Introduction
The very first requirement in a hospital is that it should do the sick no harm.
(Florence Nightingale 1859, 2001)
In this chapter you will explore what fundamental practice skills you need to learn during your foundation year and beyond so as to provide safe, high-quality practice that will enhance the health of the people that you care for and ‘do your patients no harm’.
Florence Nightingale’s remark about the environment in which health care is delivered continues to be relevant more than a century later. Furthermore, it is a sentiment that applies equally well to all sectors of health care and to all branches of nursing. Reports in the public press indicate that, despite the best endeavours of many health care workers, we cannot take for granted the fact that health care practice causes ‘no harm’. Sadly, within health care, harm is still being caused to patients. The reasons for this are not straightforward, and in some situations, such as pioneering surgery or testing out new drug regimens, risks are taken to achieve clinical outcomes. But in many cases practitioners could have avoided errors. In this chapter you will learn that you have an important part to play in maintaining safety for the people you care for and other staff.
The scope of the problem
The NHS Litigation Authority (NHSLA) is a special health authority (part of the NHS) that is responsible for handling negligence claims made against NHS bodies in England. As well as deal-ing with claims they also have an active risk-management programme to help raise standards of care in the NHS and hence reduce the number of incidents leading to claims. The NHSLA was established in 1995. Some of the following figures indicate the nature of the situation within England in terms of claims for clinical negligence. It can be seen that the NHS has to spend increasing amounts of money in cases of clinical negligence.
In 2004–2005, 5609 claims of clinical negligence and 3766 claims of non-clinical negligence against NHS bodies were received by the NHSLA. This compares with 6251 claims of clinical negligence and 3819 claims of non-clinical negligence in 2003–2004.
In 2004–2005, £502.9 million was paid out in connection with clinical negligence claims; this figure includes both damages paid to patients and the legal costs borne by the NHS. In 2003–2004, the comparable figure was £422.5 million (NHSLA 2006).
The costs of treating hospital-acquired infection, including extended length of stay, are difficult to measure with certainty, but a report in 2005 (House of Commons Committee of Public Accounts 2005) estimated that each year in England there are at least 300 000 cases of hospital-acquired infection, causing around 5000 deaths and costing the NHS as much as £1 billion. The report states that critical to managing this situation is a shift towards prevention at all levels of the NHS. This would require commitment from everyone involved and a philosophy that prevention is everybody’s business, not just the specialists’.
Not all hospital-acquired infection is preventable, since the very old, the very young, those undergoing invasive procedures and those with suppressed immune systems are particularly susceptible. However, in 1995 the Hospital Infection Working Group of the Department of Health and Public Health Laboratory Service believed that about 30% of hospital-acquired infections could be avoided by better application of existing knowledge and realistic infection-control practices. One of the most important strategies for reducing hospital-acquired infection is effective hand-washing; this is covered later in this chapter. It is probable that specific sessions will be provided by your univer-sity or placement area on hand-washing. It is vital that you attend these sessions to ensure that you are familiar with local policies and protocols.
During the 1990s, a number of prominent service failures in areas such as bone tumour diagnosis, paediatric cardiac surgery, cervical screening and wrong injection routes for powerful drugs have undoubtedly caused the public to revise their perception of the health care system and the people who work within it (Nicholls et al 2000). Although these examples may have made headline news, daily practice events remind us that we must constantly question our assumptions that health care is automatically safe practice. For example, hospital-acquired pressure sores (decubitus ulcers), methicillin-resistant Staphylococcus aureus (MRSA) and preoperative anxiety are all conditions that can have immensely detrimental physical, psychological and social consequences for people who require care and their carers. As the news about health service investigations change quite rapidly, it is worth looking at the local press for details about incidents in your area. When reading any press articles try to be critical in your reading (see Activity 13.1).
Activity 13.1
Be critical in your reading:
• How is the news reported?
• Which side of the story is being reported?
• What is the tone of the language in the report?
• Are other points of view not represented?
• Why might the news story be reported in this way?
During this activity try to draw on your own learning about providing care.
In the 21st century, given the complexity and pace of change within health care, we need to be clear and explicit in our attempts to assure both ourselves and the general public that our practices are safe and effective. Indeed, along with all the other regulatory bodies of health care practi-tioners, the Nursing and Midwifery Council of the UK (NMC) has produced a code of practice to guide practitioners and protect the public. The ‘NMC Code of professional conduct’ states that practitioners are personally accountable for their practice. This means that, once qualified, you will be answerable for your acts and omissions, regardless of advice or directions from another professional and that you have a duty of care to your patients and clients, who are entitled to receive safe and competent care.
Exercising your duty of care
You will recall that the ‘NMC Code of professional conduct’ expects you:
• To protect and support the health of individual patients and clients.
• To act in such a way that justifies the trust and confidence that the public have in you.
In this chapter we describe activities related to prevention of illness or disability or which alert nurses to potential clinical problems. All of them are aspects of care which every foundation course nursing student will encounter; they include ensuring adequate nutrition and hydration of patients and clients, preventing the complications of immobility and carrying out clinical observations. All of these nursing duties may be seen as routine; indeed, they form part of the daily work of the nurse and experience of the patient, but they are far from routine and ordinary in their consequences if they are not fulfilled as required within the patient’s care plan.
What is quality?
Everyone seems to have a general understanding of quality. It describes how individuals value particular aspects of a service or product that they either actually use or are considering using. One useful definition is:
Quality in public service can be defined as:
Others define quality as features of the service, for example: accessibility, relevance to need equity, social acceptability, efficiency and effectiveness (Maxwell 1984). This definition makes an important point as it is not only important to produce satisfaction for those health care ‘customers’ who receive the service, but to ensure that all those that need the service can and do get it. It is important to include, alongside the patient’s judgements of the service, a professional definition of need, and a professional judgement of the extent to which a service meets the patients’ needs. However, even this reference to need becomes complex as patients may not know what they need, or may ask for treatments that are really inappropriate or harmful. Therefore, the provider must gain an understanding of the perceived needs of the person. It is also important to determine who these customers are. A wide definition of customer is required; this includes staff working in the organization, employers, patients, relatives, health authority purchasers, NHS executive bodies, and health service providers.
Clinical governance was introduced into the British health care system by the Labour government in 1998. It has now become firmly established as an important framework for assuring and improving the quality of health care. It is described as: ‘a framework through which NHS organisations are accountable for continuously improving the quality of their services and safeguarding high standards of care by creating an environment in which excellence in clinical care will flourish’ (Department of Health 1998). It is important to note that this definition refers to the organizations in which individual practitioners work as well as the accountability that practitioners adhere to as part of their codes of conduct.
Clinical governance encourages safer practice and places accountability for this practice and for improving quality directly and personally with the chief executive officer of the health care institution. This means that chief executives have to focus on achieving financial balance and assuring clinical quality. Since the 1980s, quality has been high on the health care agenda. Concepts such as audit, clinical effectiveness, evidence-based practice and risk management are important elements of clinical governance.
Clinical governance is intended to foster learning from situations that go wrong. The emphasis is on learning rather than on punishment. It is designed to help practitioners, managers and all other members of the health care team to be open and honest so that risks can be identified and errors can be prevented and acted upon quickly when they do occur.
The importance of patient/client and public involvement at all levels of service development is recognized as being a critical factor in clinical governance. This has led to patient advisory councils being formed in each health care trust to provide communication channels between service providers and service users.
The National Institute for Health and Clinical Excellence (known as NICE) identifies good practice through the development of national service frameworks and clinical guidelines.
Adopting a questioning approach
The first principle of delivering safe and effective care is to adopt a questioning approach to your own practice and that of others. This involves not only being able to account for your actions, explaining why you are undertaking a particular activity and ensuring that you have the necessary knowledge and skill, but also reflecting on past situations and events to ensure that you maximize the learning available to you. You will recall that some of the techniques for using reflection in practice were introduced in Section One of this book.
Inform your practice with up-to-date knowledge and evidence
The use of the best available evidence to support practice is intended to enhance care, and lead to consistency in practice and a better-informed public. It is hoped that this in turn will contribute to an increase in the public’s confidence in the health care system. From the nurse’s perspective it is anticipated that the use of evidence to inform decision-making will assist us to account for our practice, and that the generation of such evidence will contribute to our body of knowledge as nurses. From an organization’s perspective, the use of the very best evidence to inform practice should contribute to a reduction in risk (and associated litigation), the best use of resources and an enhanced reputation.
There are many tools that provide a summary of the available evidence and help to deliver safe and effective practice (see Activity 13.2 to help identify guides to safe practice).
Activity 13.2
• Try to identify any tools in your placement area that health care professionals use to guide this practice.
• Make a list of these and then compare with the examples in the rest of this chapter.
The best available evidence is often translated locally into guidelines, protocols, principles of practice and policies which are defined as follows:
• Policies. Statements that guide decision-making and require employees of an organization to work within certain parameters.
• Guidelines. Systematically developed statements to assist practitioner and patient decisions about appropriate health care for specific clinical circumstances (NHSME 1996; further information can be found on the NHSME website).
• Protocols. A term often used to refer to a way of prescribing exactly what must be done in often high-risk situations.
• Principles of practice. A statement which explains how things should be done.
It is important for you, as a student nurse, to ensure that you become familiar with the evidence sources that are used locally. You will need to know the existence of policies and procedures in your practice placements, even if you are not expected to use them immediately. Such policies will include things such as care of drugs, patient or client control and restraint, care of patients’ property, speaking out policy, patient resuscitation, fire procedures, Mental Health Act implications for patients’ leave, child protection. There are many more, some examples of which are described later in this chapter or elsewhere in the book.
Care pathways
Integrated care pathways were introduced in Chapter 12. This approach is described in a little more detail here, together with a specific exercise to undertake. The use of care pathways has become increasingly important within health care today. A care pathway is an outline of anticipated clinical practice for a particular group of patients/clients with a particular diagnosis or set of symptoms. Successful care pathways are normally constructed by interdisciplinary care teams and are derived from evidence-based practice.
Kitchiner & Bundred (1998) comment that an integrated care pathway determines locally agreed multidisciplinary standards based on evidence, where available, for a specific patient group. Documentation associated with care pathways is an important part of clinical records as this identifies the planned clinical care.
For examples of care pathways and more in-formation, please refer to http://libraries.nelh.nhs.uk/pathways.
It is impossible in the space available here to give examples for all programme branches. Integrated care pathways are complex and result in the creation of large documents which constitute the patient’s live record of care. The use of care pathways is still being developed in the NHS but you are most likely to see those that are for patients with conditions most often encountered. Care pathways generally identify the total care regimen, including emergency admission to perhaps an accident and emergency department, through to a specialist unit such as a coronary care unit and via a general ward to discharge into the care of a rehabilitation team such as a cardiac rehabilita-tion nurse. All aspects of the care are based on evidence-based ‘best practice’ for both medicine and nursing. At this stage, you will not necessarily know about all the medical treatments and drugs used, but the pathway does show the integration of all aspects of a person’s care.
Important features of successful pathways include the following:
• They are agreed by all members of the multidisciplinary team or agencies involved in the patient’s episode of care.
• Their focus is the patient/client rather than any one professional group.
• The care contained within the pathway is based upon the very best evidence available.
Try reflecting on care pathways as suggested in Activity 13.3. Some of your reflective ideas might have included the potential of care pathways to im-prove communication, not only between those de-livering care but also between health professionals and the patient or client. This is an important benefit. Expectations are clearly mapped out in advance. Care pathway development necessitates the review of existing practice and continually monitoring the evidence. They can also help to promote evidence-based practice and reduce unwanted variations in care delivery. You may also have identified that some of your lecturers and mentors use care pathways as teaching tools for you and other new team members. In short, care pathways promote many of the activities required to ensure the delivery of safe and effective care.
Activity 13.3
• Reflect on the description of care pathways using any of the reflective models identified in Section One of the book.
• Try to identify any advantages or limitations of care pathways.
However, care pathways are not without their critics. For example, there is a thought that they will reduce clinical judgement or be used unthinkingly, resulting in poorer, rather than enhanced, care. Clearly this depends on how they are introduced. Whether care pathways are in place or not, nurses and other health care professionals are still accountable for their actions, and decisions still need to be made about the appropriateness of standard actions for individual patients/clients. Professional judgement and patient preference cannot be suspended if practice is to be safe and effective rather than routine.
Audit
Care pathways are not the only method of ensuring that practice is evidence-based. Audit is another important strategy and widely used in all areas of health and social care today. Audit of practice is usually integrated within a care pathway, but it can be undertaken independently in conjunction with guidelines and standards. Audit involves reviewing practice and ensuring that it is in accordance with that defined as ‘the best’, and that action is taken to rectify the situation when shortfalls occur.
Care bundles
A newly emerging term within hospital-based acute settings is ‘care bundles’. This idea emphasizes the importance of clinical teams delivering the best evidence-based care to patients. The technique of ‘care bundles’ measures how often therapies that should be given are actually given in practice. If a therapy is administered as proposed under best practice guidelines, then compliance is achieved. Measuring compliance in this way gives a good focus for teams to improve the care given to patients.
An example of this type of measurement is used within the critical care area when monitoring blood glucose levels. Current research (e.g. van den Berghe et al 2003) suggests that carefully controlling blood glucose can reduce mortality. Many critical care units will have protocols related to glucose control, and these may be adhered to, but they do not record how good at actually controlling blood glucose, within the target range, the units are. In other words, the measurement of blood glucose may be taken, but appropriate measures to control a person’s blood glucose levels might not be implemented. Care bundles use agreed measurement frequencies to match best evidence against actual practice.
A very useful article that relates this concept to reducing health care associated infections has been written by Storr et al (2005). The article identifies the few critical activities that health care practitioners can undertake to help reduce health-care-acquired hospital infections. More practical information can be found in the Department of Health document ‘Saving lives’ (Department of Health 2005). This is discussed later in this chapter.
Delivering safe and effective care based on the very best evidence requires active efforts to keep up-to-date with new knowledge, and national and international strategies are in place to facilitate this process. Evidence of continuing professional development (which involves keeping up-to-date with the latest knowledge and evidence) is a requirement to remain on the professional register as a nurse and is vital if we are to be accountable practitioners, able to reason for our actions. Section One of this book provides details of the continuing professional education requirements for nurses today; this chapter reinforces the importance of this for practice.
Know your limitations
When you consider the expectations placed on nurses in practice today, it is little wonder that they are sometimes faced with new and complex situations beyond their existing knowledge and experience. For a student of nursing this is clearly to be expected, yet given the dynamic and changing face of health care it is a situation that you can expect to face well beyond registration. Progress means that as nurses we are expected continually to learn and develop our practice, for example through reflection, further academic study and supervised practice.
As discussed in Section One, nurses are accountable for their practice; that is, they must be able to explain the reasoning behind their decisions and actions. The accountability of nurses and other health care professionals is primarily to the patients/clients in their care, but nurses are also accountable to the employing organization, to other members of the profession and to the professional body, the Nursing and Midwifery Council (NMC).
Accountability means not only knowing how to carry out a particular aspect of care, but also being clear about the limitations of your knowledge and experience. Although as nursing students your accountability is limited, the principles still apply as listed in the ‘NMC Code of professional conduct’. In order to be safe in practice, it is vital that you are aware of your limitations as well as your strengths, and that you know when to seek advice and support. This may not always be easy, especially in the early stages of your programme.
Activity 13.4 ask you to explore why it might be difficult to seek help. Your response to the question might have included some, or perhaps all, of the following:
• You may have feared looking foolish.
• You may have already asked once before but were unable to remember or did not grasp the response.
• The nurses may have looked busy and you did not wish to interrupt them.
• You may have asked questions in the past and received a curt response.
Activity 13.4
Although it is an important part of providing safe and effective practice that we do not undertake tasks for which we do not feel prepared and for which we are not competent, it can sometimes be very difficult to say ‘no’ or to seek help. Why might this be the case?
It is important to understand the concept of accountability and to know how to handle situations for which you feel ill prepared. Activity 13.5 asks you to reflect on a difficult situation. Then Case history 13.1 describes a situation in which a student nurse is reflecting on facing up to her limitations and how she would act differently in future, to ensure safe and effective care.
Activity 13.5
Think of a situation in which you felt unprepared to undertake the task asked of you. Use one of the frameworks described in Chapter 2 to reflect upon this incident.
• What was your response?
• Did you undertake the task or ask for help?
• Why did you behave in this way?
• What factors influenced your judgement?
• Would you deal with the situation in the same way next time, or would you do things differently?
Case history 13.1
Knowing my limitations
It was during my first placement on an orthopaedic ward that the incident took place. My mentor had arranged for me to attend fracture clinic, something I was looking forward to. When I got there it was suggested that I join the doctor and nurse covering clinic ‘A’. I spent the first hour watching patients being booked in, called through, seen by the doctor and departing. It was interesting and a lot busier than I’d expected. I was then sent to fetch some medical notes that had been left in reception. On my return, the staff nurse was nowhere to be seen and the buzzer for the next patient was sounding. I didn’t know what to do, I looked around, and all staff appeared to have vanished. The doctor came out. I explained that I was unsure where the staff nurse had gone. He said ‘Not to worry, you can do it. Call in the next patient or we will be running late’. I had watched the staff nurse, so I did as I thought she had done. I soon realized how difficult it was. I was unfamiliar with the abbreviations used, I had never heard of half of the words used and found it quite impossible to spell them. When I was asked for the simplest thing it took me ages to find it and I just got more and more flustered.
I felt really distressed by the time the nurse returned. She apologized immediately and told me that I should have fetched someone else. I went home and worried… what if I had heard the doctor’s instructions incorrectly or if what I had managed to write down did not make sense? Would the patient get the ‘wrong’ care? I began to feel angry for being put in the situation. I was angry with both the doctor and the staff nurse, it was their fault!
On reflection the nurse was right; I should have persisted in my attempt to get some assistance, but I panicked and did not want to look foolish. The fact that I didn’t know the staff seemed to make getting help harder. I wasn’t sure how they would respond as they were clearly busy. Would they be angry? I did not want to be a nuisance.
I learned a great deal about myself from this incident. I like to be seen as competent and helpful and I find it very difficult to say ‘no’ when asked to do something.
However, I now recognize that I was putting my need to look good before the safe and effective care of the patients. Perhaps the staff nurse should not have left me, but this will happen occasionally. Although I recognize that as a student I do not carry full professional accountability in situations such as this, it is my responsibility to make the limitations of my knowledge and experience known. Next time, if faced with a situation I feel ill-prepared for, I will speak out. This will not only reduce my anxiety about being left in similar situations, but will be in the interests of safe patient care.
Professional self-regulation
Self-regulation, the type of regulation that has been granted to nurses and midwives, is a privilege granted by parliament. It is not a right. It has to be earned continually to sustain public trust and confidence in the profession. Integral to self-regulation is the onus placed on each and every member of a profession, including the nursing profession, to ensure that their practice is safe and effective. Section One covers this in some detail.
Environmental awareness begins shortly after birth and continues throughout life and, ideally, people make choices in the nature and style of their personal environment. This is true for all people, whether they are well or ill or have some form of disability, who devote much energy towards accomplishing tasks to fulfil their wish of being master of their personal environment. The quality of the health and safety of our environment is greatly affected by the environment itself, and never more so than in the health care setting, where patients and clients may be more vulnerable than when in their own homes. Florence Nightingale suggested that patients in health care settings may be harmed just by being there. As previously discussed in this chapter hospital acquired infection in the UK highlights the need for health care professionals to be vigilant about this and other potential hazards to patients. So, a major task for all is to promote and maintain a safe environment. Of course, the health and safety of staff is also important and the Health and Safety at Work etc. Act (Great Britain Parliament 1974) places a general duty on all employers to ensure the health and safety of their employees.
Promoting a safe environment is one of the many functions of the nurse. As you read at the beginning of this chapter, the Nursing and Midwifery Council (NMC) makes this explicit by requiring nurses to ensure that no action they undertake is detrimental to the safety and well-being of patients, and to ensure that they report any unsafe practice or environmental danger that might affect the safety of either patients or staff. Within this section of the chapter only four specific nursing activities are covered; these are infection control, food hygiene, moving and handling, and the safe administration of medicines. All foundation students will experience elements of these. The important issue of the prevention of pressure sores is covered later.
Infection control and the role of the nurse
Chapter 9 identified some important elements of infection and you will have noted that disposable items such as dressings, gloves, aprons, eye protection and other equipment are the norm in hospitals and in the community. To be effective, these disposable items have to be used correctly and the principles of infection need to be understood.
The document ‘Saving lives: a delivery programme to reduce healthcare associated infection (HCAI) including MRSA’ (Department of Health 2005) highlights five high-impact interventions that have been developed for the clinical practice related to infection control, each with distinct evidence-based elements of the clinical process. They are:
• Preventing the risk of microbial contamination.
• Central venous catheter care.
• Preventing surgical site infection.
• Care of ventilated patients (or tracheostomy where appropriate).
• Urinary catheter care.
This chapter focuses on the first of these high-impact changes as this is the one that is most likely to involve you as a foundation student. You will learn about the other four high-impact changes as you progress through your programme. High-impact change 1, preventing the risk of microbial contamination, is based on best evidence and highlights the key points listed in Box 13.1.
Box 13.1
High-impact change 1: preventing the risk of microbial contamination
Hand hygiene
• Decontaminate hands before and after each patient contact
• Use correct hand hygiene procedure.
Personal protective equipment
• Wear examination gloves if risk of exposure to body fluids
• Gloves are single-use items
• Gowns, aprons, eye/face protection may be indicated if there is a risk of being splashed with blood or body fluids.
Aseptic technique
• Gown, gloves and drapes as indicated should be used when invasive devices are being inserted.
Safe disposal of sharps
• Sharps container available at point of use
• No disassembling of needle and syringe
• Not passed from hand to hand
• Container should not be overfilled.
Nurses play an important role in managing aspects of these high-impact interventions. As you progress through the foundation programme into your specific branch, you will learn more about aspects of these specific procedures that are relevant to your area of practice.
What is infection?
An infection is caused when the body is invaded by pathogenic (disease-producing) organisms: either bacteria or viruses. Infection is usually accompanied by a high temperature (pyrexia) and sweating and sometimes even causes a rigor. If the infection is associated with a wound then this will be red, hot and inflamed and the patient will complain of pain around the inflamed area. All these signs and symptoms are the body’s response to the presence of a pathogen.
Box 13.2 shows how cross-infection can occur from person to person, or from implements or the atmosphere.
Box 13.2
Routes of cross-infection
• Ingestion through the mouth (e.g. ingestion of contaminated food or water).
• Inhalation through the nose (e.g. breathing in micro-organisms from the atmosphere, particularly bacteria and viruses) causing sore throats, coughs and colds, leading to chest infections. The respiratory system may also succumb to more contagious aerobic bacteria such as Mycobacterium tuberculosis, which causes tuberculosis. Patients on artificial breathing machines are especially at risk.
• Via the skin, through abrasions, wounds (including open pressure sores) and ‘compound’ fractures (i.e. the bone has broken through the skin). Burns, particularly those covering large areas of the body, are so prone to infection that these patients have to be nursed in specially designed units aimed at reducing infection to the minimum. An incision made in order to undertake an operation may be sutured afterwards, but still provides a portal of entry for infection. There is the potential for infection to occur when the skin is broken.
• Injections of any kind, intravenous fluids, central venous pressure lines, and transfusing blood and blood products including contaminated blood.
• Invasive procedures such as catheterization, bladder washouts, chest drainage, wound drainage.
• Changing of dressings.
Hospital infection
Whatever the setting, everyone who works in health care establishments is responsible for maintaining a safe environment.
Despite a great increase in the legislation governing working practice in hospitals aimed at reducing cross-infection, the situation appears to be getting worse rather than better. Parker’s statement is therefore very relevant and demonstrates that such an important issue cannot be considered to be the sole responsibility of the microbiology department or the infection control nurse. One of the simplest measures to prevent cross-infection, and probably the single most important contribution to its prevention, is hand-washing (Figure 13.1), which nurses and all clinical staff are taught as a matter of priority and yet is sometimes rushed or neglected altogether.
 |
| Figure 13.1Hand-washing. |
Disposable gloves may protect you, but they do not protect your patients unless you wash your hands and change your gloves between each procedure or patient. Reducing the spread of infection in all health care areas is a major priority. Charge nurses are being urged and supported to insist that all medical and other staff wash their hands between every patient on every round and in every clinic. Knowing how to wash your hands is important (Box 13.3) (see also Figure 13.2).
Box 13.3
Hand-washing
• The hands should be washed before and after all patient contact.
• To prevent cross-infection, jewellery should not be worn; a plain wedding ring only is permissible, and it is preferable not to wear a watch on the wrist.
• A waterproof, occlusive dressing should cover any cuts or abrasions.
• A sink with elbow- or foot-operated mixer taps is best; the temperature of the water should be adjusted so that it is comfortable and the flow steady so that it avoids splashing the surrounding area.
• Liquid soap or antiseptic detergent hand-washing solution should be used, applying sufficient to create a good lather; scrubbing the skin with a nailbrush is not recommended as this causes abrasions, but the fingernails may be scrubbed.
• Wash hands thoroughly under running water and then rinse them, making sure that all traces of soap/detergent are removed.
• Turn off the taps using elbows or feet, but keeping your hands pointing upwards, to avoid water from the wrist area and above which has not been washed coming into contact with the washed area.
• Dry hands well to minimize growth of micro-organisms and to prevent the hands from becoming sore.
• Dispose of used towels in a foot-operated waste bin.
 |
| Figure 13.2The areas of the hand most often missed during hand-washing(Nicol et al 2000). |
The operating theatre ‘scrubbing up’ area is a good area to see hand-washing performed at its best. This would be a good learning opportunity if you could arrange to visit this area.
Disposable aprons and gloves do more harm than good if they are not used and disposed of correctly. A habit of abiding by some simple principles will give greater protection to your patient against cross-infection.
Aprons
Sometimes plastic aprons are supplied in different colours for different tasks (e.g. for serving meals or doing dressings). Aprons should be worn:
• For all situations in which there is direct contact with the patient.
• Where there is contact with body fluids.
• When handling bed linen, excreta or clinical waste.
• When handling items that have been in contact with infectious disease, including clothes and books.
Box 13.4 details the procedure for the use of aprons.
Box 13.4
How to use an apron
• Wash and dry hands before putting on the apron.
• Pull the apron over your head, trying to avoid touching the hair or uniform.
• Tie the apron loosely at the back so that any liquid will quickly run off.
• Remove the apron by pulling the neckband and the sides, thus breaking the ties, and fold the apron in on itself to prevent the spread of micro-organisms.
• Do not allow your hands to touch your uniform, and discard the used apron into the yellow clinical waste bag.
• Wash and dry your hands thoroughly.
Disposable gloves (non-sterile)
The use of gloves does not reduce the need to wash the hands before and after the gloves have been worn. This is because the hands sweat and create a warm, moist environment that will encourage micro-organisms to thrive. Another reason for this is that the gloves may not completely protect the hands as they have been shown to develop tiny puncture holes that go undetected, but allow micro-organisms to enter. Seamless, single-use latex or vinyl gloves are recommended. These come in three sizes and fit either hand.
Gloves should be worn whenever patient care involves dealing with blood or other body fluids, depending on the procedure, when providing care for a patient who has an infection (e.g. hepatitis, HIV, MRSA or TB) and when giving certain intramuscular drugs (e.g. antibiotics).
Choosing the correct size of glove is important as gloves that are too large or too small could impair dexterity. If gloves are required for a clean procedure these should be taken from the clean area rather than those stored in the sluice.
Box 13.5 details the procedure for the use of gloves.
Box 13.5
Use of gloves
• Wash and dry hands thoroughly.
• Take the correct size of glove from the appropriate area.
• To remove the gloves, do not touch your wrists or hands with the dirty gloves. Using a gloved hand, pinch up the cuff of the other hand and pull the glove off inside out. Using the ungloved hand, insert it behind the cuff, and pull the other glove off, turning it inside out (Figure 13.3).
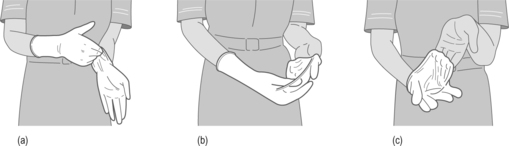 |
| Figure 13.3a–c• Safe removal of gloves(Nicol et al 2000). |
• Gloves that have been used for clinical procedures should be discarded immediately into the yellow clinical waste bag.
Eye protection
Many clinical areas provide suitable eye protection which should be used when situations determine this. Local guidelines will exist, and they are likely to include times when you may be exposed to splashes from blood or other bodily fluids.
When selecting eye protection the following should be considered:
• Eye and face protection should be selected with the particular risk in mind.
• Is the protection comfortable and does it fit properly? It should not hinder movement or visibility. Fit is important as you do not want to be adjusting eye protection with potentially contaminated gloved hands.
• The working environment; for example, spectacles or visors may be preferable in humid or hot conditions as goggles may steam up.
Every hospital trust will have an infection control team which will include a specialist infection control nurse. Infection control nurses are qualified experienced nurses, who have usually taken a further course on infection control. They are there to advise staff on how to prevent cross-infection and care for patients with infectious diseases, and to assist in the interpretation of hospital policies and procedures dealing with infection control (try Activity 13.6). They are very much involved in finding and implementing the latest research on infection control, advising on new products and updating nursing procedures. They work closely with the microbiology department and the health and safety officer.
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


