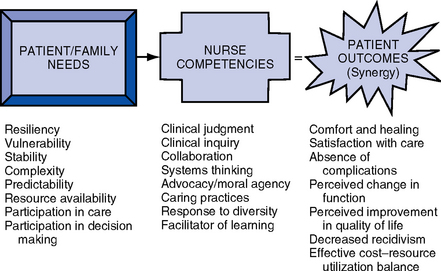
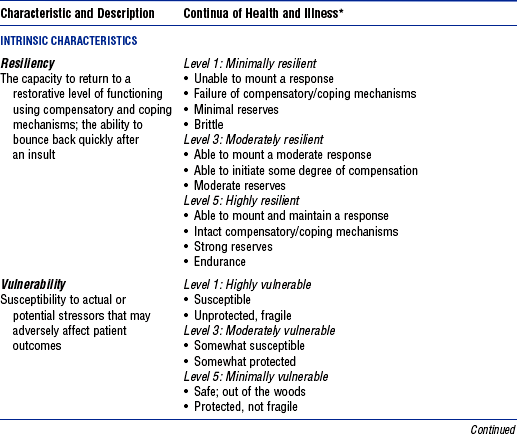
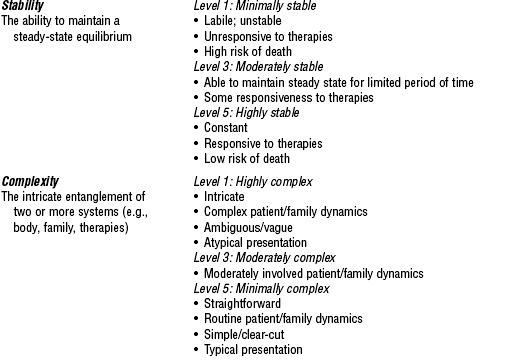
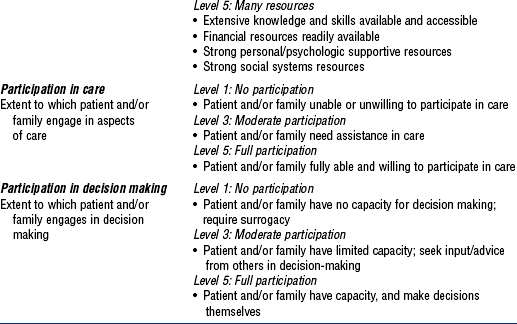
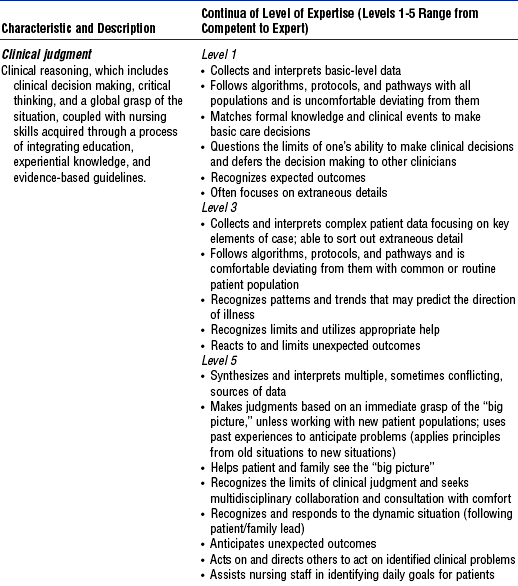
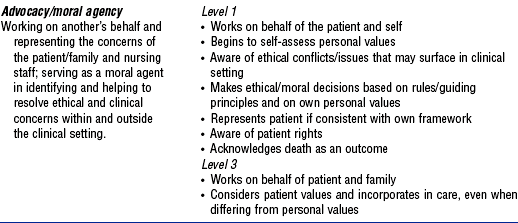
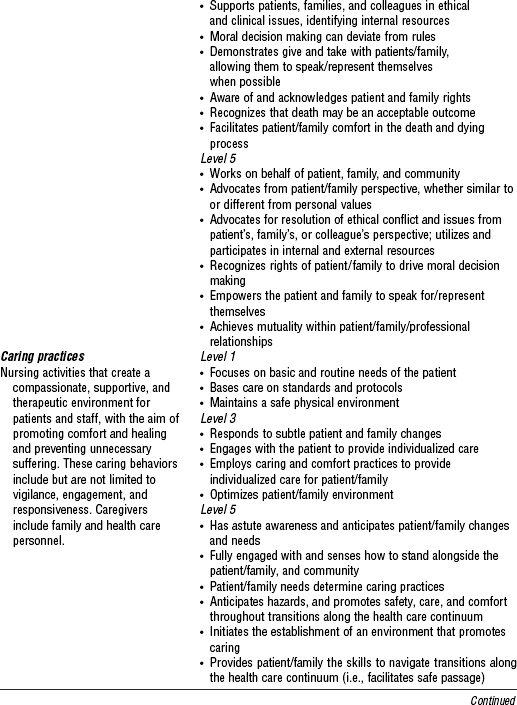
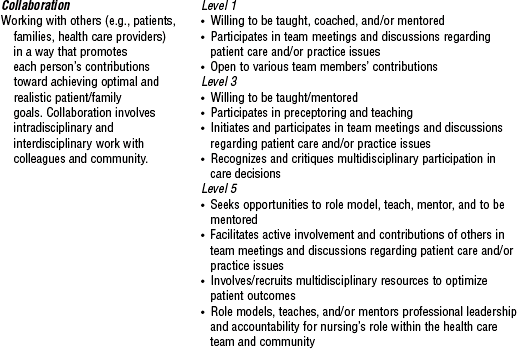
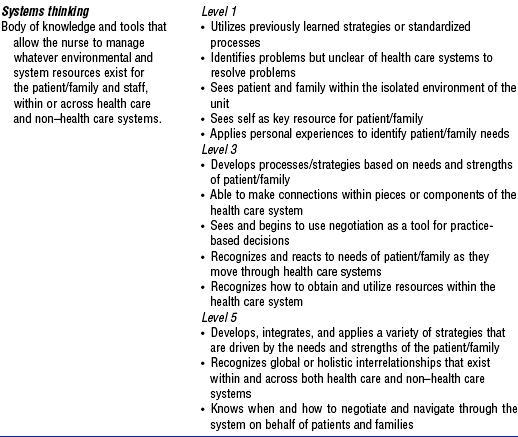
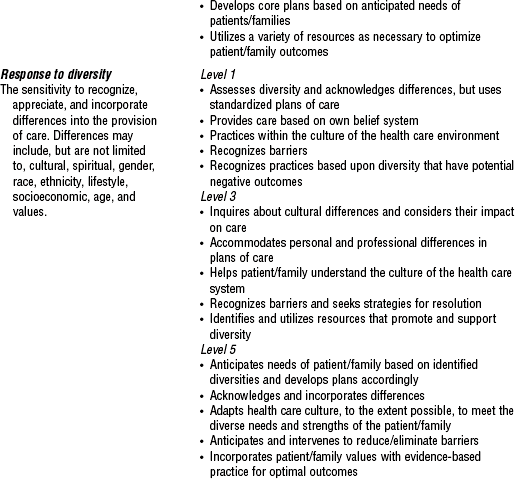
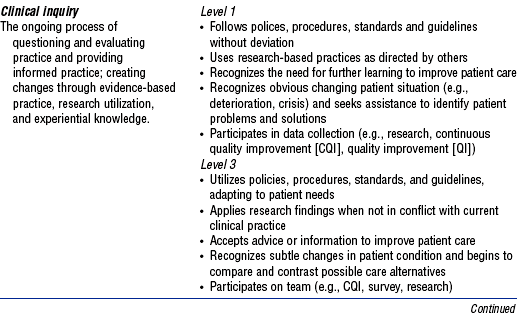
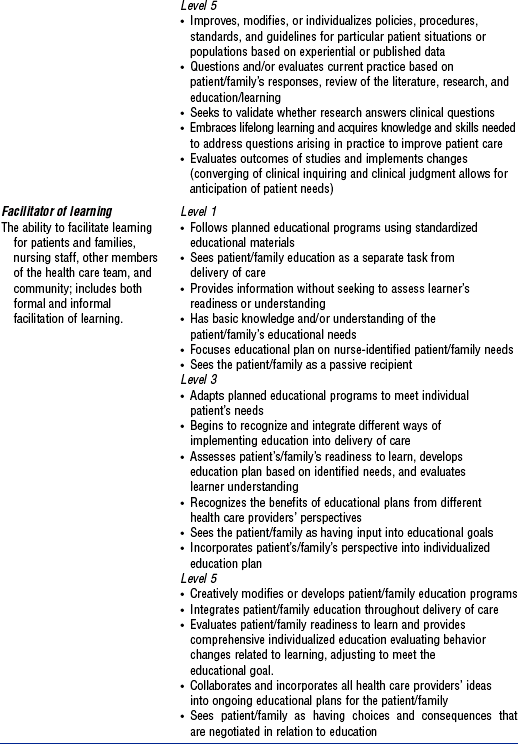
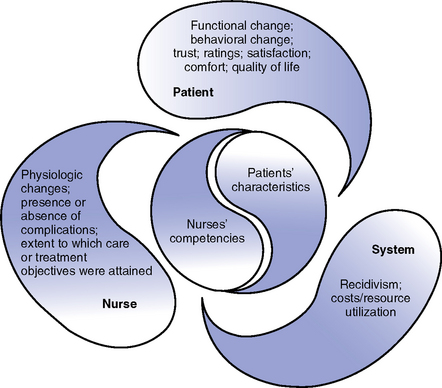
CHAPTER 1 1. Be accountable to uphold and consistently act in concert with ethical values and principles 2. Advocate for organizational decisions that are driven by the needs of patients and their families 3. Act with integrity by communicating openly and honestly, keeping promises, honoring commitments, and promoting loyalty in all relationships 4. Collaborate with all essential stakeholders by creating synergistic relationships to promote common interest and shared values 5. Provide leadership to transform thinking, structures, and processes to address opportunities and challenges 6. Demonstrate stewardship through fair and responsible management of resources 7. Embrace lifelong learning, inquiry, and critical thinking to enable each to make optimal contributions 8. Commit to quality and excellence at all levels of the organization, meeting and exceeding standards and expectations 9. Promote innovation through creativity and calculated risk taking 10. Generate commitment to and passion for the organization’s causes and work What Nurses Do (American Nurses Association [ANA], 2003) 1. Attend to the full range of human experiences of and responses to health and illness 2. Integrate objective data with knowledge of the patient as a person and understanding of the patient’s subjective experience 3. Apply scientific knowledge to the process of diagnosis and treatment of the responses to health and illness 1. Critical care nurses deal with human responses to life-threatening problems 2. The Scope of Practice includes all ages and involves a dynamic interaction between the critically ill patient, the patient’s family, the critical care nurse, and the environment 3. The framework of practice includes the scientific body of specialized knowledge, an ethical model for decision making, a commitment to interdisciplinary collaboration, and the AACN Synergy Model for Patient Care. Critical care nurses rely on this framework to do the following (Bell, 2002, p. 44): a. Support and maintain the physiologic stability of patients b. Assimilate and prioritize information sources to take immediate and decisive patient-focused action c. Respond with confidence and adapt to rapidly changing patient conditions d. Respond to the unique needs of patients and families coping with unanticipated treatment, quality of life, and end-of-life decisions e. Manage appropriately the interface between the patient and technology that may be threatening, invasive, and complex so that human needs for a safe, respectful, healing, humane, and caring environment are established and maintained f. Monitor and allocate critical care services, recognizing the fiduciary role of nurses working in a resource-intensive environment 1. Complexity requiring vigilance: Critically ill patients require complex assessment and therapies, high-intensity interventions, and continuous vigilance 2. Organizational model for a humane, caring, and healing environment a. The critical care nurse works with an interdisciplinary team to create a humane, caring, and healing environment. There are five elements of an organizational model for health and healing (Malloch, 2000; Molter, 2003): i. Common values of health as a function of mind-body-spirit interrelationships ii. Patient and family–centered philosophy iii. Physical environment that supports healing iv. Use of complementary and alternative therapies as well as conventional therapies b. The critical care nurse is a constant in the environment and works to develop an organizational culture that supports the following (Bell, 2002, p. 45): i. Providers that act as advocates on behalf of patients, families, and communities ii. The dominance of the patient’s and family’s values iii. Practice based in research and driven by outcomes vi. The fostering of leadership at all levels and in all activities vii. Lifelong learning as fundamental to professional growth viii. Optimization of existing talents and resources ix. The rewarding of innovation and creativity a. An Institute of Medicine (IOM) study notes the occurrence of a significant number of deaths related to health care service delivery processes (IOM, 1999) b. The Joint Commission on Accreditation of Healthcare Organizations (JCAHO) established National Patient Safety Goals in 2005 (JCAHO, 2006). The goals include the following*: i. Improve the accuracy of patient identification by using at least two patient identifiers when administering medications or blood products, taking blood samples and other specimens for clinical testing, or providing any other treatments or procedures. ii. Improve the effectiveness of communication among caregivers by reading back verbal or telephone orders and critical laboratory results; standardizing abbreviations, acronyms, and symbols not to be used in the organization; improving the timeliness of receiving critical test results and values; and standardizing the “hand off” of communications. iii. Improve the safety of using medications by standardizing and limiting the number of drug concentrations available in the organization, identifying and reviewing a list of look-alike/sound-alike drugs, taking action to prevent errors involving the interchange of these drugs, and labeling all medications, medication containers, or other solutions in perioperative and other procedural settings. iv. Reduce the risk of health care–associated infections by complying with current Centers for Disease Control and Prevention hand hygiene guidelines and managing as sentinel events all identified cases of unanticipated death or major permanent loss of function associated with a health care–associated infection. v. Accurately and completely reconcile medications across the continuum of care by implementing a process to obtain and document a complete list of the patient’s current medications upon the patient’s admission to the organization, by comparing the medications on the list to those available in the organization and by communicating the list to the next provider of service when a patient is referred or transferred. vi. Reduce the risk of patient harm resulting from falls by implementing a fall-reduction program and evaluating its effectiveness. 1. Synergistic practice and patient and family safety: The AACN Synergy Model for Patient Care (Curley, 1998) describes nursing practice in terms of the needs and characteristics of patients. The model’s premise is that the needs of the patient and family system drive the competencies required by the nurse. When this occurs, synergy is produced and optimal outcomes can be achieved. Buckminster Fuller stated that “synergy is the only word in our language that means behavior of whole systems unpredicted by the separately observed behaviors of any of the system’s separate parts or any subassembly of the system’s parts” (cited in Carlson, 1996, p. 92). The synergy created by practice based on the Synergy Model helps the patient-family unit safely navigate the health care system. 2. The Synergy Model and ethical practice: The Synergy Model provides a foundation for addressing ethical concerns related to critical care nursing practice (McGaffic, 2001). The model focuses on the characteristics of patients, the competencies needed by the critical care nurse to meet the patient’s needs based on these characteristics, and the outcomes that can be achieved through the synergy that develops when nursing competencies are driven by the patient’s needs. AACN is committed to helping members deal with ethical issues through education (Glassford, 1999). In 1992, AACN developed a vision of a health care system driven by the needs of patients and their families in which critical care nurses can make their optimal contribution. AACN Certification Corporation in tandem was rethinking the contributions of certification to the care of patients. Patient needs and outcomes must be the central focus of certification. A think tank was convened in 1992 to reconceptualize certified practice (Caterinicchio, 1995; Villaire, 1996). Prior to development of the Synergy Model, the certification process conceptualized nursing practice according to the dimensions of the nurse’s role, the clinical setting, and the patient’s diagnosis. The Synergy Model reconceptualized certified practice to recognize that the needs and characteristics of patients and families influence and drive the competencies of nurses. The synergy that develops when this occurs influences the outcomes of individual patients, the nurse’s practice, and the organization. A separate think tank in 1996 identified the potential outcomes (Biel, 1997). 1. Description of the Synergy Model (Figure 1-1): The synergy that occurs when patient and family characteristics or needs drive the competencies that nurses need to achieve optimal outcomes for the patient, nurse, and organization 2. Assumptions of the Synergy Model (AACN Certification Corporation, 1998) a. All patients are biologic, psychologic, social, and spiritual entities who have similar needs and experiences at a particular developmental stage across wide ranges or continua from health to illness. The whole patient must be considered. More compromised patients have more complex needs. b. The dimensions of a nurse’s practice as determined by the needs of a patient and family can also be described along continua c. The patient, family, and community all contribute to providing a context for the nurse-patient relationship d. Optimal outcomes can be achieved through the synergy effected by alignment of nurse competencies with patient and family needs. A peaceful death can be an acceptable outcome. 3. Patient characteristics: Characteristics unique to each patient and family span the continua of health and illness. The first five are intrinsic to the patient and the last three are extrinsic. Each characteristic is described in terms of a range of levels from 1 to 5 in Table 1-1 (AACN Certification Corporation, 1997, 2004). TABLE 1-1 The Synergy Model—Patient Characteristics From AACN Certification Corporation. *Note that the continua of health and illness levels vary in order of rating based on the characteristic. a. Resiliency: The capacity to return to a restorative level of functioning using compensatory and coping mechanisms; the ability to bounce back quickly after an insult b. Vulnerability: Susceptibility to actual or potential stressors that may adversely affect patient outcomes c. Stability: The ability to maintain a steady-state equilibrium d. Complexity: The intricate entanglement of two or more systems (e.g., body, family, therapies) e. Predictability: A characteristic that allows one to expect a certain course of events or course of illness f. Resource availability: Extent of resources (e.g., technical, fiscal, personal, psychologic, and social) the patient, family, and community bring to the situation g. Participation in care: Extent to which the patient and/or family engages in aspects of care h. Participation in decision making: Extent to which the patient and/or family engages in decision making 4. Nurse characteristics: Nursing care is an integration of knowledge, skills, experience, and individual attitudes. The continua of nurse characteristics needed are derived from the patient’s needs and range from a competent to expert level as outlined in Table 1-2. TABLE 1-2 The Synergy Model—Nurse Characteristics From AACN Certification Corporation and PES: Final report of a comprehensive study of critical care nursing practice. Aliso Viejo, Calif, 2004, The Corporation. a. Clinical judgment: Clinical reasoning, which includes clinical decision making, critical thinking, and a global grasp of the situation, coupled with nursing skills acquired through a process of integrating education, experiential knowledge, and evidence-based guidelines b. Advocacy/moral agency: Working on another’s behalf and representing the concerns of the patient/family, and nursing staff; serving as a moral agent in identifying and helping to resolve ethical and clinical concerns within and outside the clinical setting c. Caring practices: Nursing activities that create a compassionate, supportive, and therapeutic environment for patients and staff, with the aim of promoting comfort and healing and preventing unnecessary suffering. These caring behaviors include but are not limited to vigilance, engagement, and responsiveness. Caregivers include family and health care personnel. d. Collaboration: Working with others (e.g., patients and families, health care providers) in a way that promotes each person’s contributions toward achieving optimal and realistic patient and family goals. Collaboration involves intradisciplinary and interdisciplinary work with colleagues and community. e. Systems thinking: The body of knowledge and tools that allow the nurse to manage whatever environmental and system resources exist for the patient, family, and staff within or across health care and non–health care systems f. Response to diversity: The sensitivity to recognize, appreciate, and incorporate differences into the provision of care. Differences may include, but are not limited to, cultural, spiritual, gender, race, ethnicity, lifestyle, socioeconomic, age, and values. g. Clinical inquiry or innovation and evaluation: The ongoing process of questioning and evaluating practice and providing informed practice; creating changes through evidence-based practice, research utilization, and experiential knowledge h. Facilitator of learning: The ability to facilitate learning for patients and families, nursing staff, other members of the health care team, and community; includes both formal and informal facilitation of learning 5. Outcomes of patient-nurse synergy (Figure 1-2) (Curley, 1998) (From Curley M: Patient-nurse synergy: optimizing patients’ outcomes, Am J Crit Care 7:69, 1998.) i. Behavior change: Based on the dispensing and receiving of information. Requires caregiver trust. Patients and families grow in their knowledge about health and take greater responsibility for their own health. (a) Functional change and quality of life: Multidisciplinary measures that can be used across all populations of patients but provide specific information to a population of patients when analyzed separately (b) Satisfaction ratings: Subjective measures of individual health and quality of health services. Satisfaction measures query about expectations (technical care provided, trusting relationships, and education experiences) and the extent to which they are met. Often linked with functional change and quality-of-life perceptions. (c) Comfort ratings and perceptions: Quality-of-care outcomes based on caring practices with the aim of promoting comfort and alleviating suffering i. Physiologic changes: Require monitoring and managing instantaneous therapies and noting changes. The nurse expects a specific trajectory of changes when he or she “knows” the patient (Tanner, Benner, and Chesla, 1993). ii. The presence or absence of preventable complications: Through vigilance and clinical judgment, the nurse creates a safe and healing environment iii. Extent to which care and treatment objectives were attained: Reflects the nurse’s role as an integrator of care that requires a high degree of collaboration i. Recidivism: Decrease in rehospitalization or readmission, which adds to the personal and financial burden of care ii. Cost and resource utilization: Organizations usually evaluate financial cost based on an episode of care. Achieving cost-effective care requires knowing the patient and providing continuity of care. Resource utilization can affect patient outcomes when there is not enough care given by competent nurses (Aiken et al, 2001). When nurses cannot provide care at an appropriate level to meet patient needs, they are dissatisfied and turnover is high, which results in increased costs for the organization (Cornerstone Communication Group, 2001). 1. National validation study methodology a. Synergy Model originally validated in large-scale national study of practice (Muenzen and Greenberg, 1998) b. Survey methodology used to determine predicted relationships among patient-family and nurse characteristics and their interactions in the Synergy Model c. Surveys sent to 3924 nurses (adult, pediatric, and neonatal nurses in subacute, acute, and critical care settings); response rate of 24% a. Respondents accurately perceived acuity of patients’ conditions in the profiles developed for the study b. Respondents perceived that the critically ill patients described in the patient profiles required care by nurses with higher levels of the nurse characteristics listed in Table 1-2 than did the less acutely ill patients described in the profiles; respondents perceived that “clinical judgment” was most strongly related to patient need and that the nurse requires a higher level of this characteristic to achieve optimal outcomes c. The eight patient characteristics and their associated rating scales were useful in differentiating acuity levels d. Acuity-of-care levels were not differentiated based on the patient’s and family’s ability to participate in decision making and care, and the patient’s and family’s level of technical, fiscal, personal and psychologic, and social resources e. Patients whose care requires critical care skills are not found solely in critical care units. They may be located in progressive care units, postanesthesia units, rehabilitation facilities, and the home environment. f. The eight patient characteristics fall into two groups: Intrinsic (resiliency, vulnerability, stability, complexity, and predictability) and extrinsic (participation in decision making, participation in care, and resource availability) g. The eight nurse characteristics are all intercorrelated and may reflect overall nurse competency There are many applications for the model in clinical operations, clinical practice, education, and research* a. Leadership: Using the model for organizational infrastructure for achieving excellence in practice, improving financial outcomes, and establishing clinical advancement programs (Cohen et al, 2002; Czerwinski, Blastic, and Rice, 1999; Doble et al, 2000; Kerfoot, 2001) b. Development of continuity-of-care models (Ecklund, 2002; Edwards, 1999) c. Foundation model for family-centered care practice (Collopy, 1999; Henneman and Cardin, 2002; Stannard, 1999) d. Basis for making care assignments and making nursing rounds (Hartigan, 2000; Mullen, 2002) a. Development of clinical strategies (Markey, 2001) b. Direct patient care (Annis, 2002; Hardin and Hussey, 2003) a. Curricula design: Serves as the basis for the graduate nursing program curriculum at Duquesne University† b. Basis for CCRN (critical care nurse) and CCNS (critical care clinical nurse specialist) certification examinations since 1999 (Moloney-Harmon, 1999) c. Potential use as a foundation for education of health care teams (Molter, 1997) a. Validated in the AACN Certification Corporation Study of Practice (1998, 2004) b. Underwent theoretical review (Sechrist, Berlin, and Biel, 2000) c. Further research needed related to consumer perspective, staffing and productivity implications for nursing, patient outcomes measurement, and development of a quantitative tool based on the model for rapidly assessing patients and determining nursing characteristics needed Provides guidance for acceptable nursing roles and practices, which vary from state to state 1. Nurses are expected to follow the nurse practice act and not deviate from usual nursing activities 2. Advanced nursing practice: Expanded roles for nurses include nurse practitioner, clinical nurse specialist, certified registered nurse anesthetist, and certified nurse-midwife. These roles require education beyond the basic nurse education and usually involve a master’s degree. Certain responsibilities associated with these roles are not interchangeable (ANA, 1997) 3. A scope of practice and standards for the acute care nurse practitioner was developed by AACN and the ANA 4. A scope of practice and standards for the acute care clinical nurse specialist based on the Synergy Model was published by AACN (Bell, 2002) 1. A standard of care is any established measure of extent, quality, quantity, or value; an agreed-upon level of performance or a degree of excellence of care that is established 2. Standards are established by usual and customary practice, institutional guidelines, association guidelines, and legal precedent 3. Standards of care, standards of practice, policies, procedures, and performance criteria all establish an agreed-upon level of performance or degree of excellence a. AACN standards for acute and critical care nursing practice (Medina, 2000) d. ANA standards: The ANA has generic standards and also specialty standards (e.g., for medical-surgical nursing) c. Standards of clinical practice for acute care certified nurse practitioners d. AACN Scope of Practice and Standards of Professional Performance for the Acute and Critical Care Clinical Nurse Specialist (Bell, 2002) 4. National facility standards: Include those published by JCAHO and the National Committee for Quality Assurance* 5. Community and regional standards: Standards prevalent in certain areas of the country or in specific communities 6. Hospital and medical center standards: Standards developed by institutions for their staff and patients 7. Unit practice standards, policies, and protocols: Specific standards of care for specific groups or types of patients or specific procedures (e.g., insulin or massive blood transfusion protocols) 8. Precedent court cases: Standard of a “reasonable, prudent nurse” (i.e., what a reasonable, prudent nurse would have done in the given situation) 9. Other nursing and interdisciplinary specialty organization standards (such as those of the American Heart Association, the Society of Critical Care Medicine, the Association of periOperative Registered Nurses) 1. Certification is a process by which a nongovernmental agency, using predetermined standards, validates an individual nurse’s qualification and knowledge for practice in a defined functional or clinical area of nursing 2. A common goal of specialty certification programs is to promote consumer protection and to promote high standards of practice 3. The certified nurse may be held to a higher standard of practice in the specialty than the noncertified nurse; certification validates the nurse’s knowledge and experience in a specialty area 4. Critical care certifications are awarded by AACN Certification Corporation, established in 1975. AACN Certification Corporation is accredited by the National Commission for Certifying Agencies, the accreditation arm of the National Organization for Competency Assurance 1. Professional negligence: An unintentional act or omission; the failure to do what the reasonable, prudent nurse would do under similar circumstances, or an act or failure to act that leads to an injury of another. Six specific elements are necessary for professional negligence action and must be established by a person bringing a suit against a nurse (plaintiff) (Giordano, 2003; Guido, 1997): a. Duty: To protect the patient from an unreasonable risk of harm b. Breach of duty: Failure by a nurse to do what a reasonable, prudent nurse would do under the same or similar circumstances. The breach of duty is a failure to perform within the given standard of care. The standard defines the nurse’s duty to the patient. c. Proximate cause: Proof that the harm caused was foreseeable and that the person injured was foreseeably a victim. This element can determine the extent of damages for which a nurse may be held liable. e. Direct cause of injury: Proof that the nurse’s conduct was the cause of or contributed to the injury to the patient f. Damages: Proof of actual loss, damage, pain, or suffering caused by the nurse’s conduct 2. Malpractice: A specific type of negligence that takes account of the status of the caregiver as well as the standard of care (Giordano, 2003; Guido, 1997). Professional negligence is malpractice. It is differentiated from ordinary negligence (e.g., failure to clean up water from the floor). a. Professional misconduct, improper discharge of professional duties, or a failure by a professional to meet the standard of care that results in harm to another person b. Malpractice is the failure of a professional person to act in accordance with prevailing professional standards or a failure to foresee consequences that a professional person who has the necessary skills and education would foresee c. Most common types of malpractice or negligence in critical care settings include medication errors, failure to prevent patient falls, failure to assess changes in clinical status, and failure to notify the primary provider of changes in patient status a. Definitions (National Council of State Boards of Nursing, 1995) i. Delegation: Transferring to a competent individual the authority to perform a selected nursing task in a selected situation; the nurse retains accountability for the delegation ii. Accountability: Being responsible and answerable for actions or inactions of self or others in the context of delegation iii. Authority: Deemed present when a registered nurse (RN) has been given the right to delegate based on the state nurse practice act and also has the official power from an agency to delegate iv. Unlicensed assistive personnel (UAP): Any unlicensed personnel, regardless of title, to whom nursing tasks are delegated v. Delegator: The person making the delegation vi. Delegatee: The person receiving the delegation vii. Competent: Demonstrating the knowledge and skill, through education and experience, to perform the delegated task b. The five “rights” of delegation i. Right task: The RN ensures that the task to be delegated is appropriate to be delegated for that specific patient. Example: Delegating suctioning of a tracheostomy in a stable patient to a licensed practical nurse is appropriate. If the patient is a head injury patient who becomes bradycardic and hypotensive during suctioning, then delegation of this task for this patient may not be appropriate. ii. Right circumstances: The RN ensures that the setting is appropriate and that resources are available for successful completion of the delegated task iii. Right person: The RN delegates the right task to the right person to be performed on the right person iv. Right direction and communication: The delegating nurse provides a clear explanation of the task and expected outcomes; the RN sets limits and expectations for performance of the task v. Right supervision: The RN does appropriate monitoring and evaluation, and intervenes as needed; the RN provides feedback to the delegatee and establishes parameters for receiving feedback about the outcome of the task c. Model of the delegation decision-making process: The nurse must ensure that delegation of nursing tasks is based on appropriate assessment, planning, implementation, and evaluation. Box 1-1 describes the model for delegation established by the National Council of State Boards of Nursing. d. Nurse executives must ensure the following: i. Policies and procedures concerning supervision and delegation are in place and are consistent with state nurse practice acts ii. Job descriptions for UAPs do not include responsibilities for whose performance a license is required iii. Adequate training and consistent orientation for UAPs are provided e. In the complex critical care environment, many of the concepts for delegation to UAPs can also be applied to delegation of care to other professional nurses and licensed practical or vocational nurses (through assignments made by charge nurses or nurse managers) i. The job descriptions and scope of practice for personnel with various levels of expertise and for various roles must be clearly defined ii. When assignments are made, the patient’s characteristics (as defined by the Synergy Model) and required care procedures guide the decision regarding the competency level of the nurse who should provide the care iii. Nurse executives and nurse managers must ensure that nurses have demonstrated and documented levels of expertise necessary to provide the care required by specific patients iv. Additional training and experience are required for performance of many of the complex therapies needed by vulnerable critically ill patients a. Staffing is a process and an outcome. The term can refer to the process by which human resources are used within a nursing care unit or to the number of staff members required to provide care. The individuals managing health care services have ethical responsibilities to ensure that policies and processes are in place to ensure the safety of the patients and the staff (Box 1-2) (Curtin, 2002a, 2002b). b. The optimal use of RN time and expertise depends on a number of variables: allocating acute and critical care beds based on patient need; ensuring availability of adequate numbers of qualified, competent nursing and support staff; establishing sufficient support systems; following and adhering to legal and regulatory requirements; and evaluating services through outcome and quality measures c. Patient and family–focused care requires matching the right caregiver to each patient, identifying systems that provided the right support in delivering care, incorporating legal and regulatory considerations, and measuring the outcomes of care d. AACN (2000) recommendations for staffing policy include the following: i. Develop a comprehensive strategic plan that links patient and family needs, cost of delivery, competency of providers, and staff mix with patient outcomes. Such a plan is required by the JCAHO standards. The plan must be flexible to adjust staffing to the unpredictability of increasing patient acuity in the critical care setting. It is difficult to state a single national staffing ratio or mix because staffing must be adjusted to meet the needs of a specific group of patients at a given time. ii. The foundation for minimum staffing levels is clearly articulated in standards for acute and critical care nursing practice that prescribe a competent level of nursing practice, as well as in standards of professional performance that articulate the roles and behaviors of nursing professionals
Professional Caring and Ethical Practice
AMERICAN ASSOCIATION OF CRITICAL-CARE NURSES (AACN) VISION, MISSION, AND VALUES (AACN, 2002)
Values
SYNERGY OF CARING
What Critical Care Nurses Do (Medina, 2000)
The Environment of Critical Care
The “Synergy” of the AACN Synergy Model for Patient Care
AACN SYNERGY MODEL FOR PATIENT CARE
Purpose
Overview of the Synergy Model (AACN Certification Corporation, 2003, 2004)
Validation
Application of the Synergy Model
GENERAL LEGAL CONSIDERATIONS RELEVANT TO CRITICAL CARE NURSING PRACTICE
Scope of Practice
Standards of Care
Certification in a Specialty Area
Professional Liability
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree