Principles of phlebotomy and intravenous therapy
Intravenous cannulation
Learning outcomes
Having read this chapter, the reader should be able to:
When consistent or repeated intravascular access is needed, a cannula is inserted and secured. Some cannulas, e.g. central venous access, are beyond the scope of this text, but fairly commonly midwives insert and care for peripheral cannulae. The terminology changes; the term ‘vascular access device’ (VAD) can refer to a number of different devices (Dougherty 2011). In this book the term ‘peripheral intravenous cannula’ (PIC) will be used to describe the intravascular device placed in the hand or lower arm (generally) for the purposes of administering intravenous fluid(s), medication or blood/blood products.
Performing the skill requires training, supervised practice, and ongoing maintenance of the skill. Depending on local protocol, cannula insertion is often undertaken only by qualified staff. PICs feature highly in the nursing and midwifery literature partly because of the risks of localized and systemic infection from their incorrect insertion, use or removal. Insertion, removal and ongoing care of the PIC are all considered within this chapter. The midwife’s role and responsibilities are also considered.
Considerations for the childbearing woman
The additional blood volume in pregnancy and higher body temperature usually mean that the veins are prominent and are therefore easier to gain access to. PICs should be inserted only when there is a clinical indication, and should be removed as soon as that aspect of care is completed. Complications such as infection or occlusion make the therapy more difficult to administer, increase patient discomfort, increase length of hospital stay, and potentially have a financial consequence. Undertaking an assessment prior to insertion of a cannula, and during its insertion, aids the process and reduces the risks (see below).
Indications
There are a number of potential occasions when a PIC may be required:
Assessment prior to PIC insertion
Prior to PIC insertion it is appropriate to assess:
Choice of site
Correct choice of site considers:
■ areas with compromised circulation or sensation, oedema or fracture
■ joints, valves in the vein (seen as bulges), bone, ligaments, muscle, nerves or tendons
■ arteries, particularly those that run in unexpected directions.
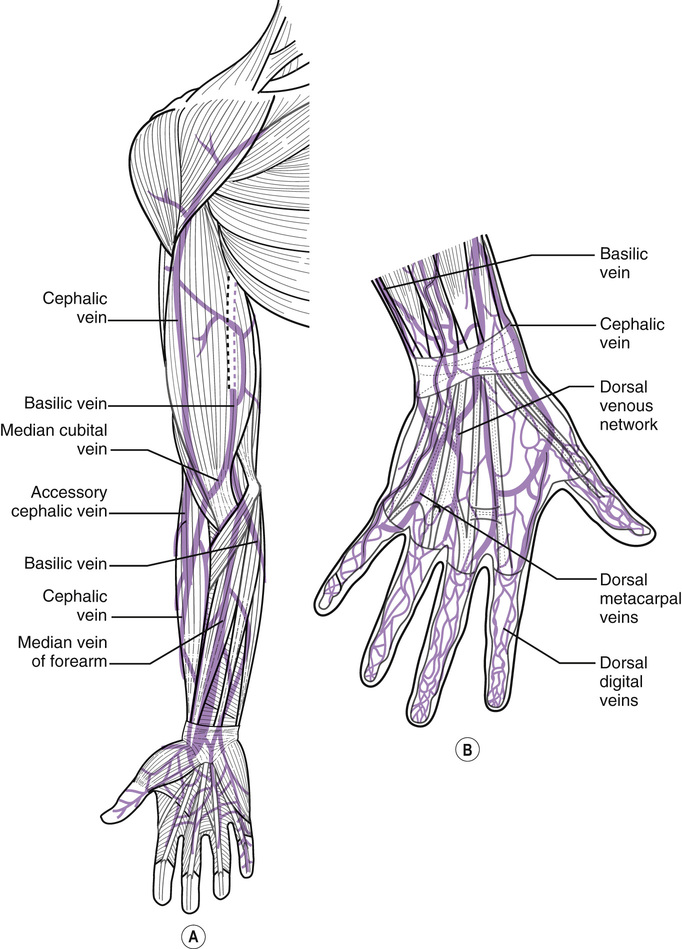
■ a vein in good condition (often described as ‘bouncy’ (Dougherty 2011)) that can be palpated in the lower half of the arm, e.g. dorsal venous network (back of the hand) and cephalic and basilic veins of the forearm (Fig. 47.1).
Preparation
Venous access is improved if the practitioner and woman are relaxed and if certain physical measures are undertaken. A tourniquet (ideally disposable) should be placed 7–8 cm above the chosen site, heat may be applied (heat pack or warm water), gravity or vein filling may be utilized (clenching/unclenching fist) and gentle stroking of the vein may increase its prominence (Brooks 2014). Topical analgesia can be prescribed in some situations, particularly if the woman requests it, or if a large bore cannula is being inserted. It may take 30 minutes to 1 hour to take effect. A small amount of local anaesthetic such as lidocaine (lignocaine) may be injected intradermally (see Chapter 20) at the proposed puncture site. This needs only 3–5 minutes to take effect. This is often agreed locally under a Patient Group Directive (PGD) (see Chapter 18).
Asepsis and use of standard precautions
The RCN (2010) are clear that infection control measures are very important for the insertion and ongoing care of PICs. The Aseptic Non Touch Technique (ANTT) approach (Rowley & Clare 2011) has a specific standard for cannulation (www.antt.co.uk), using a non touch technique for all Key-Parts and Key-Sites and a general aseptic field with the use of Micro Critical Aseptic Fields. (see Chapter 10). All equipment should be sterile and for single use only; a sterile dressing pack is used, as is appropriate personal protective equipment (PPE), e.g. a plastic apron and non-sterile gloves. All sharps should be disposed of at the point of use in a portable sharps box. If continual use of a PIC is needed, it should be renewed after 72–96 hours (RCN 2010), or sooner if no longer required, or if complications are suspected.
Skin cleansing (Key-Site) should be undertaken using the locally agreed wipes/solution, often 70% alcohol with 2% chlorhexidine (Loveday et al. 2014). Friction is generated using the up-and-down, right-to-left approach, cleansing for at least 30 seconds. The skin should then air dry for at least 30 seconds, the vein should not be repalpated once the skin has been cleansed. If repalpation is necessary, sterile gloves should be worn.
Choice of equipment
In the UK, cannulae are colour-coded according to size, the size is both the gauge and the length, and it determines the flow rate per minute. The one chosen should suit the site and the fluid to be infused. The smallest possible that is appropriate should be chosen, as this improves patient comfort (RCN 2010). A larger bore cannula – 16 g (grey) or 14 g (brown) – is often chosen for the childbearing woman in an emergency.
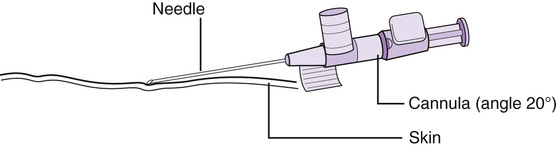
Cannulae may vary slightly according to the manufacturer, but generally consist of a polyurethane piece of tubing with a hub, in which there is a bevelled needle (stylet), also with a hub. Wings may be attached for ease of securing the cannula and there may or may not be a needleless injection port (Fig. 47.2). Once inserted, a closed system is maintained. Any extension tubing or needleless hubs are added and used in an ANTT way. A transparent polyurethane dressing helps the cannula to stay in place, allows for observation of the site, permits the woman to bathe, but does take skill to apply correctly (Lavery & Ingram 2006). A poorly dressed cannula increases the risks of leaking, extravasation, infection, air embolism and trauma; this is unacceptable (Moureau 2013). Whichever type of dressing is used, it should be assessed every 24 hours and if contaminated or peeling, changed (RCN 2010). Otherwise it may be left in place for 48 hours.