Principles of infection control
Principles of asepsis
Learning outcomes
Having read this chapter, the reader should be able to:
Asepsis – the absence of sepsis or infection – is a critical component of care. Healthcare-associated infections (HCAIs) are costly in monetary and human terms and are often preventable. The risk of litigation is also real (Pratt 2014). Preventing sepsis is a multi-faceted issue, the epic3 guidelines (Loveday et al 2014) place significance on hospital environmental hygiene, hand hygiene, use of personal protective equipment, and the safe use and disposal of sharps, while the Department of Health (2010) also place it within the context of the whole of health care provision, e.g. appropriate prescribing, laboratory and mortuary services, food provision, etc.
It is the principles of asepsis that midwives need to understand in order to then apply them across a range of care situations. This chapter should be read in conjunction with several others including hand hygiene, obtaining swabs, intravenous medicines, epidural analgesia, wound care, etc. This chapter reviews the principles of aseptic practice, particularly with regard to the ANTT (Aseptic Non Touch Technique) framework (Rowley et al 2010).
The ANTT Practice Framework
The ANTT Practice Framework (www.antt.org) (Rowley & Clare 2011a) provides a standardized way in which any Key-Site on the woman can be protected from the introduction of bacteria by using appropriate sterile equipment and fluids. The approach utilizes three strands:
In the UK the DH (2010) require that healthcare providers have a standardized and auditable approach to asepsis management. The ANTT framework has been endorsed by the epic3 guidelines (Loveday et al 2014) and is now widely adopted internationally also (Rowley & Clare 2011a). It moves away from defining terms such as ‘clean’ or ‘sterile’ techniques into recognizing the importance of achievable and well-defined terminology forming a common and meaningful practice language. ANTT is based on a concept of Key-Part and Key-Site Protection for all invasive procedures that involve a risk of infection for the woman. The aim is freedom from infection – asepsis (Rowley et al 2010).
How is it achieved?
A clear differentiation is made between Standard-ANTT and Surgical-ANTT. Surgical-ANTT is typically used in operating theatres, e.g. laminar air flow, surgical hand scrub, full protective gowning, gloving, etc. and uses an extensive and Critically Managed Aseptic Field. However, Surgical-ANTT is also used in other clinical settings for complicated invasive procedures (such as central line insertion). Standard-ANTT generally uses a smaller aseptic field that is managed differently to Surgical-ANTT. It relies more heavily on a non touch technique and therefore may use non-sterile gloves. The practitioner considers their level of competency and the technical difficulty of maintaining asepsis of Key-Parts and Key-Sites. As a rough guide, if a procedure is likely to take 20 minutes or less, be technically simple due to involving few and relatively small Key-Parts and Key-Sites, then Standard-ANTT is used. Not only is this safe, it is more efficient. Examples of this include:
• venepuncture and peripheral cannulation
• childbirth, of whichever mode
• siting of epidural analgesia
If, however, the procedure is more complex, will take longer, or involves larger Key-Sites or many Key-Parts, then Surgical-ANTT is appropriate. Sometimes ANTT-specific risk assessment may determine that a procedure could come into either category due to the competency of the practitioner or the technical difficulty of maintaining Key-Part/Site protection. On occasion, a modified approach may be used, some Standard-ANTT procedures may warrant the introduction of sterile gloves based on this risk assessment, e.g. peripheral cannulation (Rowley et al 2010). However, the emphasis, whichever approach is used, is on the non touching of Key-Sites and Key-Parts (see below). Non touch may refer to the literal non touching of Key-Parts or the necessary (non) touching of Key-Parts by using sterile gloves.
ANTT is built on 10 principles, some of which are summarized above. Others include (Rowley & Clare 2011b):
• Key-Sites are any portal of entry on the woman that could be infected, e.g. any wound, insertion, or puncture site (Rowley & Clare 2011a). If inserting a urinary catheter, for example, the Key-Site is the urethra, if undertaking venepuncture, it is the skin/puncture site. Key-Parts are any items (equipment or fluids) that have direct or indirect contact with the Key-Sites, e.g. the peripheral cannula and the insertion point of any connections into it are both Key-Parts. Thereafter Key-Parts, e.g. needleless ports, should also be disinfected before use. When cleaning an item, e.g. bottle top, needleless port, or sampling port, friction should be generated and scrubbing, with different parts of the wipe, should take place for at least 20 seconds. Key-Sites, e.g. skin cleansing prior to venepuncture, should be cleaned for 30 seconds using the right-to-left and up-and-down approach. The locally approved cleanser is often 70% alcohol/2% chlorhexidine.
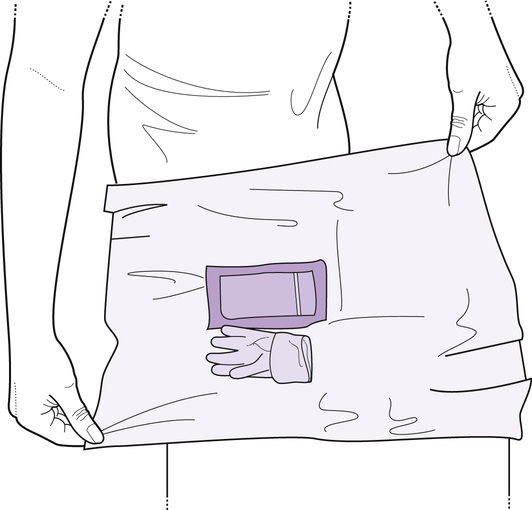
• Establishing an aseptic field. The main aseptic field in Surgical-ANTT is managed ‘critically’. Only sterile equipment must be placed onto it. Its therefore called a Critical Aseptic Field. The main aseptic field in Standard-ANTT is managed ‘generally’, and clean but not necessarily sterile equipment may be placed onto it. It is therefore promoting asepsis. On a General Aseptic Field, Key-Parts are protected by individual caps and covers which are said to be Micro Critical Aseptic Fields. The available equipment, e.g. plastic tray or dressings trolley, is cleansed, with decontaminated hands, using the locally approved cleanser. Sterile items, e.g. dressings pack, are then removed from their outer packaging and placed onto the cleansed area. Care is taken to open the pack using only the corners so that the inside of the pack remains an aseptic field. Other items are then added aseptically to the field. This is shown in Figure 10.1.