Chapter 20 Prolonged Pregnancy and Disorders of Uterine Action
Post-term or prolonged pregnancy
Risks and clinical implications of post-term pregnancy
 Post-term pregnancy is one that is in excess of 287 days (although 42 weeks is often considered acceptable).
Post-term pregnancy is one that is in excess of 287 days (although 42 weeks is often considered acceptable).
 Accurate dating of a pregnancy is essential, as incorrect diagnosis that a pregnancy has gone beyond term may lead to inappropriate or unnecessary intervention.
Accurate dating of a pregnancy is essential, as incorrect diagnosis that a pregnancy has gone beyond term may lead to inappropriate or unnecessary intervention.
 Post-term pregnancy is associated with an increase in perinatal mortality and neonatal morbidity rates.
Post-term pregnancy is associated with an increase in perinatal mortality and neonatal morbidity rates.
 Possible fetal consequences include macrosomia or fetal compromise due to placental demise.
Possible fetal consequences include macrosomia or fetal compromise due to placental demise.
 Prolonged pregnancy is the largest single indication for induction of labour.
Prolonged pregnancy is the largest single indication for induction of labour.
Antenatal surveillance
 Biophysical profile. A combined ultrasound assessment of fetal breathing, fetal movement, fetal tone, reactivity of the heart rate and amniotic fluid volume is used to predict fetal wellbeing in a high-risk pregnancy. A total score of 8–10 indicates the fetus is in good condition.
Biophysical profile. A combined ultrasound assessment of fetal breathing, fetal movement, fetal tone, reactivity of the heart rate and amniotic fluid volume is used to predict fetal wellbeing in a high-risk pregnancy. A total score of 8–10 indicates the fetus is in good condition.
 Doppler ultrasound of umbilical artery.
Doppler ultrasound of umbilical artery.
 Twice weekly cardiotocography (CTG), also known as non-stress testing (NST).
Twice weekly cardiotocography (CTG), also known as non-stress testing (NST).
Induction of labour
Indications for induction
Induction is indicated when the benefits to the mother or the fetus outweigh those of continuing the pregnancy. It is associated with the maternal and fetal factors described in Box 20.1.
Box 20.1 Indications for induction of labour
Maternal
Methods of inducing labour
Prostaglandins and induction
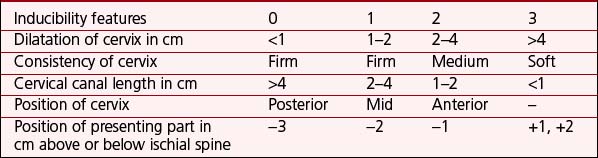
Prior to prescribing prostaglandin, the cervix is assessed using the Bishop’s score (Table 20.1). PGE2 preparations are available in gels, tablets or controlled-release pessary form; they are inserted close to the cervix within the posterior fornix of the vagina. Fetal heart rate and uterine contractions should be monitored continuously for 30–60 minutes thereafter. The mother remains recumbent or resting for 1 hour. Changes in the cervix can be assessed by an increase in the Bishop’s score.
Recommended prescribed doses of PGE2 are shown in Table 20.2.
Table 20.2 Recommended prescribed doses of prostaglandin E2
| Form | Dose |
|---|---|
| Slow-release pessary | One dose (10 mg of dinoprostone), string left accessible, removed after 24 hours |
| Tablets | 3 mg 6–8 hourly, maximum dose 6 mg |
| Gels | Nulliparous women with an unfavourable cervix: 2 mg (maximum 4 mg) |
| All other women: 1 mg (maximum 3 mg) | |
| Repeat doses of 1–2 mg 6 hourly may be given |
Amniotomy
ARM is carried out using an amnihook or an amnicot. Procedures are shown in Box 20.2.
Box 20.2 Amniotomy procedures
Prior to intervention
Oxytocin
Administration of oxytocin to induce labour
 Oxytocin is used intravenously, diluted in an isotonic solution such as normal saline.
Oxytocin is used intravenously, diluted in an isotonic solution such as normal saline.
 The infusion should be controlled through a pump to enable accurate assessment of volume and rate.
The infusion should be controlled through a pump to enable accurate assessment of volume and rate.
 Dosage should be recorded in milliunits per minute, with the suggested dilution being 30 IU in 500 ml of normal saline. (Note: 1 ml per hour delivers 1 milliunit per minute.) The midwife should aim to administer the lowest dose required to maintain effective, well-spaced uterine contractions, with a maximum of 3–4 contractions every 10 minutes (Table 20.3).
Dosage should be recorded in milliunits per minute, with the suggested dilution being 30 IU in 500 ml of normal saline. (Note: 1 ml per hour delivers 1 milliunit per minute.) The midwife should aim to administer the lowest dose required to maintain effective, well-spaced uterine contractions, with a maximum of 3–4 contractions every 10 minutes (Table 20.3).
 Oxytocin should not be started within 6 hours of the administration of prostaglandins.
Oxytocin should not be started within 6 hours of the administration of prostaglandins.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree