublingual area; 2) assessment of chest wall configuration; and 3) evaluation of respiratory effort. If possible, patients should be positioned upright, with their arms resting at their sides.3 Inspection usually begins during the interview process.2 The tongue and sublingual area should be observed for a blue, gray, or dark purple tint or discoloration indicating the presence of central cyanosis. Central cyanosis is a sign of hypoxemia, or inadequate oxygenation of the blood, and it is considered to be a life-threatening condition. It occurs when the amount of reduced hemoglobin (unsaturated hemoglobin) exceeds 5 g/dL. The fingers and toes may also appear discolored, an indication of the presence of peripheral cyanosis.8 Assessment of chest wall configuration incorporates observations about the size and shape of the patient’s chest. Normally, the ratio of anteroposterior diameter to lateral diameter ranges from 1:2 to 5:7 (Fig. 18-1A).2,4,5 An increase in the anteroposterior diameter is suggestive of chronic obstructive pulmonary disease (COPD).2,4,5 The shape of the chest should be inspected for any structural deviations. Some of the more frequently seen abnormalities are pectus excavatum, pectus carinatum, barrel chest, and spinal deformities. In pectus excavatum (funnel chest), the sternum and lower ribs are displaced posteriorly, creating a funnel or pit-shaped depression in the chest. This causes a decrease in the anteroposterior diameter of the chest and may interfere with respiratory function. In pectus carinatum (pigeon breast), the sternum projects forward, causing an increase in the anteroposterior diameter of the chest. The barrel chest also results in an increase in anteroposterior diameter of the chest and is characterized by displacement of the sternum forward and the ribs outward (see Fig. 18-1B). Spinal deformities such as kyphosis, lordosis, and scoliosis also may be present and can interfere with respiratory function.9 Evaluation of respiratory effort incorporates observations on the rate, rhythm, symmetry, and quality of ventilatory movements.2 Normal breathing at rest is effortless and regular and occurs at a rate of 12 to 20 breaths per minute.3 There are a number of abnormal respiratory patterns (Fig. 18-2). Some of the more commonly seen patterns in patients with pulmonary dysfunction are tachypnea, hyperventilation, and air trapping. Tachypnea is manifested by an increase in the rate and decrease in the depth of ventilation. Hyperventilation is manifested by an increase in the rate and depth of ventilation. Patients with COPD often experience obstructive breathing, or air trapping. As the patient breathes, air becomes trapped in the lungs and ventilations become progressively more shallow until the patient actively and forcefully exhales.10 Other areas of focus for the careful assessment are patient position, active effort to breathe, use of accessory muscles, presence of intercostal retractions, unequal movement of the chest wall, flaring of nares, and pausing midsentence to take a breath.2,4,5 The presence of other iatrogenic features, such as chest tubes, central venous lines, artificial airways, and nasogastric tubes, should be identified because they may affect assessment findings. Palpation of the patient should focus on three aspects: 1) confirmation of the position of the trachea; 2) assessment of thoracic expansion; and 3) evaluation of fremitus. The thorax should be assessed for any areas of tenderness, lumps, or bony deformities. The anterior, posterior, and lateral areas of the chest should be evaluated in a systematic fashion.2 Confirmation of the position of the trachea is performed to verify that the trachea is midline. It is assessed by placing the fingers in the suprasternal notch and moving upward (Fig. 18-3).10 Deviation of the trachea to either side may indicate a pneumothorax, unilateral pneumonia, diffuse pulmonary fibrosis, a large pleural effusion, or severe atelectasis. With atelectasis, the trachea shifts to the same side as the problem, and with pneumothorax, the trachea shifts to the opposite side of the problem.9 Assessment of thoracic expansion involves measuring the degree and symmetry of respiratory movement. It is assessed by placing the hands on the anterolateral chest with the thumbs extended along the costal margin, pointing to the xiphoid process, or on the posterolateral chest with the thumbs on either side of the spine at the level of the 10th rib (Fig. 18-4). The patient is instructed to take a few normal breaths and then a few deep breaths. Chest movement is assessed for equality, which signifies symmetry of thoracic expansion.3,9,10 Asymmetry is an abnormal finding that can occur with pneumothorax, pneumonia, or other disorders that interfere with lung inflation. The degree of chest movement is felt to ascertain the extent of lung expansion. The thumbs should separate 3 to 5 cm during deep inspiration.5,10 Lung expansion of a hyperinflated chest is less than that of a normal one.5,10
Pulmonary Clinical Assessment
History
Physical Examination
Inspection
Tongue and Sublingual Area
Chest Wall Configuration
Respiratory Effort
Additional Assessment Areas
Palpation
Position of the Trachea
Thoracic Expansion
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Pulmonary Clinical Assessment
Get Clinical Tree app for offline access