47. Principles of phlebotomy and intravenous therapy
intravenous cannulation
CHAPTER CONTENTS
Considerations for the childbearing woman321
Indications322
Asepsis and use of standard precautions322
Choice of equipment322
Documentation324
Ongoing care324
Role and responsibilities of the midwife326
Summary326
Self-assessment exercises326
References326
LEARNING OUTCOMES
Having read this chapter the reader should be able to:
• discuss the indications for cannulation
• describe how the site is selected and the equipment chosen
• describe a safe cannulation technique
• describe the correct removal of an intravenous cannula
• summarise the role and responsibilities of the midwife.
As one of the vascular access devices, peripheral intravenous cannulae (PIC) are commonly sited and utilised in midwifery care. A peripheral cannula is sited into a vein for the purposes of infusing fluids or administering medicines via the intravenous route. Performing the skill requires training, supervised practice and ongoing maintenance of the skill. Depending on local protocol, cannula insertion is often only undertaken by qualified staff. PICs feature highly in the nursing and midwifery literature partly because of the risks of localised and systemic infection from their incorrect insertion, use or removal. This chapter reviews the skills of siting and removing a PIC, along with the role and responsibilities of the midwife.
Considerations for the childbearing woman
The additional blood volume in pregnancy and higher body temperature usually mean that the veins are prominent and are therefore easier to gain access to. PICs should only be inserted when there is a clinical indication, and it should be removed as soon as that aspect of care is completed. Undertaking an assessment prior to insertion of a cannula aids the process and reduces the risks. This includes assessment of the woman – previous experiences, age, health, informed consent, suitable site, known allergies – as well as considerations regarding the nature of the medication to be administered and for how long (Lavery & Smith 2007).
Indications
• Administration of whole blood or blood products.
• For drugs requiring IV administration.
• In preparation for a potential complication or operative delivery, e.g. caesarean section, previous caesarean section in labour aiming for vaginal delivery, multiple or breech birth.
• Administration of patient-controlled analgesia.
• Fluid administration with epidural analgesia.
Choice of site
Correct choice of site considers:
• Structures to avoid:
○ the dominant arm
○ areas that are painful, bruised, tortuous, thrombosed, inflamed or with existing skin infection, e.g. eczema
○ areas with compromised circulation, oedema or fracture
○ joints, valves in the vein (seen as bulges), bone, ligaments, muscle, nerves or tendons
○ arteries, particularly those that run in unexpected directions.
• Try to choose:
○ a vein (identified by its lack of pulse and the ability to empty and fill by occluding and releasing it digitally)
○ a vein in good condition (often described as bouncy (Dougherty 2008a), that can be palpated in the lower half of the arm, e.g. dorsal venous network (back of the hand) and cephalic and basilic veins of the forearm (Fig. 47.1).
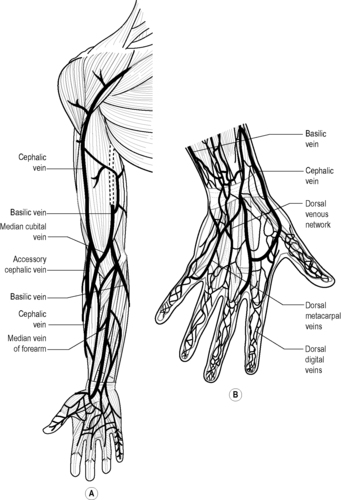 |
| Figure 47.1 • A Veins of the forearm. B Veins of the hand (Adapted with kind permission from Williams 1995) |
Preparation
Venous access is improved if the practitioner and woman are relaxed and if certain physical measures are undertaken. A tourniquet should be placed 7–8 cm above the chosen site, heat may be applied (heat pack or warm water), gravity or vein filling may be utilised (clenching/unclenching fist) and gentle tapping or stroking the vein may increase its prominence (Dougherty 2008a). If indicated, topical analgesia may be used, but (depending on type chosen) needs 1–2 hours to be effective. A small amount of local anaesthetic such as lidocaine may be injected intradermally (see Chapter 20) at the proposed puncture site. This needs only 3–5 minutes to take effect.
Asepsis and use of standard precautions
Strict asepsis is indicated for the insertion and ongoing use of a peripheral intravenous cannula. All equipment should be sterile and for single use only, a sterile dressing pack and sterile gloves are used. Other personal protective equipment (PPE) includes the use of an apron. All sharps should be disposed of at the point of use in a portable sharps box. If continual use of a PIC is needed it should be renewed after 72–96 hours.
Skin cleansing should be undertaken using either 2% chlorhexidine or 70% alcohol (Dougherty 2008a). Gentle friction is necessary for at least 30 seconds, in a circular motion from centre to periphery. A rapid ‘one wipe’ of the skin merely disturbs the skin flora. The skin should then air dry for up to 1 minute, the vein should not be repalpated once the skin has been cleansed.
Choice of equipment
A cannula should be a suitable size for both the vein and the fluid that is to be infused. A large bore cannula should be used for the childbearing woman: sizes 14 or 16 gauge.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


