Chapter 12 Problems of Pregnancy
Abdominal pain in pregnancy
 the physiologically normal (e.g. mild indigestion or muscle stretching)
the physiologically normal (e.g. mild indigestion or muscle stretching)
 the pathological but not dangerous (e.g. degeneration of a fibroid)
the pathological but not dangerous (e.g. degeneration of a fibroid)
 the dangerously pathological requiring immediate referral to the appropriate medical practitioner for urgent treatment (e.g. ectopic pregnancy or appendicitis).
the dangerously pathological requiring immediate referral to the appropriate medical practitioner for urgent treatment (e.g. ectopic pregnancy or appendicitis).
The midwife should take a detailed history and perform a physical examination in order to reach a decision about whether to refer the woman. Treatment will depend on the cause (Box 12.1) and the maternal and fetal conditions.
Box 12.1 Causes of abdominal pain in pregnancy
Severe uterine torsion
Management
Symphysis pubis dysfunction (Pelvic girdle pain [PGP])
Management
 Reduce non-essential weight-bearing activities and avoid straddle movements that abduct the hips, e.g. squatting.
Reduce non-essential weight-bearing activities and avoid straddle movements that abduct the hips, e.g. squatting.
 A supportive panty girdle or ‘tubigrip’ and comfortable shoes may help when the woman is up and about.
A supportive panty girdle or ‘tubigrip’ and comfortable shoes may help when the woman is up and about.
 Refer to an obstetric physiotherapist for advice and treatment.
Refer to an obstetric physiotherapist for advice and treatment.
 In severe cases, bed rest on a firm mattress may be necessary.
In severe cases, bed rest on a firm mattress may be necessary.
 Postnatal physiotherapy will aid the strengthening and stabilisation of the joint.
Postnatal physiotherapy will aid the strengthening and stabilisation of the joint.
Antepartum haemorrhage (APH)
Types of APH (Table 12.1)
 Bleeding from local lesions of the genital tract (incidental causes).
Bleeding from local lesions of the genital tract (incidental causes).
 Placental separation due to placenta praevia or placental abruption.
Placental separation due to placenta praevia or placental abruption.
Table 12.1 Causes of bleeding in late pregnancy
| Cause | Incidence (%) |
|---|---|
| Placenta praevia | 31.0 |
| Placental abruption | 22.0 |
| ‘Unclassified bleeding’, e.g.: | 47.0 |
| Marginal | |
| Show | |
| Cervicitis | |
| Trauma | |
| Vulvovaginal varicosities | |
| Genital tumours | |
| Genital infections | |
| Haematuria | |
| Vasa praevia | |
| Other |
Initial appraisal of a woman with APH
Assessment of physical condition
Maternal condition
 Take a history from the woman.
Take a history from the woman.
 Observe pulse rate, respiratory rate, blood pressure and temperature.
Observe pulse rate, respiratory rate, blood pressure and temperature.
 Look for any pallor or breathlessness.
Look for any pallor or breathlessness.
 Assess the amount of blood lost.
Assess the amount of blood lost.
 Perform a gentle abdominal examination, observing for signs that the woman is going into labour.
Perform a gentle abdominal examination, observing for signs that the woman is going into labour.
 On no account must any vaginal or rectal examination be done; nor may an enema or suppository be given to a woman suffering from an APH.
On no account must any vaginal or rectal examination be done; nor may an enema or suppository be given to a woman suffering from an APH.
Factors to aid differential diagnosis
The location of the placenta is perhaps the most critical piece of information that will be needed in order to make a correct diagnosis; initially, the midwife may not have this fact at her disposal. However, if she is able to elicit the information listed in Box 12.2 from her observations and from talking to the woman and her partner, then this will help her to arrive at a provisional diagnosis.
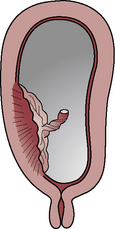
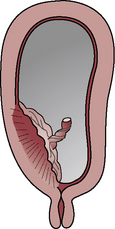
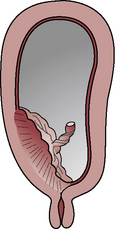
Placenta praevia
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree