34. Principles of intrapartum skills
perineal repair
CHAPTER CONTENTS
The pelvic floor241
Aims of perineal repair242
Perineal suturing244
Effective analgesia for the woman 244
Asepsis and standard precautions 245
Alignment of the tissues to encourage granulation and healing 245
Cessation of haemorrhage 245
Reduction of any dead space 245
Minimal amount of suture material 245
Infiltration of the perineum for repair 245
Using a needle holder 246
Record keeping251
Role and responsibilities of the midwife251
Summary251
Self-assessment exercises251
References252
LEARNING OUTCOMES
Having read this chapter the reader should be able to:
• state the aims of perineal repair
• discuss the role and responsibilities of the midwife when undertaking perineal repair
• discuss the current evidence for the choice of materials and the technique used
• describe how to infiltrate the perineum
• demonstrate tying a knot, continuous non-locked and subcuticular sutures
• list the factors that should be included with record keeping.
Perineal trauma of some kind is estimated to occur in up to 85% of vaginal deliveries in the UK, with 69% requiring suturing (Kettle et al 2002); perineal repair is associated with short-term discomfort and/or pain and 20% of women experience long-term problems such as dyspareunia (Kettle et al 2007). This chapter examines the procedure, technique and materials used for perineal repair; the anatomy of the pelvic floor is reviewed and the significance of correct perineal repair is highlighted. The reader is encouraged to read widely in other literary sources to appreciate the associated issues (e.g. prevention of perineal trauma, postnatal perineal care).
The pelvic floor
As a hammock-shaped arrangement of muscles and fascia, the pelvic floor is the supportive structure in the woman’s pelvis. The muscles are arranged in two layers, deep and superficial (Fig. 34.1) extending to and from landmarks in the pelvis, encircling other structures (e.g. the vagina) and forming the perineal body. The perineal body is triangular in shape and comprises skin, two superficial muscles (bulbocavernosus and transverse perineal) and one deep muscle (pubococcygeus). It lies between the anus and vagina and is flattened and displaced as the baby is born. The pelvic floor prevents the pelvic organs from prolapsing and is an important component in the correct functioning of the vagina, bladder, uterus and rectum; a damaged or weakened pelvic floor may cause long-term urinary, faecal or sexual morbidity.
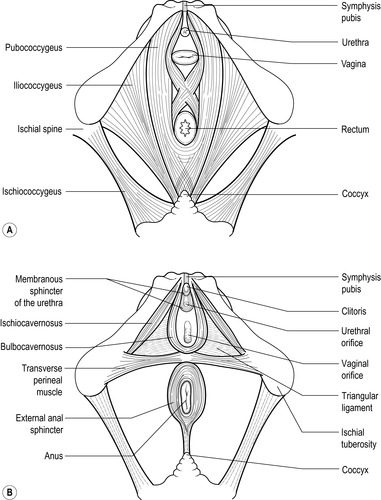 |
| Figure 34.1 • A Deep muscle layer of the pelvic floor. B Superficial muscle layer of the pelvic floor |
Aims of perineal repair
Repairing perineal trauma aims to ensure that the tissues are correctly realigned, haemorrhage is stemmed and dead space (into which bleeding may occur) is reduced. The overall aim is to maintain the integrity of the woman’s pelvic floor.
On examining the genital tract immediately postdelivery, the extent of perineal damage is noted and decisions are made as to:
• if so, using which materials
• by whom
• in which environment.
Definitions of perineal trauma are based around the structures involved; note that no classification is currently made as to the size of the injury. It may have occurred naturally or be a result of incision (episiotomy). The accepted definitions are:
• first degree: affects skin only
• second degree (tear or episiotomy): affects the skin, posterior vaginal wall and superficial muscle (occasionally deep muscle is affected)
• third degree: affects the same structures as a second degree as well as the anal sphincter and are further classified as:
○ 3a <50% of external anal sphincter torn
○ 3b >50% of external anal sphincter torn
○ 3c injury to both the external and internal anal sphincter
• fourth degree: affects the perineum (as above) and the anal sphincter complex and epithelium (NICE 2007).
However, damage can occur to any part of the pelvic floor, perineal body or vulval tissue, including the vagina and/or labia. Careful examination of the labia is required to determine if the clitoris or urethra have been damaged.
Suturing is the most likely means of repair; there has been some speculative research into the use of tissue adhesive (Adoni and Anteby, 1991 and Rogerson et al., 2000) but there is little evidence this is preferable to suturing, with further research and development required (Royal College of Midwives (RCM), 2008 and Viswanathan et al., 2005). The skill of the operator is paramount; midwives can provide good continuity of care for the woman, but care needs to be evidence based, with training and updating and within one’s capabilities. Hesitations about the task in hand, for whatever reason, should cause the midwife to refer to an experienced midwife or obstetrician. The health and wellbeing of the woman may be seriously affected in both the short and long term if the repair is poorly completed (Sleep et al 1984). Extensive perineal damage or third- or fourth-degree injury requires repair by a senior obstetrician in theatre with additional analgesia (general or regional anaesthesia). If the urethra is involved, the repair may need to be undertaken by a genitourinary specialist. Bilateral labial grazes that would be in apposition when standing or sitting should also be sutured so that the labia do not heal together. Arkin & Chern-Hughes (2001) cite a case study in which the labia needed surgically parting some months following abrasions in childbirth. If the woman declines suturing of bilateral labial tears, she should be advised about the risks and encouraged to part her labia daily to reduce the likelihood of fusion. Perineal repair can be undertaken in the home if adaptations are made to accommodate suitable positioning of the woman and midwife (with good light). If the repair is extensive, however, the midwife may consider transfer to a hospital environment.
Current evidence
Draper & Newell (1996) suggest that failure to adhere to evidence-based practice with perineal repair may have wide-ranging consequences in women’s lives. The body of research is now extensive (but still increasing) and therefore there is little excuse for diversity in practice. Kenyon & Ford (2004) discuss the process and implementation of an evidence-based accepted protocol in their maternity unit.
To suture or not to suture?
NICE (2007) recommends that first-degree tears where the wound is not in apposition and all second-degree tears should be sutured, although not all women will consent to the procedure. Kenyon & Ford (2004) agree, indicating that the existing studies are small and therefore unreliable and that, at this time, suturing of the vaginal wall and muscle layers is indicated. McCandlish (2001) also suggests that it is time to seek the evidence, but not to change practice until reliable evidence exists.
The midwife should discuss the rationale for suturing, with the advantages and disadvantages, to allow the woman to make a more informed choice. The advantages of suturing include quicker initial healing of the tissues with better wound alignment compared with not suturing (Fleming et al., 2003, Langley et al., 2006 and Leeman et al., 2007) and reduced urinary problems (Metcalfe et al 2006) although the RCM (2008) suggests that studies on non-suturing have yielded conflicting results and agree with Metcalfe et al (2006) that further research is required. However, suturing can be a painful procedure in itself, may require the use of lithotomy, which can be difficult for some women (e.g. those with pelvic girdle pain) and may result in increased use of analgesia (Langley et al., 2006 and Leeman et al., 2007). Metcalfe et al (2006) found reported levels of perineal pain were similar between sutured and unsutured women.
The skin, following the Ipswich Trial (Gordon et al 1998), may be left unsutured providing that the skin edges are in apposition with a gap no greater than 0.5 cm. This is considered to reduce dyspareunia at 3 months postpartum, but with no differences in short- or long-term perineal pain. However, Grant et al (2001) found that 1 year later there were no differences in relation to the amount of discomfort or pain experienced, dyspareunia and the time in which sexual intercourse was resumed; the RCM (2008) conclude that there appears to be neither benefit nor disadvantage in relation to suturing or not suturing the skin. Viswanathan et al (2005) advise that it is preferable to leave both the superficial vaginal and perineal skin unsutured.
Choice of material
Fast-absorbing polyglactin sutures are currently considered to be the suture material of choice when compared to chromic catgut and other absorbable sutures as they are associated with less perineal pain, a reduced need for analgesia, less uterine cramping at 24–48 hours and at 6–8 weeks, a significant reduction in the need for suture removal, fewer healing problems in the short term and earlier resumption of sexual activity (Greenberg et al., 2004, Kettle et al., 2007, Leroux and Bujold, 2006 and Viswanathan et al., 2005). Size 2/0 is indicated for perineal tissue.
Instruments
There is little mention of instruments, except that Bott (1999) recommends that midwives should learn to suture with instruments (needle holder and tissue forceps) rather than fingers, to reduce the risk of injury to the midwife and possible transfer of HIV. The Department of Health (DH 1998) also recommends the use of blunt-ended needles for suturing to reduce these risks further; the American College of Surgeons also support the use of blunt-ended needles when suturing muscle to reduce the risk of needlestick injury (ACS 2007). However, Wilson et al (2008) found no difference in the rate of surgical glove perforation between blunt and sharp needles during perineal repair but the use of blunt needles increased the difficulty of perineal repair.
Technique
Perineal repair is often completed in three stages:
1. posterior vaginal wall
2. perineal muscle layer
3. perineal skin.
The use of a loose continuous suture is currently recommended for all three layers as it results in less short-term pain than interrupted or locked sutures (Kettle et al 2007). Whilst a continuous locked suture has been used to repair the vagina in the past – this was thought to prevent concertinaing of the vaginal wall if the continuous non-locked suture were pulled too tight (Enkin et al 2000) – there have been no randomised controlled trials to confirm this (Kettle et al 2007). Indeed, Kettle et al (2007) agree that tight stitches can restrict the distribution of tissue resulting in increased pain and propose the use of a loose continuous suture as it enables the tension to be transferred throughout the length of the whole stitch thereby reducing pain.
The current evidence may be summarised as:
• if indicated, a perineal wound should be sutured throughout using a rapidly absorbing polyglactin suture, e.g. Vicryl Rapide®, with a loose continuous unlocked suture to the posterior vaginal wall and muscle layer, bringing the skin into good apposition
• if skin closure is indicated, a continuous subcuticular technique should be used
• for good practice (not evidence based) the midwife should consider standard precautions and use instruments to suture with and if possible blunt-ended needles.
Perineal suturing
A successful perineal repair incorporates all of the following principles:
Effective analgesia for the woman
Get Clinical Tree app for offline access



