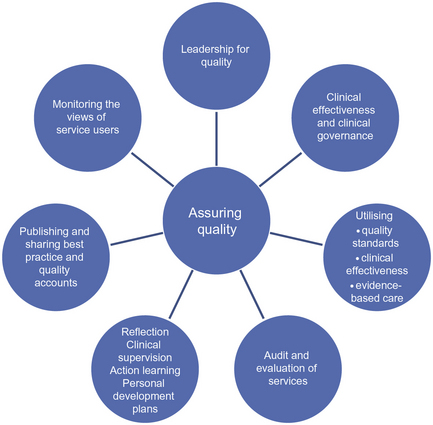
11 • To examine the concepts of clinical effectiveness and clinical governance • To examine a variety of different factors which can contribute to maintaining quality of care • To develop the student’s knowledge and understanding of the audit process • To explore how an understanding of clinical effectiveness can support the student’s achievement of specific Nursing and Midwifery Council Standards and Competencies Figure 11.1 demonstrates the wide range of issues that can contribute to achieving quality in health care. This chapter refers to each of these issues with specific reference to the community nursing role. The Department of Health’s publication, ‘High Quality Care for All’ (DH 2008a) emphasised the significance of quality in health care for all practitioners and stated that service provision should centre on three essentials of quality: In addition, the Healthcare Quality Strategy for NHS Scotland (Scottish Government 2010) focuses on similar ambitions for the quality of healthcare, namely, safe, effective and person-centred care. These strategic documents set the direction for achieving excellence in healthcare quality and drive forward initiatives at all levels of health and social care organisations. You will have come across a number of key phrases that are involved in the promotion and sustainability of quality in care, including reference to clinical effectiveness. Clinical interventions are deemed clinically effective when they do what they are intended and achieve the best possible outcomes for people within the resources that are available. Bowers and Cook (2012) refer to the importance of district nurses being able to demonstrate their effectiveness and role within the multidisciplinary team in supporting health outcomes for patients. Clinical effectiveness requires an analytical and questioning approach at all levels of the organisation and a willingness to make changes according to the evidence of what works best. Methods to promote clinical effectiveness include clinical audit and different strategies to develop and utilise skills, knowledge and experience of staff. The continual evaluation of practice is also an essential part of clinical effectiveness and includes gaining feedback from service users, carers and members of the clinical team. NHS Quality Improvement Scotland (NHS 2005; www.clinicalgovernance.scot.nhs.uk) describes clinical effectiveness as the right person (you) doing: • The right thing (evidence-based practice) • In the right way (skills and competence) • At the right time (providing treatment/services when the patient needs them) • In the right place (location of treatment/services) • With the right result (clinical effectiveness/maximising health gain). From the above activity, you will see that clinical effectiveness consists of a series of actions and changes which necessitates the management of change, the implementation of evidence-based care and the continuous monitoring and supervision of practice. The provision and promotion of quality services are an essential part of the healthcare practitioner’s role. As professionals, nurses are personally accountable for their actions and omissions and must adhere to the Nursing and Midwifery Council Code (NMC 2008b). Some characteristics of professional behaviour are essential to ensure quality, safety and effectiveness of care. These include a commitment to learning and updating of knowledge and skills; willingness to accept responsibility and to stand accountable for one’s own practice; respect; compassion and empathy for clients and colleagues; and being able to act in the best interest of service users and carers. As a student, you are personally accountable for the care you provide and this includes saying ‘No’ to something for which you feel unprepared or inexperienced. Access the Guidance on Professional Conduct for Nursing and Midwifery Students, at: www.nmc.org which outlines your professional responsibilities as a student nurse. The significance of regularly reflecting on practice in promoting quality of care is discussed later in this chapter. Quality can mean something different to different people, whether healthcare users or healthcare providers. The Institute of Medicine (2001) identified six dimensions of quality and these have been used widely in the UK to clarify the meaning and establish a shared understanding of quality in healthcare and are relevant to all practitioners. The Healthcare Quality Strategy for NHS Scotland (Scottish Government 2010) refers to the six dimensions, which are shown in Table 11.1. Table 11.1 The dimensions of quality in health care Person-centred care was referred to in Chapter 5 and was defined as the provision of care that is responsive to individual needs and values. There are a number of programmes which place people at the centre of care and support the development of relationships between them, their carers and healthcare providers. This results in shared decision-making, better experiences of care and greater job satisfaction for staff. The Department of Health (DH 2010a) referred to the importance of patient involvement in decisions about their health care; emphasis has also been placed on the facilitation of this with the provision of information to help patients make informed choices. The Care Quality Commission (CQC; www.cqc.org.uk) is a new independent regulator of all health and adult social care in England, which emphasises the importance of the patient’s perspective by listing a range of essential standards that clients should expect from health and adult social care services in England. This includes client expectation to: • be respected, involved in your care and support and told what’s happening at every stage • receive care, treatment and support that meets their needs • be cared for by staff with the right skills to do their job properly • know that the services you receive are continually monitored and checked for quality. Registration with the CQC provides assurance that essential levels of safety and quality are being met. An increasing number of healthcare providers are now registered with CQC in reference to healthcare associated infection. This requires that providers ensure clients and workers are protected against identifiable risks of acquiring a healthcare-associated infection. Service users can be reassured that quick action will be taken against those providers that fail to meet the requirements. (In Chapter 1, you will find reference to the organisations that perform this function in the other UK countries.) The Department of Health publication, ‘The Nursing Roadmap for Quality: a signposting map for nursing’ (DH 2010b) has demonstrated the nurse’s essential role and contribution to promoting and achieving quality. Seven elements to maintaining quality are identified within this publication: Clinical Quality Indicators (CQIs) are evidence-based process indicators that support practitioners to focus on quality, safety and reliability of care (NHS 2008b). The transforming community services (TCS) programme identified 43 indicators for quality improvement of community services in England (DH 2009). The programme supports: the development of services by setting out clear ambitions and the actions to achieve these; the development of people to design, deliver and lead change; the reform of systems to put in place the strong organisations and incentives that are needed to respond to the needs of people in their communities. The indicators cover many aspects of community services that interface with GPs, secondary care and social services and are very relevant to community nurses as part of the community multidisciplinary team. Their use is voluntary and, consequently, they are not used in all localities. (A link to the indicators for quality improvement is provided at the end of the chapter.)
Promoting clinical effectiveness and maintaining quality of care
Introduction
Policy drivers
Clinical effectiveness
Assuring quality
Quality in health care
1.
Person-centeredness: care which addresses the individual needs and values of the client
2.
Safety: care which is safe and avoids injury to the patient
3.
Effectiveness: care which is based on scientific evidence
4.
Efficiency: care which avoids waste and utilises resources appropriately
5.
Equitable: all care is available to all clients and patients whoever and wherever they are
6.
Timely: care is delivered when it is required whenever that may be without undue delay.
Person-centred care, involving patients and the views of service users
The role of the community nurse in promoting quality
Clinical guidelines
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Nurse Key
Fastest Nurse Insight Engine
Get Clinical Tree app for offline access