Principles of intrapartum skills
Examination of the placenta
Learning outcomes
Having read this chapter, the reader should be able to:
• describe the appearance and structure of the term placenta
• describe the examination of the placenta and the significance of the information obtained
• discuss how the midwife can obtain cord blood samples
• discuss the role and responsibilities of the midwife in relation to examining the placenta.
Examination of the placenta following delivery is an important skill undertaken by the midwife to reduce the occurrence of both postpartum haemorrhage (PPH) and infection. This chapter begins with a description of the appearance and structure of the placenta, discussing the significance of deviations and the procedure for undertaking examination of the placenta, followed by a discussion around obtaining cord blood samples. It concludes with a brief discussion concerning disposal of the placenta. Obtaining blood for cord blood banking is not discussed.
Appearance and structure
The placenta is a disc-shaped structure with different appearances to the maternal and fetal surfaces. Whilst around 90% of placentae are round-to-oval in shape, the remaining 10% have an abnormal appearance, e.g. bipartite, succenturiate lobe (Baergen 2011). Hargitai et al (2004) suggest an abnormal placental shape is associated with a placenta that underwent disturbed implantation or with a uterine abnormality. The term placenta weighs approximately 500–600 g. Ryan et al (2011) suggest the baby should weigh 7–8 times the weight of the placenta. It has a mean diameter of 22 cm and thickness of 2.5 cm (Baergen 2011). A thicker diameter may be associated with diabetes, macrosomia and hydrops, whereas a thinner placenta can be associated with intrauterine growth restriction (IUGR). The placenta will be heavier if early cord clamping is used and lighter with delayed cord clamping (DCC) due to the transfusion of blood from the placenta to the baby at delivery. A larger placenta may be associated with maternal diabetes, fetal infections and multiple pregnancy and a smaller placenta with chronic IUGR and placental insufficiency. The placenta should not have an offensive smell – this is associated with intrauterine infection.
A circumvallate placenta is a rare abnormal development of the placenta resulting in an abnormal structure and appearance. This occurs because the placenta enlarges underneath the surface of the endometrium and the embryonic sac grows above it, resulting in the endometrium between them being compressed and obliterated. This results in the formation of an acellular membrane which can affect the placental attachment to the decidua and increase the risk of placental abruption. Hargitai et al (2004) question whether a circumvallate placenta is significant but advise it may be associated with IUGR and both acute and chronic maternal haemorrhage. When examining the placenta, there will be a thick grey/white raised ring around the central part of the fetal surface which is a result of the fetal membranes folding back on themselves.
Fetal surface of the placenta
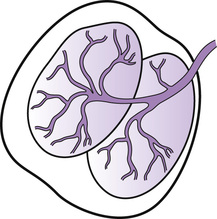
The amnion, covering the fetal surface of the placenta and the chorionic plate (a thin membrane continuous with the chorion), creates a white shiny appearance to the fetal surface of the placenta. If the baby passed meconium in utero it may be seen on the fetal surface. Underneath the surface layer are 50–60 lobes (cotyledons) which are further divided into 1–5 lobules. These usually present as one unified group but occasionally a placenta is divided into two (bipartite) or three (tripartite) separate, distinct lobes, each having its own section of umbilical cord inserted into it. The cord presents as one cord until it is close to the placental surface where it divides to supply each lobe (Fig. 33.1).
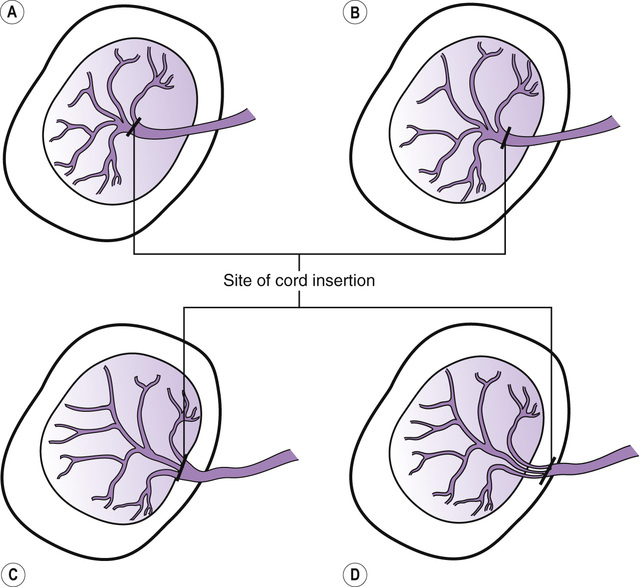
Inspection of the fetal surface will show arteries and veins beneath the amnion spreading outwards from the point of cord insertion with the arteries crossing over the veins. The cord is usually inserted centrally or slightly off centre (Fig. 33.2A, B). A ‘battledore’ or marginal insertion refers to the cord that is inserted at the edge of the placenta (Fig. 33.2C); this is usually insignificant but may have a more fragile attachment, which can increase the risk of cord avulsion during controlled cord traction (CCT). Occasionally the cord is inserted into the membranes – a ‘velamentous’ insertion (Fig. 33.2D) – with blood vessels running from the cord through the membranes to the placental surface. In this situation the attachment of the cord can be very fragile, resulting in an increased incidence of cord avulsion during CCT. Rarely the blood vessels can lie over the cervix (vasa praevia) and have a risk of rupturing during spontaneous or artificial rupture of the membranes, resulting in massive fetal haemorrhage. A furcate cord is one that divides prior to insertion regardless of the site of insertion.
The umbilical cord
The cord contains the umbilical vein that carries oxygenated blood to the fetus and two smaller umbilical arteries that bring the deoxygenated blood from the fetus to the placenta. The blood vessels are surrounded by Wharton’s jelly, which helps protect them, and are covered by the amnion. A cord with less than three vessels can be associated with a congenital abnormality and the baby should be referred to the paediatrician for review. A small portion of the cord may also be required for analysis. When examining the cord for the presence of three vessels the vein is the larger vessel with the two smaller vessels being the arteries. If the cut end of the cord has been squashed, it can be difficult to locate the vessels – cut off a small portion of the cord to make counting the vessels easier.
The average umbilical cord is 40–70 cm long, less than 40 cm is a short cord and longer than 70 cm is a long cord (Baergen 2011), although Hargitai et al (2004) suggest this should be longer than 100 cm. A short cord is usually insignificant, although if it is very short, the cord will be pulled taut as the fetus descends through the pelvis, which can lead to an abnormal fetal heart rate pattern. There is a risk of a long cord wrapping around the fetus or becoming knotted, resulting in occlusion of the vessels. There is also an increased risk of cord presentation and prolapse, particularly if the presenting part is poorly applied to the cervix, e.g. with a malposition or malpresentation. The cord is 1–2 cm wide – a thicker cord is associated with diabetes, macrosomia, and hydrops and may be difficult to secure prior to clamping, whereas a thinner cord is associated with IUGR (Baergen 2011). The cord is twisted in a spiral with one coil every 5 cm which provides some protection to the vessels from pressure and has enhanced capacity to withstand kinking, compression, and torsion. False knots may be noted in the cord and can occur when the blood vessels are longer than the cord, forming a loop in the Wharton’s jelly.
The fetal membranes
Two membranes surround the fetus and form the amniotic sac – the amnion and chorion. These can appear to be fused but are not and can be separated by stripping one from the other. The amnion covers the cord and fetal surface of the placenta and is the inner lining of the amniotic sac; it is smooth, tough, and translucent. The chorion begins at the placental edge and extends around the decidua and is thick, friable, and opaque. Following delivery the membranes will have a hole in them through which the baby has been born. They should be carefully examined as a piece of membrane may be retained in utero and is likely to give the appearance of ragged membranes. Even a small fragment of retained membrane can result in uterine atony and PPH or be a site for microorganisms to grow, predisposing to infection. Pieces of membrane may be found in clots passed post-partum, hence the need to examine postpartum clots for the presence of membranes, particularly when the membranes were ragged.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree