48. Principles of phlebotomy and intravenous therapy
intravenous infusion
CHAPTER CONTENTS
Definition327
Indications328
Checking the infusion solution prior to administration329
Calculating the flow rate of the intravenous fluid330
Changing the administration set330
Changing the intravenous solution331
Ongoing care of the intravenous infusion331
Monitoring fluid balance331
Role and responsibilities of the midwife332
Summary332
Self-assessment exercises332
References332
LEARNING OUTCOMES
Having read this chapter the reader should be able to:
• discuss the indications for an intravenous infusion
• describe the different types of fluid solution commonly used for an intravenous infusion
• describe the formula for calculating the flow of an intravenous infusion
• discuss the midwife’s role and responsibilities in relation to intravenous infusion therapy
• discuss how fluid balance is monitored and the significance of this.
This chapter focuses on the skills involved with the setting up, monitoring and discontinuation of an intravenous infusion, including reference to the types of solution commonly used and the monitoring of fluid balance. These are skills primarily used in the hospital setting for the childbearing woman and the baby. For the woman, having an intravenous infusion in progress can be debilitating, affecting her mobility and independence. She may require assistance in caring for herself and for her baby. It can also alter her body image. There are associated risks with intravenous infusion therapy, ranging from phlebitis to death (Scales 2008).
Definition
An intravenous infusion is the introduction of sterile fluid into the blood circulation. When intravenous therapy is expected to be short term, access to the circulation is usually via the veins of the back of the hand, wrist or lower arm. If intravenous therapy is expected to be long term, lasting several days or weeks, the subclavian vein or internal jugular vein is the usual site of cannulation. The latter is rarely used in midwifery. Prior to commencing an intravenous infusion, cannulation is required (see Chapter 47). Due to the risk of infection it is important to use a non-touch technique throughout.
Indications
• Hypovolaemia, e.g. haemorrhage, shock, dehydration.
• Administration of drugs, e.g. Syntocinon.
Equipment
Intravenous administration set
These are sterile prepacked sets consisting of a long piece of tubing with a drip chamber and trocar at the top end and a nozzle at the bottom end that connects to a cannula. Around the tubing is an adjustable roller clamp that alters the flow of fluid (Fig. 48.1); this should be positioned on the upper third of the tubing. It is important to reposition the clamp from time to time to prevent the tubing from kinking as it may then attempt to straighten out pushing the clamp open (Sarpal 2008). There are two main types used in midwifery – one for the administration of clear fluids and one for blood transfusion, the latter having a double chamber and a filter.
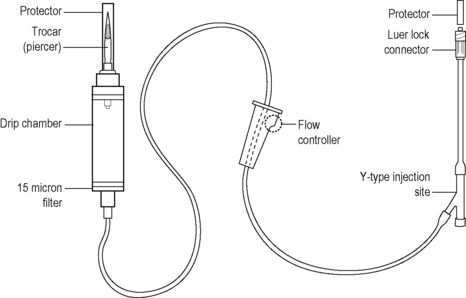 |
| Figure 48.1 • An intravenous administration set (Adapted with kind permission from Jamieson et al 2002) |
Burette sets or volume control devices are used when an infusion pump is unavailable, to obtain greater control over the flow rate. The drip chamber is calibrated, with a clamp above and below the chamber, and is filled with the amount of fluid to be infused during 1 hour. The flow rate is calculated according to the drop factor (varies according to manufacturer’s instructions) and the amount prescribed. It will require refilling each hour. As it limits the amount of fluid transfused, it reduces the risk of the woman receiving too much fluid too quickly.
The use of a closed system of infusion will reduce the risk of infection; with each connection that is added to the infusion line, the infection risk increases (Dougherty et al., 2008 and NPSA (National Patient Safety Agency), 2007). For example, three-way taps used between the cannula and infusion line are difficult to keep clean and can act as a reservoir for microorganisms, which multiply in the warm, moist environment, increasing the risk of infection (Dougherty et al 2008).
Infusion pumps
A variety of infusion pumps are available that adjust the infusion flow electronically, administering a prescribed amount of fluid over a set time. The midwife should know how the infusion pump works and ensure it is properly cleaned and maintained.
Syringe pumps
Syringe pumps may also be used for the administration of drugs (e.g. insulin) and are useful when a small volume of a highly concentrated drug is required (see Chapter 23).
Volumetric pumps
Volumetric pumps can accurately measure the volume of fluid to be infused; different pumps may require different administration sets.
Intravenous fluid
Intravenous fluid can be one of a variety of solutions (Table 48.1) with different types of containers used, for example, soft plastic bag, glass bottle, semi-rigid plastic (polyfusor). Glass containers have a rubber bung covered by a sterile seal that is removed and wiped with an alcohol-impregnated swab just prior to insertion of the trocar from the top end of the infusion set. To facilitate flow of the fluid, a sterile air inlet needle is inserted through the rubber bung to equalise the pressure within the bottle. Sterile scissors should be used with the semi-rigid container to cut off the end of the entry conduit. The trocar is inserted into this tube and twisted to ensure a good fit. Soft bags have an end that is twisted off or has two flaps that are pulled apart and the trocar inserted as for the semi-rigid container. Soft and semi-rigid containers do not require venting.
| Solution | Example | Indication for use |
|---|---|---|
| Crystalloid: isotonic solutions (same tonicity as blood) | 0.9% sodium chloride | To compensate for fluid loss from diarrhoea and vomiting by expanding the circulating volume |
| 5% dextrose | ||
| Crystalloid: hypotonic solutions (lower particle concentration than plasma) | 0.45% sodium chloride | To compensate for fluid loss by moving fluid into intracellular spaces Used if sodium intake restricted |
| Crystalloid: hypertonic solutions (higher tonicity than plasma) | 20% dextrose |



