30. Principles of intrapartum skills
first-stage issues
CHAPTER CONTENTS
Role and responsibilities of the midwife210
Summary210
Self-assessment exercises210
References211
The first stage of labour is divided into two phases: latent and established. The National Institute for Health and Clinical Excellence (NICE 2007) defines the latent phase as the time when painful contractions occur with some cervical change, including effacement and dilatation up to 4 cm. Labour is established when the contractions are regular and painful and are accompanied by progressive cervical dilatation.
This chapter focuses on a selection of the skills used when caring for a woman during the first stage of labour; it is acknowledged that these skills may also be employed during the second stage of labour. In particular, this chapter addresses the skills of examination per vaginam during labour, commonly referred to as a vaginal examination (VE). This is an essential skill for the midwife when caring for a labouring woman, one that should be undertaken sensitively due to the intimate nature of the examination, but efficiently as the information gained will help assess progress and inform care. The procedure is invasive and considered a medical intervention, thus it should only be undertaken when necessary (Mandaza & Nolan 2001). The procedures for performing amniotomy and applying a fetal scalp electrode are also described. The chapter concludes with a discussion on different positions that may be adopted by the woman during the first stage of labour.
Examination per vaginam
Indications
An examination per vaginam is an intimate procedure that should be undertaken only when there is a clear clinical indication. Levin et al (2005) found that women experience an average of three VEs during labour; some women will have more than this. NICE (2007) advise that the midwife (and doctor) should be sure that it is absolutely necessary and that the findings will provide important information to the decision making process; they advise that for women in normal labour the frequency of the examination should be every 4 hours, although this may be considered as too frequent by some women and midwives who will undertake the examination only when clinically indicated.
Women can find this procedure very distressing and it is important that the procedure is discussed with the woman prior to undertaking the procedure. This discussion should include: the rationale for the procedure, what will happen, what is expected of the woman and confirmation that the procedure can be stopped at any point if requested by the woman. This discussion should be undertaken in a manner that allows the woman to ask questions and also to refuse the examination. During the examination itself, it is important to maintain both verbal and non-verbal communication with the woman, recognising when she is experiencing discomfort/pain and requires the procedure to end and providing her with information (Stewart 2005). Levin et al (2005) found that only 70% of women recalled having the subject of VE discussed with them before the procedure although 95% considered they were well informed of the findings. Only 40% felt they could refuse the examination and sadly 22.2% considered that their permission was not sought.
During labour, the midwife may undertake a VE to:
• confirm the onset of labour
• assess progress during labour
• identify the presentation and position
• perform an artificial rupture of membranes
• apply a fetal scalp electrode
• exclude cord prolapse following spontaneous rupture of the membranes where there is an ill-fitting presenting part
• confirm the onset of the second stage of labour, especially with a breech presentation and multiple pregnancy.
Contraindications
The midwife should not undertake a VE when there is:
• bleeding
• placenta praevia
• preterm rupture of the membranes
• preterm labour (the initial VE should be undertaken by the obstetrician; the midwife may perform subsequent examinations)
• no consent from the woman.
Information gained from undertaking an examination per vaginam
External genitalia
Any abnormalities such as varicosities, oedema, warts or signs of infection should be noted, as should scarring, particularly if indicative of previous perineal or labial trauma or female genital mutilation; NICE (2007) warns that a VE may be very difficult in the presence of fibulated genital mutilation. The colour, consistency, amount and odour of any discharge or bleeding from the vagina should be recorded; amniotic fluid may be seen if the membranes have ruptured.
Cervix
The cervix is assessed for position, consistency, effacement, dilatation and application to the presenting part. Prior to labour, the cervix is usually in a central or posterior position, firm, non-effaced with the os closed (unripe). In the latter weeks of pregnancy and early labour, the structure and position of the cervix alters as the cervix ripens, resulting in a cervix that feels less rigid and in an anterior position. A ripe cervix that feels soft and stretchy is associated with good dilatation of the os uteri, whereas a tight unyielding unripe cervix at term is more likely to be associated with prolonged labour. An unripe cervix requires three to four times more uterine effort than a ripe cervix (Burnhill et al 1962).
A cervix that is well applied to the presenting part is associated with good uterine activity (Blackburn 2007). The reverse may be true, that a poorly applied cervix is associated with less efficient uterine activity and slower progress. For example, when the fetus is in an occipitoposterior position, the head is not pushed directly onto the cervix; rather it is directed downwards and forwards against the back of the symphysis pubis, leading to a decrease in the effectiveness of uterine contractility, slower cervical dilatation and prolonged labour (Chamberlain 1993). The application of the cervix to the presenting part can be assessed by feeling between them.
Effacement usually precedes dilatation with the primigravida; these may appear to occur simultaneously with the multigravida. Effacement is assessed by the length of the cervix and the degree to which it protrudes into the vagina. A non-effaced cervix feels long and tubular, with the os closed or partly dilated. As effacement occurs, the cervix thins out and feels shorter, as the lower uterine segment takes it up (Fig. 30.1). A fully effaced cervix feels continuous with the lower uterine segment and does not protrude into the vagina.
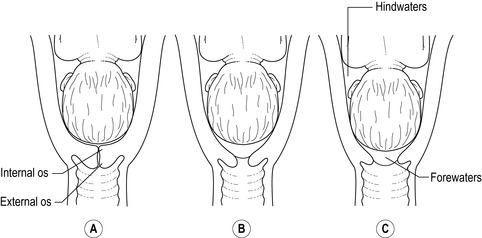 |
| Figure 30.1 • Effacement of the cervix |
Dilatation of the os uteri is measured in centimetres and is assessed by inserting one or both fingers through the external os and parting the fingers to assess the diameter. In early labour, when the cervix is less than 2 cm dilated, usually only one finger can be inserted. Towards the end of the first stage it may be easier to feel around the remaining rim of cervix to estimate dilatation; for example, a rim of 1 cm equates to a dilatation of 8 cm, as there is 2 cm of cervix remaining. When the cervix can no longer be felt, full dilatation has occurred, equal to 10 cm. This is the point at which the fetal head can pass through the cervix although for the preterm fetus, this may be less than 10 cm. If the presentation is breech, it is possible for the foot and leg to protrude through the cervix before it is fully dilated (footling breech). Dilatation of the os uteri should occur progressively throughout the first stage of labour and is one factor in determining progress (NICE 2007 suggest this to be 0.5 cm or more per hour).
The os uteri is usually closed in the primigravida until labour begins, but the os of the multigravida may allow one or two fingers through before labour, commonly referred to as a ‘multips os’.
The membranes
Intact membranes may be felt as a shiny surface over the presenting part. This can be difficult to feel, particularly in early labour or if the forewaters are shallow and the membranes tightly pressed against the presenting part. If the membranes are difficult to feel, it may be mistaken for ruptured membranes. When the presenting part is poorly applied to the cervix, the membranes contain a greater amount of fluid and may bulge through the cervix. As the pressure increases in the forewaters during contractions, the membranes can become tense and may rupture spontaneously. This usually occurs earlier when the presenting part is ill-fitting or poorly applied; for example, with a malposition such as an occipitoposterior position, malpresentation such as face presentation or a high presenting part. If the membranes are felt intact but amniotic fluid is leaking, a hindwater rupture is the likely cause. Pulsation felt beneath the membranes may be indicative of cord presentation or vasa praevia.
Presentation
In conjunction with information gained from the abdominal examination, the identification of landmarks on the presenting part help to confirm the presentation:
• A cephalic presentation is smooth, round and firm, and sutures or fontanelles may be felt. Moulding can be assessed by the degree of overlapping of the bones of the vault. Caput succedaneum may also be felt as a soft or firm mass on the presenting part, which can make the identification of sutures and fontanelles more difficult.
• Both the breech and face presentation feel soft and irregular. The sacrum may be palpable as a hard bone, with the anus close by and the landmarks are felt in a straight line. If a finger is inadvertently inserted into the anus, it will be gripped. Fresh meconium is also likely to be present.
• With the face presentation, the orbital ridges may be felt and a finger inserted into the mouth may be sucked, the landmarks are located in a triangular position. If a face presentation is suspected or confirmed, care should be taken to avoid damaging the eyes; application of a fetal scalp electrode is not recommended and obstetric cream should not be used as it could initiate a chemical conjunctivitis.
• If the cord presents, the pulsations can be palpated through the membranes – the membranes should not be ruptured due to the danger of cord prolapse. If a cord is felt without membranes the emergency procedure for managing cord prolapse should be instigated whilst the examining midwife keeps her fingers in the vagina in an attempt to push the presenting part off the cord.
Level of the presenting part
This is determined by assessing the distance between the presenting part and the ischial spines in centimetres (Fig. 30.2). The ischial spines are referred to as zero station, with the presenting part being above (− cm) or below (+ cm) this. The ischial spines may be difficult to palpate; this becomes a subjective measurement. It is important for the midwife to ensure it is the level of the presenting part being assessed and not caput succedaneum. Descent of the presenting part is one indicator of progress during labour and the assessment should correlate with the findings from the degree of engagement determined during the abdominal examination.
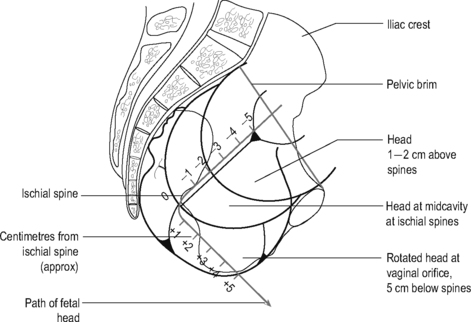 |
| Figure 30.2 • Level of presenting part in relation to the ischial spines |
Position
With a cephalic presentation, identification of sutures and fontanelles will confirm the position and attitude:
• The sagittal suture is easily identified as a long straight suture; its position is taken in relation to the maternal pelvis, moving from back to front.
• A sagittal suture in the right oblique is felt moving from the posterior right quadrant of the maternal pelvis obliquely forwards to the left anterior quadrant (Fig. 30.3) and is indicative of left occipitoanterior position or right occipitoposterior position.
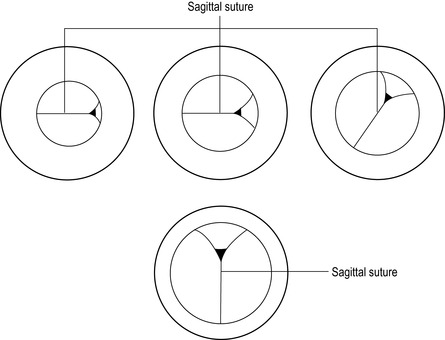 |
| Figure 30.3 • Rotation of a cephalic presentation felt on examination per vaginam
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|