Public Health Nursing in the United States: A History
Sandra B. Lewenson
|
The history of public health nursing is continuous. What we are, we have become through those that have gone before, and the great leaders are of no country, but of the world (Gardner, 1933, p. 15).
LEARNING OBJECTIVES
At the completion of this chapter, the reader will be able to
Define the various terms used to describe the work of nurses who have practiced in public health nursing over time.
Describe the history of public health nursing.
Explain the relevance of the history of nursing to current issues in public health nursing.
KEY TERMS
Community health nurse
District nurse
Home care nurses
Populations
Public health nurse
Visiting nurse
Hiestand (1982) called for the historian to reflect on “practice as it changed over time” because of its relevance to “understanding the nurses’ experience” (p. 11). The purpose of this chapter is to reflect on the practice of public health nursing by examining the nurse’s evolving experience in this role. This experience has been influenced by the type of agency where nurses worked, the community in which they served, the economic climate, the advances made in the sciences and technology, and other sociopolitical factors that
shaped the kind of work being done (Bryant, 1968; Stewart & Vincent, 1968). The evolution of public health nursing reflects the response to these factors and the transformation that these nurses made in meeting the needs of individuals, families, populations, and communities (American Nurses Association {ANA}, 2007). As the public health nursing role evolved, so did the nomenclature, leading some to question what a public health nurse is. This chapter examines public health nursing and the shift in roles as the names changed throughout the late 19th century until today. It also highlights the educational requirements for the public health nurse because as the titles and responsibilities changed to meet the needs of society, so did the educational requirements and expectations. Although this chapter seeks to explain the history of public health nursing and to address the question of what is a public health nurse, it raises more questions for the reader to consider than provides answers.
shaped the kind of work being done (Bryant, 1968; Stewart & Vincent, 1968). The evolution of public health nursing reflects the response to these factors and the transformation that these nurses made in meeting the needs of individuals, families, populations, and communities (American Nurses Association {ANA}, 2007). As the public health nursing role evolved, so did the nomenclature, leading some to question what a public health nurse is. This chapter examines public health nursing and the shift in roles as the names changed throughout the late 19th century until today. It also highlights the educational requirements for the public health nurse because as the titles and responsibilities changed to meet the needs of society, so did the educational requirements and expectations. Although this chapter seeks to explain the history of public health nursing and to address the question of what is a public health nurse, it raises more questions for the reader to consider than provides answers.
What Is a Public Health Nurse?
Early public health nursing leader Mary Gardner raised the question of what to call the nurse who provided care in the home in the preface of her 1933 book, Public Health Nursing. She decided on using the term “public health nurse” throughout her book instead of the other possible terms attributed to this role. Gardner (1933) explained as follows:
Certain questions of nomenclature have arisen, chief among them the name to be given to the nurse and to her work as described in these pages. In view of the present tendency toward more generalized methods of administration, and also because the functions of the various nurses are now so closely interwoven, the names “visiting nurse” and “visiting nursing association” have not been used in this book. “Public health nurse” and “public health nursing” have been substituted throughout to describe all types of nurses and organizations. (p. x)
Others questioned who was considered to be a public health nurse and the activities of this nurse. For example, Welsh (1936) wrote an article entitled, “What Is Public Health Nursing?,” where she exclaimed that the very need for public health nursing to define itself after 50 years of organized activity was in itself an “indication of the lack of unity within the field itself” (p. 452). Confusion about who and what a public health nurse was stemmed from the increasing specializations that public health nurses were branching into other areas, such as tuberculosis nurses, maternity nurses, infant welfare nurses, and other specialty areas aside from visiting nurses.
The change in names used to describe the person who provided the care in the home has perpetually confused those in health care, as well as consumers of care (Geis, 1991; Humphrey & Milone-Nuzzo, 1996; Jones, Davis, & Davis, 1987; Levin et al., 2007; Roberts & Heinrich, 1985; Welsh, 1936). In schools of nursing, for example, students take courses in public health that are often labeled community health. Faculty members debate what they consider a “good” community clinical experience. This debate usually includes whether a visiting nurse experience (“carry the bag”) or working in a health department or incorporating public health initiatives in a shopping mall or any number of combinations of experiences allow the student to understand the full dimension of public health nursing. This confusion stems from the faculty’s orientation to this specialty and from the terminology used to describe the course: Is it public health or community health or both? Clark (2008) poignantly asks
what’s in a name and tries to explicate the meaning of the various terms used to describe this specialty.
what’s in a name and tries to explicate the meaning of the various terms used to describe this specialty.
As the public health nursing role evolved, so did the names for this role. The changing names reflected the tensions between and among the stakeholders that shaped the work of public health nurses. The lack of cohesiveness of the various volunteer and public organizations and the separation of the preventive care from the curative aspects of the public health nurse’s role led Buhler-Wilkerson (1993) to write, “it is little wonder, then that the question, ‘What is a public health nurse’ has been debated for more than 80 years” (p. 1783). The history of public health nursing provides the reader with the origins of the various names, the educational requirements for these roles, and insight into the debate that continues today as to what a public health nurse is.
Evolution of the Public Health Nurse
District Nurses
District nursing began in 1859 as part of an experiment where a hospital-based, trained nurse was sent to provide nursing care to the poor in “a small district” in Liverpool, England (Hughes, 1893/1949). From that early success the promoter of this experiment, William Rathbone, expanded this work, dividing Liverpool into 18 districts and supplying each district with its own district nurse (Hughes). The adoption of this successful form of nursing spread, and various agencies began to use district nurses throughout England.
English nursing leader Dacre Craven (1889/1984) wrote about the work of the district nurse in England and called Rathbone’s experiment as the defining incident in identifying the distinct work of the district nurse. In Craven’s description of the district nurse, she includes the care of the sick poor in their homes as the main focus of a district nurse. The responsibilities of the district nurse were carefully explained in Craven’s work, A Guide to District Nursing, first published in 1889. Craven was considered one of the first superintendents of the central home where district nurses lived together. These nurses were drawn together from “the class of gentlewomen, with a view to bringing women of higher education and refinement to grapple with the special difficulties of the work” (Hughes, 1893/1949, p. 113).
District nurses addressed the health of the poor in the community and needed to have a “real love for the poor and a desire to lessen the misery” (Craven, 1889/1984, p. 1) that was found in the homes. Concern for the family and bringing cleanliness to the patient, the family, and the environment in which the family lived was part of the district nurse’s role. The district
nurse needed to know about the sanitary and charitable organizations in the district where the patients lived. In this way, when sanitary problems arose, such as a defective water supply, or “untrapped” cesspools or “unemptied dustbins,” the nurse would notify the appropriate “sanitary committee of the district … who {would} take legal steps, if necessary, to compel the landlord to put the premises into a proper sanitary condition” (Craven, 1889/1984, p. 11). The daily work consisted of care of the sick poor and enabled the nurse to observe the sanitary conditions in the home that affected the health of the patient, the family, and the community (or district) in which the patient lived. Craven (1889/1984) gave the following examples of the sanitary work of the district nurse:
nurse needed to know about the sanitary and charitable organizations in the district where the patients lived. In this way, when sanitary problems arose, such as a defective water supply, or “untrapped” cesspools or “unemptied dustbins,” the nurse would notify the appropriate “sanitary committee of the district … who {would} take legal steps, if necessary, to compel the landlord to put the premises into a proper sanitary condition” (Craven, 1889/1984, p. 11). The daily work consisted of care of the sick poor and enabled the nurse to observe the sanitary conditions in the home that affected the health of the patient, the family, and the community (or district) in which the patient lived. Craven (1889/1984) gave the following examples of the sanitary work of the district nurse:
Sometimes there is a plague of flies in the room, which can be traced to some foul or decaying animal or vegetable refuse. When the nurse carries down the dust and ashes to the dustbin she sees whether it ought to be emptied, and ascertains when this was last done. As she fetches water for the kettle she can find out whether it is from an impure and uncovered cistern, and as she empties the slops of her patient she ascertains whether the w.c. is in a good sanitary condition, and with a separate cistern from that used for drinking purposes (and she can herself occasionally flush the pan of the w.c). (pp. 11-12)
Another important role of the district nurse was to educate patients, friends, and family about the need for a sanitary environment. The nurse taught about the need for personal cleanliness and hygiene, and she herself was expected to be a role model of both. The nurse’s uniform, as Craven (1889/1984) described, reflected a clean and neat appearance. The district nurse was to be a paragon of excellence in the way she cared for the sick poor, managed the sanitation of the environment, and educated others about cleanliness and sanitary principles. She also assumed the responsibility for the care of the dying patient and the dead. Craven (1893/1949) wrote that district nurses were instructed on the “best positions in which to place the dying, according to their ailment … so that they might breathe to the last without unnecessary effort or pain” (p. 133).
As the district nurses that Craven (1889/1984) wrote about carried on their work, they also were responsible for keeping records of what they did. Each district nurse spent time on paperwork documenting her caseload, the time she spent, and the care she provided in each home. The nurses shared this information with the superintendent of the district nurses, who collated their reports into a monthly report. The superintendent kept a log of all the cases the nurses managed. Based on the district nurses’ work, reports included the number of new cases per month, the length of visits, and the number of visits required by the patients (Craven, 1889/1984, p. 131). Superintendents rated the work done and the data collected. For example, they would use ratings such as “excellent,” “good,” “moderate,” “imperfect,” or “nil” to rank such things as the patient’s status; the cleanliness of the patient, the room, utensils, and beds; and the various kinds of treatments, like sponge baths, mouth care, precautions against bed sores, wound care, and other treatments. Records of various types of cases such as typhoid fever, diphtheria, puerperal disease, scarlet fever, obstetrical cases, and care of the newborn were also kept. In addition, the superintendent’s report included an evaluation of the probationers, who acted as the district nurses, on their ability to observe the sick and manage the care of the sick (Craven, 1889/1984).
Knowledge about the work of these early district nurses in England spread to the United States. In 1893, Amy Hughes, Superintendent
of Nurses at the Metropolitan and National Nursing Association, one of the agencies to form in London, came to the United States to speak before the International Congress of Charities, Correction, and Philanthropy in Chicago. She explained to the American audience that “district nursing is the technical name for the work of nursing the sick poor in their own homes” (p. 111). Interest in district nursing spread as trained nurses from the early Nightingaleinfluenced training schools sought ways to improve the health of those who lived in the community. Miss C. E. Somerville, from Lawrence General Hospital in Massachusetts, said, “the last quarter of the century was well advanced when America caught the reflection of England’s light, and the era of trained nursing for the poor began in this country” (Somerville, 1893/1949, p. 119).
of Nurses at the Metropolitan and National Nursing Association, one of the agencies to form in London, came to the United States to speak before the International Congress of Charities, Correction, and Philanthropy in Chicago. She explained to the American audience that “district nursing is the technical name for the work of nursing the sick poor in their own homes” (p. 111). Interest in district nursing spread as trained nurses from the early Nightingaleinfluenced training schools sought ways to improve the health of those who lived in the community. Miss C. E. Somerville, from Lawrence General Hospital in Massachusetts, said, “the last quarter of the century was well advanced when America caught the reflection of England’s light, and the era of trained nursing for the poor began in this country” (Somerville, 1893/1949, p. 119).
Early district nursing associations, also called visiting nurse associations, organized in the United States. Some were established along religious missionary lines that expected the care of the sick to include a religious concern for the well-being of the patient. An early example of this was the Woman’s Branch of the New York City Mission and Tract Society, which in 1877 used trained nurses to provide care to the sick in the home in New York City (Lewenson, 1993; Somerville, 1893/1949). Two years later the Ethical Culture Society offered a nondenominational visiting nurse service that rendered care to the sick poor. Both associations began almost 20 years before the secular visiting nurse service was founded by Lillian Wald and Mary Brewster in 1893 at the Henry Street Settlement. Other early district and visiting nurse associations opened in Boston, Chicago, Philadelphia, and other cities across the United States, offering care to the sick poor and those of moderate means. They shared a common goal and assumed many of the same roles as their counterpart district nurses did in England (Somerville, 1893/1949).
Nightingale’s paper “Sick Nursing and Health Nursing,” presented at the Chicago World Fair in 1893, described the district nurse as providing care to the sick at home, as well as someone who assumed the work as a health missioner. A health missioner required additional training in how to teach healthy behaviors to mothers in the community and in the home. Nightingale outlined some of the content that was included in their additional training in areas such as sanitary conditions in the home, management of health of adults, women in childbearing years “before and after confinement,” and infants and children (Nightingale, 1893/1949, p. 41).
Nightingale (1893/1949) believed that to improve the health of infants and babies, mothers needed to learn about healthier lifestyle behaviors. Nightingale used a population focus to explain why these health missioners needed to be concerned about the health of infants and babies. She wrote that,
The life duration of babies is the most ‘delicate test’ of health conditions. What is the proportion of the whole population of cities or country which dies before it is five years old? We have tons of printed knowledge on the subject of hygiene and sanitation. The causes of enormous child mortality are perfectly well known: they are chiefly, want of cleanliness, want of fresh air,
careless dieting and clothing, want of whitewashing … in one word, want of household care of health. (p. 29)
careless dieting and clothing, want of whitewashing … in one word, want of household care of health. (p. 29)
Nightingale’s idea about health nursing extended to the community, and she summarized this in her paper by saying, “The health of the unity is the health of community. Unless you have the health of the unity there is no community health” (Nightingale, 1893/1949, p. 35).
The concept of health missioners or health nursing was embedded in the work of the visiting nurse in the United States as these nurses added to their work the ideas generated by the public health movement that was calling for ways to keep communities healthy. The public health movement was ongoing in the United States since the mid-1800s, when the Shattuck commission identified the need for the creation of local health boards that would collect statistical data on the population, including records of marriages, births, and deaths. States were called on to investigate “the cause of disease, abatement of the smoke nuisance, adoption of means for public health education, and other far-reaching measures” (Beard, 1922, p. 142). Scientific discoveries about the causes of the spread of certain diseases like yellow fever, malaria, tuberculosis, or poliomyelitis further advanced public health initiatives. Visiting nurses cared for the sick at home and provided the families they visited with information about how to keep their families and communities healthier.
Public health nursing leader Lillian Wald attended the Chicago exposition and was greatly influenced by Nightingale’s paper describing health nursing (Haupt, 1953). Haupt wrote that Wald had “accepted Florence Nightingale’s concept of ‘health nursing’ and put the word ‘public’ in front of it so that all the people would know that they could use it” (p. 81). The nurses at the Henry Street Nurses Settlement, for example, cared for the sick at home and offered classes to mothers on how to keep their families healthier. Although the term “health missioner” is rarely seen in the literature describing public health nursing in the United States, the dimension of health promotion and disease prevention continued to be imbued in the work of public health nursing.
Visiting Nurse
Public health nursing leader Lavinia Dock addressed the issue of nomenclature in her text, A Short History of Nursing (Dock & Stewart, 1938). Dock wrote that the first evidence of the term “visiting nursing” was found in the early records of St. John’s House, England, which began in 1848. During that period cholera and smallpox were rampant in England and the United States, and “Anglican and Catholic sisters spent their lives in visiting the poor and caring for the sick under the most terrible conditions” (Dock & Stewart, 1938, p. 305). By the
20th century, however, the role of the visiting nurse expanded into what was to become part of the larger “public health movement.” Dock wrote, “In the twentieth century visiting nursing became one part of the broadening field of ‘public health nursing,’ as an ideal of the visiting nurse who was teacher, sanitarian, and publicspirited citizen as well as nurse, gradually took form” (Dock & Stewart, 1938, pp. 305-306). This new expanding field of public health nursing, Dock believed, was to become the “nursing of the future” (p. 306).
20th century, however, the role of the visiting nurse expanded into what was to become part of the larger “public health movement.” Dock wrote, “In the twentieth century visiting nursing became one part of the broadening field of ‘public health nursing,’ as an ideal of the visiting nurse who was teacher, sanitarian, and publicspirited citizen as well as nurse, gradually took form” (Dock & Stewart, 1938, pp. 305-306). This new expanding field of public health nursing, Dock believed, was to become the “nursing of the future” (p. 306).
As mentioned earlier, public health nurses were closely aligned with the public health movement that flourished during the early 20th century. Fitzpatrick (1975a) described the noted public health expert Charles Winslow’s identification of three phases of the public health movement: “the phase of empirical environmental sanitation, the bacteriological phase, and the educational phase” (p. 6). The fact that nurses were already engaged in providing both health care and health education within communities led Winslow and others to acknowledge the value public health nurses brought to the larger public health movement (Fitzpatrick, 1975a).
Modern Nursing Movement
The history of the modern nursing movement in the United States began in 1873 as Nightingale’s work influenced the opening of schools for nurses in New York, Connecticut, and Massachusetts (Lewenson, 1993). It was a time of great change for women who sought a way to financially support themselves in some kind of labor outside of the home. Women read a description about one of the new training schools that had started at Bellevue Hospital in New York City in The Century Magazine (North, 1882), describing nursing as a “new profession for women” (p. 38). Once a nursing student completed the apprenticeship training at one of these hospital schools, however, she was sent out as a “trained nurse” into the community without the security of hospital employment. Instead of hiring their graduates, hospitals typically used their next class of nursing students to staff the hospital. A trained nurse consequently had to find employment elsewhere and usually worked as a private duty nurse, caring for one patient in the home setting, or as a public health nurse, working in public or privately-funded organizations with responsibilities for visiting patients in their homes and promoting health in the community.
By 1893, 20 years after the first few Nightingale-influenced training schools began, nursing superintendents of the schools that had already opened joined together with other women from around the world at the now famous Chicago World’s Fair. It was at this international conference that professional nursing organizations in the United States began. The first organization to form was the American Society of Superintendents for Nurses, which was started by pioneering nursing superintendents who wanted to establish standards and control over the education and practice of nursing. These leaders banded together in 1893 and by 1912 became known as the National League of Nursing Education, which changed its name again in 1952 to the current title, the National League for Nursing (NLN). As this group formed, the leaders, Isabel Hampton Robb, Lavinia Dock, and others, saw the need to organize nurses working at the bedside. The need to control practice; lobby for state nursing registration laws, which were nonexistent at the time; and support those nurses in financial trouble led to the formation of the Nurses Associated Alumnae of the United States and Canada in 1896, which in 1911 became known as the American Nurses Association (ANA).
This need to control and standardize nursing education and practice extended to another group of nurses, marginalized because of racial bias.
Many African American nurses were excluded from joining the ANA as a result of a shift to statewide membership in the organization. Once that occurred in 1916, individual nurses no longer could join and relied on membership through their state nurses associations (Carnegie, 1991; Lewenson, 1993). Racist policies of many states, particularly in the South, prohibited African American nurses from membership and left them without the support of a professional organization. This meant issues such as control of education in their nursing schools and control of practice through state registration laws that often discriminated against them would be left unattended until 1908, when the National Association of Colored Graduate Nurses (NACGN) formed. Nursing leader Martha Franklin sought assistance from other African American nurses to establish this organization to support the needs of black nurses in the United States. This organization lasted from 1908 until 1952, when integration into the ANA was achieved (Carnegie, 1991).
Many African American nurses were excluded from joining the ANA as a result of a shift to statewide membership in the organization. Once that occurred in 1916, individual nurses no longer could join and relied on membership through their state nurses associations (Carnegie, 1991; Lewenson, 1993). Racist policies of many states, particularly in the South, prohibited African American nurses from membership and left them without the support of a professional organization. This meant issues such as control of education in their nursing schools and control of practice through state registration laws that often discriminated against them would be left unattended until 1908, when the National Association of Colored Graduate Nurses (NACGN) formed. Nursing leader Martha Franklin sought assistance from other African American nurses to establish this organization to support the needs of black nurses in the United States. This organization lasted from 1908 until 1952, when integration into the ANA was achieved (Carnegie, 1991).
Sophia Palmer, first editor of the American Journal of Nursing, wrote that, “Organization is the power of the age. Without it nothing great is accomplished” (Palmer, 1897/1991, p. 297). Organizations formed throughout the country, addressing many of the Progressive Era issues touching on the social, economic, and political welfare of the population. Nurses, by virtue of their education and practice, were aware of the connection between a healthy society and the right to vote (Lewenson, 1993). Concern for women’s rights extended into the discussions of the NLN and the ANA, leading to organizational support of a woman’s right to vote by 1912. The NACGN also supported women’s rights initiatives, as evidenced by its support of the work of the International Council of Nurses in that area. The NACGN had sent a delegation years ahead of both the NLN and the ANA to participate in discussions related to women’s rights around the globe (Lewenson, 1993).
Public Health Nursing Emerges
Throughout the late 1800s and early 1900s, Lavinia Dock advocated suffrage for women and wrote extensively about this issue in the American Journal of Nursing and other journals of that period. Dock aligned the vote with health care and said that without it, nurses would not be able to effectively improve the health of society (Lewenson, 1993). Concern for the public’s health was shared by others like Lillian Wald and Mary Brewster, who founded the Henry Street Settlement in New York City’s Lower East Side in 1893 to address the health of the people who lived there. Graduates and friends from the New York Hospital training school, Wald and Brewster opened the nurses’ settlement house in 1893 (2 years after they had graduated from the training school) to care for the population of immigrants who flooded into the United States during the late 19th and early 20th centuries. The spread of illness became a real threat to the many Americans who lived in the overcrowded cities and experienced firsthand the diversity of those who immigrated here (Fitzpatrick, 1975a; Lewenson, 1993).
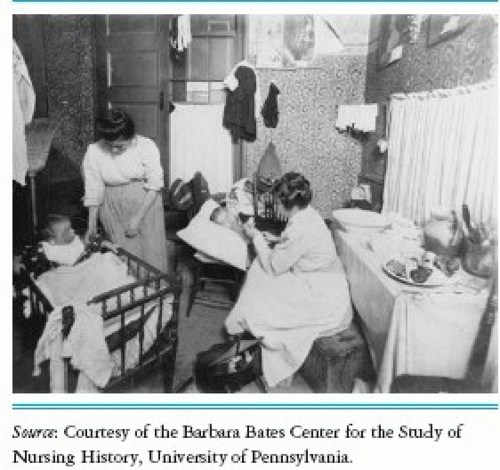
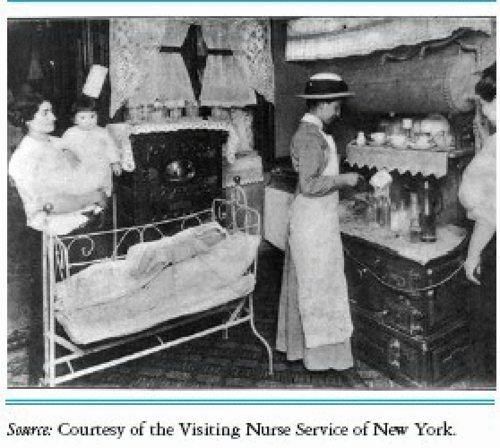
Buhler-Wilkerson (1985) said the impetus of the wealthier parts of society to improve the health of the poor stemmed, in part, from an understanding of the germ theory along with the idea that infectious diseases could be spread easily to their own families and communities by those immigrants who “sewed clothes in their filthy tenement homes or who processed food” (p. 1155). Early visiting nurses were hired by philanthropic women who sought to provide the urban poor with assistance during times of illness. According to Buhler-Wilkerson (1985),
the nurses hired by these lady philanthropists were to bring their shared vision of the “good society” by bringing “care, cleanliness, and character to the homes of the sick poor” (p. 1155). Nurses were to teach the families they visited about the ways of American life that would lead to the prevention of disease and promotion of health. Fear of the spread of illness prompted some of the concerns of those nurses and their benefactors in bringing health care to the homes of the sick poor (Buhler-Wilkerson, 1985).
the nurses hired by these lady philanthropists were to bring their shared vision of the “good society” by bringing “care, cleanliness, and character to the homes of the sick poor” (p. 1155). Nurses were to teach the families they visited about the ways of American life that would lead to the prevention of disease and promotion of health. Fear of the spread of illness prompted some of the concerns of those nurses and their benefactors in bringing health care to the homes of the sick poor (Buhler-Wilkerson, 1985).
Dock worked at the Henry Street Settlement alongside Wald and other colleagues, engaging in what we now call primary healthcare activities, including visiting homes of those who needed care related to an illness, participation in well-baby clinics, case finding, health-promoting activities, surveillance, and school nurse activities. They lived within the Henry Street settlement in the same community in which they provided nursing care. It was the comprehensive visiting nurse services like the ones delivered at Henry Street that proliferated throughout the country and offered another way for nurses to support themselves while caring for individuals, families, populations, and communities. Nursing care included the care of the sick at home as well as well-baby classes and other health-promoting courses offered to the community.
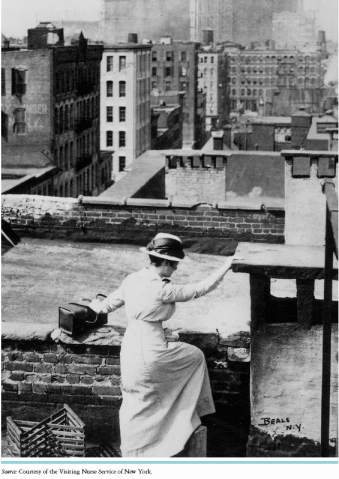
Most nurses who graduated from the nursing schools in the late 1800s worked in private duty, providing nursing services to one patient in the home. This focus differed somewhat from that of the visiting nurse. Visiting nurses saw several patients in a day, and depending on the agency in which they worked, variable fees were attached to their visit based on the patients’ ability to pay. While caring for the sick at home, they also provided much-needed health education. Often, the ability to care for the sick at home fostered a level of trust among the nurses and the families and community they served, which in turn provided them easier access to these same groups as they sought to provide health education. The work of the visiting nurse evolved into what became known as public health nursing and became a viable specialization for the graduate trained nurse. Having coined the term “public health nurses,” Wald and other nursing leaders recognized a need to control the practice of this emerging specialization in nursing and founded the National Organization for Public Health Nursing (NOPHN) in 1912 (Buhler-Wilkerson, 2001).
National Organization for Public Health Nursing
The NOPHN grew out of a desire by public health nurses to control the practice and standards of the emerging field of public health nursing. By 1912, the number of public health nurses had grown to over 3,000 and their work was supported through private and public funding (Gardner, 1933). The work was accepted by
the community and extended far beyond the care provided to the sick at home. The public health nurses’ role had expanded to meet the needs of a growing American urban and rural population— public health nurses visited patients in the home and provided additional primary healthcare services. In 1933, Gardner described the increasingly expanded and valued role of the public health nurse as follows:
the community and extended far beyond the care provided to the sick at home. The public health nurses’ role had expanded to meet the needs of a growing American urban and rural population— public health nurses visited patients in the home and provided additional primary healthcare services. In 1933, Gardner described the increasingly expanded and valued role of the public health nurse as follows:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree